 |
History
A 27-year-old female patient reported to the office with a chief complaint of red, itchy eyes for three months. She explained that she had been placed on Pataday (olopatadine hydrochloride ophthalmic solution, Novartis) QD, PRN by her internal medicine doctor but did not get sustained relief. Her ocular history was non-contributory.
Her systemic disease history was positive for rheumatoid arthritis, for which she medicated with Enbrel (etanercept, Amgen) 50mg/week. She denied allergies to medications and foods.
Diagnostic Data
Her best-corrected entering visual acuities were 20/15 OD and 20/15 OS at distance and near. Her external examination was normal with no evidence of afferent pupillary defect. The pertinent biomicroscopic examination of the anterior segment findings are demonstrated in the photo. Goldmann applanation tonometry measured 14mm Hg OU. The dilated fundus examination revealed no peripheral pathologies in either eye.
Discussion
The diagnosis in this issue is vernal keratoconjunctivitis (VKC), or atopic keratoconjunctivits (AKC) with Horner’s Trantas dots. VKC is a chronic mast cell/lymphocyte-mediated allergic inflammatory process of the conjunctiva.1 Clinical symptoms often present as a conjunctival hyperemia, tearing and itching. Photophobia is often present in severe cases.2
VKC is more prevalent in young males, however, cases that arise later in life are equally distributed amongst sexes.1 VKC is a chronic allergic inflammatory reaction mediated by Th2-lymphocytes. There is an overexpression of eosinophils, eosinophilic proteins, growth factors and cytokines.1-5 The reaction is provoked by the warmer seasons of dry, hot climates.
There are three clinical forms of VKC:
1. The palpebral form with giant papillae on tarsal conjunctiva.
2. The limbal form with Horner’s-Tranta’s dots (clumps of necrotic eosinophils, neutrophils and epithelial cells-the active form.
3. A mixed form combining the two described before.1,6,7 According to Zicari and coworkers there is evidence supporting associations between familys that have a history of immunological disorders and higher order ocular signs and symptoms.2
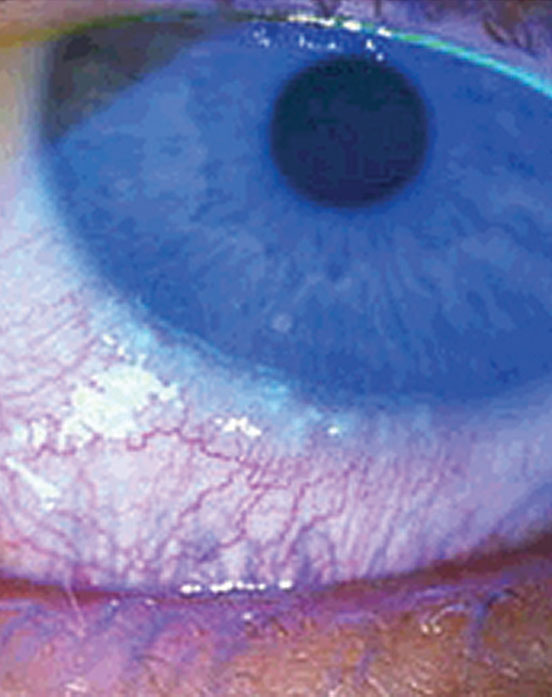 |
This 27-year-old patient’s red, itchy eyes have been causing her trouble for the previous three months. Consider her medical history plus this image to help you uncover the cause behind her discomfort. |
Atopic keratoconjunctivitis (AKC) is another form of ocular chronic allergic inflammatory process which involves the conjunctiva of the eye and eyelid.4 AKC is mediated by Th1- along with Th2-lymphocytes.4 While Th2-lymphocyte is an important mediator in the allergic response, it is the Th1- lymphocytes that have been shown to maintain the low level chronic inflammatory response in these allergic diseases.4
AKC is associated with familial history of eczema and asthma.1 This type of allergic keratoconjunctivitis is more prevalent in individuals over age of 50, however, younger patients are also susceptible.1 AKC is not particulary associated with seasonal changes or climate provocation. AKC ocular clinical findings vary but also include eye lid chemosis and Horner’s-Tranta’s dots.
VKC and AKC can be seen as overlapping, however, the potential for morbidity is greater in untreated cases of AKC. VKC typically resolves by age of 20 while AKC can persist throughout life.3 In both instances, chronic eye rubbing has the potential to induce keratoconus.
In their most tacit forms VKC/AKC is a seasonal nuisance disease. It can be treated easily with palliative methods (tears, cold compresses, lubricants) and mild topical anti-allergy medications (topical vasoconstrictors, topical antihistamine/mast cell stabilizers). Oral non-sedating antihistimines can be used to concurrently manage accompanying non-ocular and adnexal symptoms.8 When possible the patient should be instructed to avoid the environmental and chemical agents that are known to provoke the process.
It their worst forms VKC/AKC can induce chronic debilitating symptoms along with tissue destruction capable of permanently affecting function.1-7 Topical non-steroidal anti-inflammatory medications (NSAID), qid-qd, can also be used to mitigate signs and symptoms.9 Here, dosage and length of use must be monitored. Documented cases of keratolysis (corneal melting) have been reported in the literature associated with increased frequency of administration and extended use.10,11 Since the pathology of AKC involves inflammation, topical corticosteroids may be required to suppress an aggressive inflammatory response. Prednisolone acetate 1% and difluprednate emulsion are topical ophthalmic steroids that can be prescribed for chronic forms of the disorder. While they are effective agents, both are known for their propensity to raise intraocular pressure with protracted use (difluprednate, 2-3 weeks, prednisolone acetate, 4-6 weeks). Loteprednol etabonate 0.5% is a less potent topical steroid with a reputation for having less risk for raising IOP. It should be considered as an option for patients who require long-term corticosteroid therapy.12,13 The dosing of topical steroids should vary depending on the individual case; qid-q2h for severe cases, with bid-qd dosing for cases requiring maintenance. In cases demonstrating raised IOP where the topical therapy must be continued, aqueous suppressants can be added. Here, because of their slow speed of onset and reputation for upregulating anterior segment inflammation, the topical prostaglandin medications should be avoided. Finally, topical steroids used for less than two weeks generally can be discontinued without tapering.
In the cases that evolve into painful events with iritis or cases inducing the formation of corneal shield ulcer, topical cycloplegia and broad-spectrum antibiotic prophylaxis should be added.1-7 In these instances, some prefer the convenience of a combination antibiotic/corticosteroid. Others keep the agents separate so that the fluorinated quinolone antibiotics are available and so that as the condition resolves, the antibiotic can be stopped while the topical steroid continued.
Patients who are inadequately controlled with topical corticosteroids or those who experience negative sequelae warranting discontinuation of steroids may require topical or systemic immunomodulatory therapy (oral, sublingual or subcutaneous routes).14-20 Topical cyclosporine may be an effective alternative in this situation; it has been shown to specifically inhibit T-lymphocyte proliferation while imparting direct inhibitory effects on eosinophil and mast-cell activation.14,15 Early research using 2% cyclosporine in maize oil demonstrated a distinct benefit16; however, clinical studies involving 0.05% cyclosporine emulsion have shown mixed results.14-19 Oral steroids are only considered in non-responsive situations.
Atopic dermatitis involving the lids, in addition to palliative treatments and oral antihistimines may require corticosteroid creams or ointments. Options include over the counter hydrocortisone 10%, fluorometholone ointment, 0.1% triamcinolone acetonide or 0.05% clobetasone butyrate. The immediate satisfaction topical steroid preparations can produce encourages patients to use them liberally or without consulting a professional. This relapsing behavior by the patient is sometimes known as “topical steroid addiction”. Since topical steroids can raise IOP and thin the dermis patients must be educated that unapproved use is not a sound strategy. In lieu of steroids, topical 0.1% tacrolimus ointment (Protopic, Astellas Pharma) has demonstrated equivalent safety and efficacy in a head-to-head clinical study.20,21
Some literature suggests the development of cataracts due to chronic corticosteroid therapy of AKC.5
Dr. Gurwood thanks Dr. Inna Kraisy for her contributions to this case.
1. Leonard Bielory, MD Allergic Diseases of the Eye Med Clin N Am 90 (2006) 129–148. 2. A. M. Zicari et al. vernal keratoconjunctivitis: atopy and autoimmunity. 2013;17:1419-1423. 3. Mario la Rosa et al. Allergic conjunctivitis: a comprehensive review of the literature. Italian journal of pediatrics 2013,39:18. 4. Ngoc PL et al. Cytokines, allergy, and asthma. Curr Opin Allergy Clin Immunol. 2005 Apr;5(2):161-6. 5. Bielory B, Bielory L:Atopic dermatitis and keratoconjunctivitis. Immunol allergy clin North Am 2010, 30:323-336. 6. Friedlander MH: Ocular Allergy. Curr Opin Allergy Clin Immunil 2011, 11(5):477-482. 7. Kumar S: Vernal keratoconjunctivitis: a major review. Acta Ophthalmol. 2009,87:133-147 8. Gane J, Buckley R. Leukotriene receptor antagonists in allergic eye disease: a systematic review and meta-analysis. J Allergy Clin Immunol Pract. 2013;1(1):65-74. 9. Li Z, Mu G, Chen W, et al. Comparative evaluation of topical pranoprofen and fluorometholone in cases with chronic allergic conjunctivitis. Cornea. 2013;32(5):579-82. 10. Demirel S, Sarac O. Late corneal perforation with topical diclofenac sodium use after radiotherapy. Eye Contact Lens. 2012;38(3):197-9. 11. Feiz V1, Oberg TJ, Kurz CJ, et al. Nepafenac-associated bilateral corneal melt after photorefractive keratectomy. Cornea. 2009;28(8):948-50. 12. Calder VL, Jolly G, Hingorani M, et al. Cytokine production and mRNA expression by conjunctival T-cell lines in chronic allergic eye disease. Clin Exp Allergy 1999;29(9):1214–22. 13. Novack GD, Howes J, Crockett RS, Sherwood MB. Change in intraocular pressure during long-term use of loteprednol etabonate. J Glaucoma 1998;7(4):266–9. 14. Whitcup SM, Chan CC, Luyo DA, et al. Topical cyclosporine inhibits mast cell–mediated conjunctivitis. Invest Ophthalmol Vis Sci 1996;37(13):2686–93. 15. Pucci N, Caputo R, Mori F. Long-term safety and efficacy of topical cyclosporine in 156 children with vernal keratoconjunctivitis. Int J Immunopathol Pharmacol. 2010;23(3):865-71. 16. Hingorani M, Moodaley L, Calder VL, et al. A randomized, placebo-controlled trial of topical cyclosporin A in steroid-dependent atopic keratoconjunctivitis. Ophthalmol 1998;105(9):1715–20. 17. Akpek EK, Dart JK, Watson S, et al. A randomized trial of topical cyclosporin 0.05% in topical steroid-resistant atopic keratoconjunctivitis. Ophthalmol 2004;111(3):476–82. 18. Daniell M, Constantinou M, Vu HT, Taylor HR. Randomised controlled trial of topical ciclosporin A in steroid dependent allergic conjunctivitis. Br J Ophthalmol 2006;90(4):461–4. 19. Settipane RA1, Peters AT, Borish L.Chapter 17: Immunomodulation of allergic sinonasal disease. Am J Rhinol Allergy. 2013;27 Suppl 1:S59-62. 20. Nivenius E, van der Ploeg I, Jung K, et al. Tacrolimus ointment vs. steroid ointment for eyelid dermatitis in patients with atopic keratoconjunctivitis. Eye 2007;21(7):968–75. 21. Tzu JH, Utine CA, Stern ME, Akpek EK. Topical calcineurin inhibitors in the treatment of steroid-dependent atopic keratoconjunctivitis. Cornea. 2012;31(6):649-54. |

