New Neuroprotective Target in Glaucoma
Lowering IOP may one day take a back seat to a more direct treatment strategy.
By
A new study suggests lipid mediators found in the inner retina may be a key to halting glaucoma progression.1 Using a rodent model, researchers at the University of California–Berkeley and the University of Toronto found that lipoxins—inflammation-regulating lipid mediators—secreted from astrocytes stopped retinal ganglion cell (RGC) degeneration. While lipoxins are known to be anti-inflammatory, the researchers were excited to uncover their neuroprotective abilities.1
After discovering lipoxin A4 and B4 secretions in the retina and optic nerve head, the researchers wanted to test their treatment potential. They administered them to rodents eight weeks after the onset of glaucoma-like damage and neurodegeneration and found injecting either lipoxin A4 or B4 provided sufficient neuroprotection; conversely, inhibiting key lipoxin pathway components exacerbated the damage from injury.1 At 16 weeks, they found that lipoxin B4, in particular, stopped RGC degeneration.
“At rest, astrocytes provide a host of neurotoxic and neuroprotective mediators to neighboring RGCs, but during acute or chronic injury the neuroprotective response is suppressed,” says Brian D. Fisher, OD, who practices at the Villages VA Outpatient Clinic in the Villages, Fla. “In the study’s glaucoma model, the administration of the specific lipid mediator LXB4 showed a preservation and restoration of both RGC function and retinal nerve fiber layer structure.”
The researchers have already filed a patent application and hope to one day start clinical trials. If successful, it could finally address the neurodegeneration of glaucoma directly instead of through the proxy of IOP.
“With glaucoma being a leading cause of blindness worldwide with no definitive cure, the results from this show promise for a therapeutic breakthrough,” says Dr. Fisher. “If we can control intraocular pressure and provide neuroprotection to our patients, we would have less visual impairment caused by glaucoma, and keep our patients functional.”
“Neuroprotection has long been the Holy Grail of glaucoma management, but thus far everything has fallen short,” says Joseph W. Sowka, OD, a professor at Nova Southeastern University College of Optometry. “Now, it certainly seems possible to be able to one day use such a novel treatment, likely in conjunction with conventional IOP lowering therapies, in a holistic management of glaucoma.”
| 1. Livne-Bar I, Wei J, Liu H, et al. Astrocyte-derived lipoxins A4 and B4 promote neuroprotection from acute and chronic injury. J Clin Invest. November 6, 2017. [Epub ahead of print]. |
AMD: Supplement Regardless of Genotype
Recently, after re-analyzing data from the Age-Related Eye Disease Study (AREDS), researchers found no evidence to suggest any genotype-treatment interactions, bringing into question if clinicians should still refrain from prescribing them for patients with age-related macular degeneration (AMD) of certain genotype subgroups.1 The results were presented at the Annual Meeting of the American Academy of Ophthalmology in New Orleans, Nov. 11-14, 2017.
 |
| Based on the AREDS classification system, this eye qualifies as intermediate AMD and would benefit from supplementation. Photo: Julie Poteet, OD |
The researchers looked at 879 AREDS participants for whom the same CFH and ARMS2 single nucleotide polymorphisms were available. The study took a three-pronged approach: One team focused on data concordance between conflicting studies; another focused on replicating the interaction between genotype and treatment found in previous reports; and the third group looked at baseline predictors of treatment response.1
After crunching the numbers again, the investigators realized errors existed in the data used to support the notion of a genotype-treatment interaction. Together, the three groups were unable to replicate any genotype-treatment interaction, although they did discover treatment was more beneficial for high-risk patients.1
“Even if we assumed that interactions in fact did exist, we did not find evidence to support the claim that supplementation leads to a large increase in the risk of advanced AMD in some genotype subgroups,” the study reads.1
Given this new evidence, the researchers suggest supplementation should be recommended for any patients who meet criteria for supplementation with zinc and antioxidants, regardless of genotype.1
“This study seems to have approached this controversy in a very rational way to come up with an unbiased conclusion,” says
Mohammad Rafieetary, OD, a consultative optometrist at the Charles Retina Institute. “I personally agree with their conclusion; however, I don’t think the debate over this issue, as well as the appropriate zinc dosing and the correct benchmark to start the patient (i.e., at risk vs. those with AMD), will go away anytime soon.”
Combo Therapy Helps with PEDs
A new study adds to the body of evidence suggesting autologous serum eye drops (ASEDs) in combination with silicone hydrogel contact lenses (CLs) can lead to successful re-epithelialization for post-infectious persistent epithelial defects (PEDs).1
“Each of these therapies have been used independently for treatment of this condition, and several small case series had previously reported successful use of a combination approach with persistent epithelial defects,” says Aaron McNulty, OD, who practices at Louisville Eye Center in Louisville, KY. “This report is novel because it applies a combination approach specifically to post-infectious persistent defects.”
Researchers reviewed 12 cases of post-infectious corneal PEDs unsuccessfully treated with conventional medical management that were then treated with combined topical 20% ASEDs and silicone hydrogel CLs. They found all 12 PEDs had complete re-epithelialization within two weeks without adverse effects. They also noticed all 12 had improved best-corrected visual acuity with the decreased intensity of corneal scarring and reduced corneal edema.1
“This combination therapy is within the scope of practice of optometrists and represents an effective treatment for an often frustrating condition,” says Dr. McNulty. In addition, even though this study describes treatment of a very specific type of epithelial defect, Dr. McNulty suggests clinicians may consider using this therapy for other persistent epithelial defects as well.
| 1. Wang WY, Lee YK, Tsai SH, et al. Autologous serum eye drops combined with silicone hydrogen lenses for the treatment of postinfectious corneal persistent epithelial defects. Eye Contact Lens. 2017;43(4)225-9. |
Gene Therapy Shows Promise For Inherited Retinal Disease
Patients diagnosed with Leber congenital amaurosis (LCA) may have a new treatment option to look forward to that has significant real-world implications. Researchers found that 27 of 29 patients treated with gene therapy, or 93%, experienced meaningful improvements in their vision, including light sensitivity and peripheral vision.
“Hard work and perseverance for the past decade by many researchers has finally resulted in the first commercial gene therapy to treat any eye disease,” says Jerome Sherman, OD, a professor at SUNY College of Optometry. “LCA is considered one of the most devastating of all the retinal degenerations, since blindness is present at birth and is typically progressive.”
The therapy involves the injection of billions of harmless viruses genetically modified to carry a healthy version of the gene to the retina.
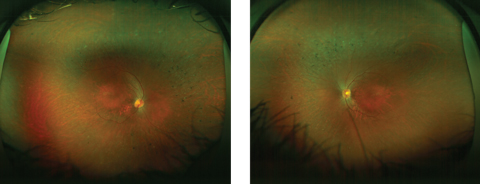 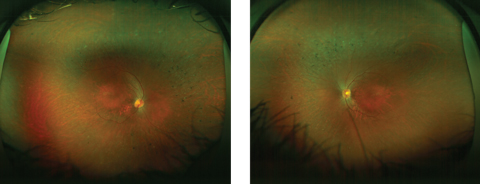 |
| This 19-year-old patient, diagnosed with LCA at six months of age, has attenuated arterioles and bone-spicule pigmentation in the mid-periphery of both eyes. Click photos to enlarge. Photos: Sherry J. Bass, OD |
Although the treatment does not restore normal vision, it does allow the patient to see shapes and light, which could give patients enough functional vision to move around without a guide dog or cane. So far patients have retained their improved vision for two years.
For the one in roughly 80,000 individuals diagnosed with LCA, the news is huge, according to researchers presenting the findings at the Annual Meeting of the American Academy of Ophthalmology in New Orleans, Nov. 11-14, 2017. No gene therapy for retinal disease—or any other eye disease, for that matter—has come this close to approval by the US Food and Drug Administration (FDA). This new treatment is currently under FDA review and could be approved soon, the researchers said.
“Clinicians need to be aware of LCA since effective treatment will shortly be available for at least LCA patients with the abnormal RPE65 gene,” says Dr. Sherman. “Although RPE65 LCA is rare, the approval of an effective treatment gives hope to all patients with myriad other inherited retinal degenerations. For the first time in my five-decade career diagnosing such patients, I can now offer them hope. For those young patients, I tell them that I am (near) certain that a cure will be available in their lifetime.”
In the newsThe five-year risk of developing age-related macular degeneration (AMD) is decreasing with each generation, according to a new study. Researchers analyzed data from 4,819 Baby Boomers and their adult children from the Beaver Dam studies and found the risk of AMD decreased by a relative 60% for each generation. Researchers have yet to discover the factors contributing to this decline. Cruickshanks KJ, Nondahl DM, Johnson LJ, et al. Generational differences in the 5-year incidence of age-related macular degeneration. JAMA Ophthalmol. November 16, 2017. [Epub]. Research now suggests donor corneal tissue can be stored for 11 days before implantation—four days longer than the current protocol of seven days. Investigators looked at 1,090 people (1,330 eyes) that underwent DSAEK at 40 different surgery centers and found a 92.1% three-year success rate for corneas preserved eight to 14 days, and 95.3% for those preserved up to seven days. Further analysis revealed much of the difference between the groups came from corneas preserved 12 to 14 days. Lass JH, Benetz BA, Verdier DD, et al. Corneal endothelial cell loss 3 years after successful descemet stripping automated endothelial keratoplasty in the cornea preservation time study. JAMA Ophthalmol. November 10, 2017. [Epub]. Clinicians now have a better idea of population-based estimates of diplopia in the United States, thanks to a new study. Researchers found diplopia accounts for roughly 850,000 yearly doctor office and emergency department (ED) visits. While life-threatening diagnoses were rare in the ambulatory setting, approximately 16% of the ED visits resulted in a diagnosis of stroke or transient ischemic attack. De Lott LB, Kerber KA, Lee PP, et al. Diplopia-related ambulatory and emergency department visits in the United States, 2003-2012. JAMA Ophthalmol. October 26, 2017. [Epub]. |

