 |
Q:
I have a patient who was moving metal sheets and one slipped and caught him in the eye. How do I handle this case?
A:
Ocular trauma can be very concerning, and even the smallest abrasion or subconjunctival hemorrhage can be alarming for our patients. “When addressing ocular trauma, our initial goal is to assess the extent of damage,” says Alison Bozung, OD, who is on staff at Bascom Palmer Eye Institute in Miami, specializing in ophthalmic emergencies.
Examination
Evaluate the eyelids and periocular structures first. Full-thickness eyelid lacerations, for example, can indicate likely globe damage. Next, address the ocular surface including the conjunctiva and cornea. If there is a subconjunctival hemorrhage, closer inspection will often reveal a conjunctival laceration as well.
In dealing with eye injuries, rule out open globes first, according to Dr. Bozung. When assessing a conjunctival laceration, the subconjunctival hemorrhage may limit your view. “Be particularly mindful of the possibility of a scleral rupture in the presence of a complete subconjunctival hemorrhage obscuring the entire sclera,” Dr. Bozung warns.
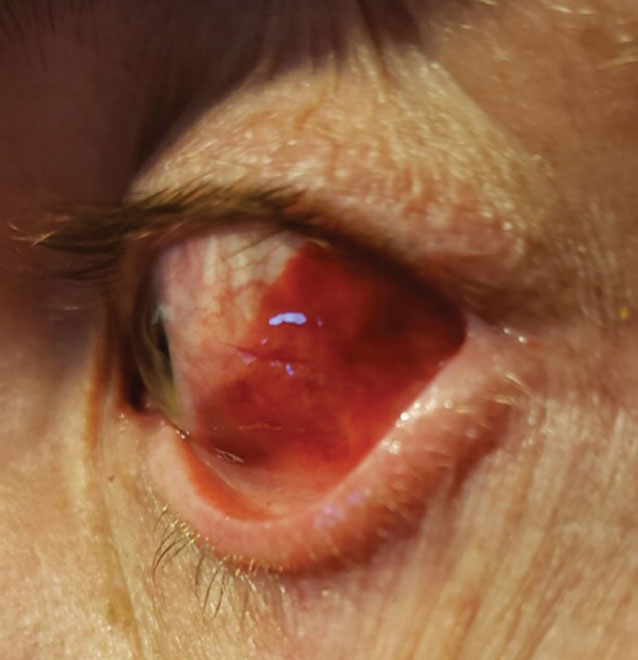 |
| When assessing conjunctival laceration, subconjunctival hemorrhage may limit view of the sclera. Click image to enlarge. |
Most commonly, scleral ruptures from blunt trauma will occur at the limbus or posterior to muscle insertions. If defect depth is not particularly obvious, anesthetize the eye and use a fluorescein strip to paint over the area of concern in order to look for a Seidel sign, as you would with a corneal wound leak. Instilling fluorescein will also highlight any corneal or conjunctival abrasions.
“When the extent of tissue violation anywhere is still unclear, you may want to gently explore the tissue with a cotton-tipped applicator moistened by sterile water or saline,” Dr. Bozung suggests. Be on the lookout for any residual foreign matter. If a deep or non-mobile foreign body is present, or if any uveal tissue is showing, refer this patient to an anterior segment or orbital specialist for further globe exploration and possible CT imaging.
A dilated fundus exam is a critical part of an ocular trauma assessment. Only avoid dilation in very specific circumstances, such as when there is uveal tissue prolapsed through a wound, a foreign body in the anterior chamber or obvious globe disorganization. “Use fundus examination to rule out retinal breaks or detachment, vitreous hemorrhage and intraocular foreign body,” Dr. Bozung says. In cases that sustain focal trauma to the globe, pay special attention to the corresponding area of the retina. Note changes such as commotio retinae or retinal hemorrhage.
Treatment
Treating conjunctival lacerations is quite simple in most cases. Often, small lacerations will heal without surgical intervention. Dr. Bozung will typically prescribe a prophylactic broad-spectrum topical antibiotic drop or ointment four times daily until the defect has closed. “Remind patients not to rub their eye and to temporarily discontinue contact lens wear, as this mechanical irritation may impede healing,” she says.
A plastic shield at night is a good way to prevent accidental rubbing or pressure on the traumatized eye. In the case of an extensive conjunctival laceration, consider referral. When surgical repair is indicated, absorbable sutures are typically used. The surgeon typically exercises care to ensure a sterilized wound with properly apposed edges while taking care to avoid capture of subjacent Tenon’s capsule.
“Fortunately, superficial conjunctival lacerations, such as with this patient, are often self-limiting and of minimal consequence,” Dr. Bozung says. “A thorough examination can rule out more dangerous complications of ophthalmic trauma and ensure our patients’ visual health is not compromised.”

