The urgent care department of the local hospital referred an 85-year-old white male with acute pain in his left eye. The patient reported waking up in the middle of the night with severe pain in the eye. This was the first time he noticed pain such as this in that eye.
The patient had a history of decreased visual acuity, no light perception vision and elevated intraocular pressure in the left eye. The elevated IOP was a complication of a previous central retinal vein occlusion (CRVO) that became ischemic. The patient did not use any IOP-lowering medications because the eye was functionally blind and there were no previous reports of discomfort.
Systemic history was positive for hypertension, hyperlipidemia, cerebrovascular accident and coronary artery bypass surgery. He was taking the following medications: Coumadin (warfarin sodium, Bristol-Myers Squibb), Protonix (pantoprazole sodium, Wyeth), Flomax (tamsulosin, Boehringer Ingelheim) and Lipitor (atorvastatin calcium, Parke-Davis). He also took the generic medications lisinopril, metoprolol, isosorbide and aspirin.
Diagnostic Data
Entering visual acuity was 20/150 in the right eye with no improvement using pinhole. There was no light perception in the left eye.
Pupils were round but uneven, and there was a relative afferent pupillary defect in the left eye. IOP measured 10mm Hg O.D. and 48mm Hg O.S.
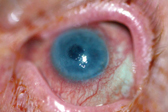
1. Steamy, decompensating cornea as seen in a patient with elevated IOP.
Slit-lamp examination of the right eye was unremarkable but revealed small bullae (ruptured and intact) and epithelial erosions on the left cornea inferiorly. The left cornea was edematous and steamy, making iris detail invisible. A layered hypopyon was also present in the anterior chamber of the left eye. Funduscopic examination could not be performed during this exam due to the hazy nature of the cornea. Dilated exam of the right eye revealed advanced retinal pigment epithelial dropout from dry age-related macular degeneration.
Diagnosis
We diagnosed this patient with ruptured bullae and corneal erosions secondary to corneal decompensation in the left eye (figure 1). The decompensation was a result of long-standing elevated IOP.
Treatment and Follow-up
We fit the patient with a bandage soft contact lens that was soaked in Zymar (gatifloxacin ophthalmic solution 0.3%, Allergan) prior to insertion. We also placed him on gatifloxacin one drop tid in the left eye.
We also discussed two possible options for pain relief: retrobulbar injection with Thorazine (chlorpromazine, GlaxoSmithKline) and enucleation. We instructed the patient to return in three days.
At the follow-up visit, the patient had no complaints of pain in the left eye. Visual acuity was slightly worse at 20/200 O.D. and no light perception O.S. We removed the bandage contact lens after the slit lamp examination. The corneal bullae and epithelial erosions were resolved but some residual corneal haze remained. The anterior chamber was deep, and a hypopyon was still present. We noted iris rubeosis at this time. IOP in the left eye was stable at 47mm Hg.
We instructed the patient to continue using the gatifloxacin tid for three more days and added Refresh Liquigel (Allergan) for extra lubrication and comfort. We prescribed no other therapy at this time.
The patient returned approximately three months later complaining of pain in the left eye and trouble sleeping as a result. At this time, we decided that conservative therapy was no longer the best option. The patient indicated that he would like to pursue retrobulbar chlorpromazine injection, so we scheduled the procedure for the next available surgical date.

2. Needle position in the retrobulbar space after injection with Xylocaine and before chlorpromazine injection.
To administer the injection, we placed the patient in the supine position and applied tetracaine ophthalmic to anesthetize the left lower cul-de-sac. We then prepped the eye with Betadine (povidone-iodine, Purdue Frederick) and draped it.
Using a retrobulbar needle and a 3cc syringe, we injected 2cc of Xylocaine (lidocaine and epinephrine, AstraZeneca) in a retrobulbar fashion behind the left eye. We maintained the hub of the needle, clamped it with forceps and removed the syringe (figure 2). After waiting for two minutes, we attached a 3cc syringe with 2ml chlorpromazine 25mg/ml to the retrobulbar needle and injected it into the retrobulbar space. We removed the retrobulbar needle and syringe, and applied pressure to the left globe for a few moments. We also applied a pressure patch and instructed the patient to maintain the patch for three hours.
At follow-up the next day, the patient noted no pain in the left eye. The only adverse postoperative event was profuse swelling of the upper and lower eyelids (figure 3). This swelling slowly resolved within three to four weeks after the injection. To date, this patient has enjoyed 10 pain free months and no further complications secondary to the injection. His IOP remains elevated with continued corneal decompensation that we managed with lubrication.
Discussion
Many conditions can result in a blind and painful eye. Prior trauma is the most common cause.1 Other causes include chronic retinal detachment, corneal ulcer, phthisis bulbi, infraorbital neuralgia, endophthalmitis, failed corneal grafts, neovascular glaucoma and end-stage (absolute) glaucoma.2
Retrobulbar alcohol injections were first administered in the early 1900s and have since been used for pain relief in both blind and seeing eyes. Alcohol concentrations of 60%, 80% or 96% have been used. Alcohol achieves pain relief by coagulating the proteins of the nerves that supply sensation to the globe.2,3
For painful eyes that still have useable vision, the treatment goal is to relieve the pain yet maintain as much vision as possible. If the eye is blind, treatment objectives are to alleviate the pain and preserve the globe.
Retrobulbar alcohol injection becomes a valid option when an eye looks normal and/or the patient is not medically or psychologically fit for enucleation or evisceration.2 Some of the most common indications for alcohol injection are end-stage glaucoma, endophthalmitis and corneal ulcer.2 Enucleation or evisceration should still be considered the treatment of choice if you cannot rule out an intraocular tumor even after ultrasound investigation.2
Enucleation involves the removal of the eyeball from the orbit. The surgeon separates the globe from its six extraocular muscle attachments, then severs it from the optic nerve. This is followed by replacement with some form of orbital implant.4
Evisceration is a surgical procedure in which the surgeon removes the intraocular contents of the eye through a paralimbal incision.5 The removed contents include all accessible uveal tissue (iris, ciliary processes, ciliary body and choroid), retina, vitreous and lens. The scleral shell is left attached to the extraocular muscles. Enucle-ation and evisceration remain the most consistent and reliable methods for achieving complete and permanent resolution of pain in blind eyes.1

3. This patient experienced eyelid edema postoperatively on day one.
Indeed, the efficacy of retrobulbar alcohol has been shown to be as high as 87% in some studies and as low as 20% in others.3,6 The length of duration for pain relief also varies, ranging from two weeks to two years, with an average of one to seven months.2,7
There are several possible side effects associated with alcohol injection. These include lid swelling (21% of patients), conjunctival chemosis (13%), retrobulbar hemorrhage (5%), blepharoptosis (13%), sixth-nerve palsy (10%), corneal epithelial defect (8%), ophthalmoplegia and cellulitis.2,3,8 Some of these complications are more serious than others, but most seem to subside within 12 weeks and leave no lasting effects. The benefit of the pain relief often outweighs the risk of these complications.3
French physicians first used chlorpromazine in 1951 as an antipsychotic agent. We still dont understand the origin of its discovery as a substance for relief of pain through retrobulbar injection, nor do we understand its mechanism of action.8 One hypothesis: The mechanism of action has to do with the membrane stabilizing effects the drug has on the ciliary ganglion.
Chlorpromazine is generally administered in a 1ml or 2ml dose using a concentration of 25mg/ml or 40mg/ml. Because there is some systemic absorption after injection, the 25mg/ml concentration is preferred.7,9
In recent studies, the efficacy of chlorpromazine has been shown to rival that of alcohol with rates of pain relief as high as 80%.7 The average duration of relief ranged from three months in one study, to slightly more than a year in another. Thats better than the reported one- to seven-month average for retrobulbar alcohol.7,9
The most common reported side effects for chlorpromazine are transient palpebral edema (40%) and chemosis (47%). Transient ptosis, phthisis bulbi, sterile orbital cellulitis, hyphema, increases in IOP, nausea and vomiting, and brief loss of consciousness also are reported side effects, but these are not common.7,9
Chlorpromazine has been used on both blind and seeing eyes. The results in the seeing eyes are promising. In one study, half the seeing eyes treated retained their vision.7 In another study of five seeing eyes that were treated, vision decreased in two, remained the same in two and actually improved in one eye.9 The improvement was not directly due to the injection of chlorpromazine, but can be attributed to subsequent surgeries.9
Although retrobulbar alcohol has long been the standard of treatment for ocular pain, chlorpromazine appears to be just as effective, with a longer duration of pain relief and fewer complications. With the added bonus of sight preservation in more than 50% of seeing eyes, chlorpromazine has become a promising treatment of choice for such painful eyes. It has also become a viable option for patients who are not willing to undergo enucleation or evisceration.
Dr. Rhen is a recent graduate of Pacific University, College of Optometry. Dr. Skorin is a contributing editor of Review of Optometry and staff ophthalmologist at Albert Lea Eye Clinic-Mayo Health System, Albert Lea, Minn. He lectures both nationally and internationally.
1. Custer PL, Reistad CE. Enucleation of blind, painful eyes. Ophthal Plast Reconstr Surg 2000 Sep;16(5):326-9.
2. Al-Faran MF, Al-Omar OM. Retrobulbar alcohol injection in blind painful eyes. Ann Ophthalmol 1990 Dec;22(12):460-2.
3. Olurin O, Osuntokun O. Complications of retrobulbar alcohol injections. Ann Ophthalmol 1978 Apr;10(4):474-6.
4. Chen WP. Enucleation. In: Chen WP, ed. Oculoplastic Surgery: The Essentials. New York: Thieme, 2001:327-45.
5. Chen WP. Evisceration. In: Chen WP, ed. Oculoplastic Surgery: The Essentials. New York: Thieme, 2001:347-53.
6. Maumenee AE. Retrobulbar alcohol injections: relief of ocular pain in eyes with and without vision. Am J Ophthalmol 1949;32:1502-8.
7. Chen TC, Ahn Yuen SJ, Sangalang MA, et al. Retrobulbar chlorpromazine injections for the management of blind and seeing painful eyes. J Glaucoma 2002 Jun;11(3):209-13.
8. Scerra C. Chlorpromazine alleviates some eye pain better than alcohol. Ophthalmol Times 1998;23(22):30.
9. Estafanous MF, Kaiser PK, Baerveldt G. Retrobulbar chlorpromazine in blind and seeing painful eyes. Retina 2000;20(5):555-8.

