Perhaps no other ocular structure does so much yet receives such cursory clinical descriptions as the conjunctiva. ‘Clear and quiet,’ ‘pinguecula nasal’ and ‘diffuse injection’ dominate the lexicon as practitioners evaluate the state of this ocular structure. While it doesn’t catch our attention with flashy biochemical processes or precisely change shape to focus light, the conjunctiva performs a number of essential functions. For instance, it acts as a defense of the globe and eyelids, produces the mucus portion of the tear film and facilitates the globe’s freedom of movement. So, when the conjunctiva is insulted, it can be a calamity. Here’s a closer look at the structure and the conditions that can compromise its integrity.
  |
| This patient presented with a unilateral ptosis, edema and injection, characteristic of viral conjunctivitis. Click image to enlarge. |
Anatomy
The conjunctiva is a mucous membrane that extends from the corneolimbus across the globe, down into the fornix and then returns back up the inner surface of the eyelid, terminating at the keratinized margin. It is composed of cuboidal epithelial cells interspersed with Langerhans cells, melanocytes and lymphocytes. Underneath the epithelium is a richly vascularized substantia propria containing lymphatics and additional immune cells.1
The conjunctiva is typically divided into three sections: the palpebral conjunctiva, the bulbar conjunctiva and the fornix. The average conjunctiva covers 16cm2—13 times greater than the surface of the cornea, and 1.3 times greater than the area of the retina.2 The conjunctiva allows for unencumbered movement of the globe, provides a protective barrier for the eyeball and orbit, contributes to production of the tear film and hosts ocular immune tissues.1
The ophthalmic division of the trigeminal nerve provides sensation, while autonomic efferents supply the vessels, accessory lacrimal glands and epithelium. Vascular supplies to the bulbar conjunctiva and fornices are provided by the long ciliary arteries and peripheral tarsal arcades. The palpebral conjunctiva is primarily supplied by the terminal branches of the ophthalmic artery and secondarily by the branches of the facial artery. Blood drains from the bulbar conjunctiva and fornices via the anterior ciliary and conjunctival veins, while the palpebral conjunctiva drains into the post-tarsal veins of the eyelids and the deep facial branches of the anterior facial vein and the pterygoid plexus.
The conjunctiva houses the only ocular lymph tissue. Nasal lymphatics drain into the submandibular nodes, while temporal vessels empty into the pre-auricular nodes.1
Diagnostic Considerations
When the eye is insulted, whether from an allergen, microbe, chemical assault, physical trauma or autoimmune cause, the local tissue reaction is an inflammatory response—conjunctivitis. When a patient presents with a red, irritated eye, it can be challenging to determine the cause of their conjunctivitis. Each type has key characteristics, and checking the boxes off on your clinical checklist can help narrow down the etiological culprit (Table 1).
Thorough history. It is crucial to ascertain as many details from the patient as possible, including onset, duration and laterality. Take note of symptoms, such as pain or itching, to further help distinguish etiology. For instance, a chief complaint of itching is highly suggestive of an allergic reaction, while severe pain is quite uncommon in isolated conjunctivitis and would warrant a check of the cornea for epithelial defects and foreign bodies.
Patient education. Because a high risk of transmission exists with bacterial and viral conjunctivitis, remember to thoroughly educate patients about rigorous hygiene.
Lab work. In many cases, cultures or other laboratory investigations are helpful to find the cause of the patient’s conjunctivitis.
Here we focus on the three most common types of each conjunctivitis etiology—viral, allergic and bacterial—and the pearls regarding their diagnosis.
 |
| In the same viral conjunctivitis patient, follicles and injection were present on the palpebral conjunctiva, and sub-epithelial infiltrates were present in the cornea. |
Viral Conjunctivitis
Practitioners often encounter patients with a chief complaint of the dreaded pink eye, and up to 80% of infectious cases of acute red eye are viral in origin.3 When patients present with a red, irritated eye and you suspect a viral etiology, two virus types may be at play: adenovirus and coxsackie virus.3,4
Adenovirus. Of the 53 subtypes of adenovirus in existence, 19 are responsible for 90% of all viral conjunctivitis.4 Infections can be present in relative isolation, but often occur as epidemics in places such as schools, hospitals and swimming pools. The virus is capable of surviving for weeks, even on dry surfaces. Patients begin to shed virus particles days prior to the onset of symptoms; therefore, many individuals may be affected before preventative measures can be employed.5
The adenoviridae infections manifest in four clinical presentations: non-specific follicular, pharyngoconjunctival fever (PCF), epidemic keratoconjunctivitis (EKC) and chronic adenoviral conjunctivitis. The exact incidence of each of the adenoviral presentations is unknown. Symptoms may be mild to severe, with unilateral redness and serous discharge spreading to the second eye one to two days later.
Follicular conjunctivitis is the most common variant and produces a mild bilateral conjunctivitis with watery discharge and no corneal involvement.4 It is associated with serotypes 1 through 11 and 19.6 PCF, which is caused by adenoviral serotypes 3, 4 and 7, can affect the cornea in about 30% of cases.4 It is associated with pharyngitis, high fever and pre-auricular lymphadenopathy.3 Both follicular conjunctivitis and PCF may be associated with a sore throat and are seen often in children. EKC, adenovirus serotypes 8 and 19, is the most severe form and involves the cornea about 80% of the time.4-6 The initial ocular presentation of EKC and PCF is similar, making differentiation difficult on ocular presentation alone. Therefore, it is helpful to remember to check for the systemic manifestations of PCF, while corneal subepithelial infiltrates are much more commonly seen with EKC.7
Chronic follicular conjunctivitis, the rarest adenoviral conjunctivitis variant, is characterized by intermittent, relapsing episodes of follicular conjunctivitis, though papillae may predominate.4 The clinical presentation is less severe than in other forms. The condition, though sometimes lasting for years, tends to resolve spontaneously. Adenoviral serotypes 2, 3, 4 and 5 have been isolated from affected individuals.7
Coxsackie virus. Acute hemorrhagic conjunctivitis creates a startling clinical presentation. It is more common in tropical areas and is usually caused by the enterovirus or coxsackie virus. Infectious outbreaks typically occur in underdeveloped countries with a prevalence of up to 50%.8 Patients are often worried by the particularly red, bloody appearance of the petechial subconjunctival hemorrhages present with this type of infection.4,5
Diagnosis. In viral conjunctivitis, clinical signs often govern the diagnosis. These include eyelid edema, as well as a swollen preauricular node and conjunctival redness, follicles, membranes and pseudomembranes. Corneal involvement includes superficial punctate keratitis in mild cases, or discrete whitish anterior stromal infiltrates, which may persist for months.4,5
Though diagnosis is typically made based on clinical presentation, Giemsa stain can reveal multinucleated giant cells in herpetic infection and mononuclear cells in adenovirus infection. Viral cultures, nucleic acid amplification and, more recently, in-office immunochromatography tests such as the AdenoPlus (Quidel), are available for point-of-care diagnosis. The AdenoPlus test kit identifies the presence of adenovirus with a sensitivity of 93% and specificity of 98%, according to research. The in-office test results are available within approximately 10 minutes.9,10
Table 1. Differential Diagnosis of Viral, Allergic and Bacterial Conjunctivitis | |||
| Viral | Allergic | Bacterial | |
| Laterality | Unilateral, then bilateral | Bilateral | Unilateral, then bilateral |
| Tissue response | Follicles Chemosis Petechial hemorrhages Subepithelial Infiltrates | Papillae Chemosis Corneal scarring, if severe | Papillae Subepithelial Infiltrates *Note: mixed papillary and follicular response with Chamydia |
| Discharge | Serous, mucoserous | Serous, mucoserous | Mucopurulent, purulent |
| Membrane/pseudomembrane | Yes | No | Yes |
| Lympadenopathy | Yes | No | Only with Neisseria and Chlamydia |
Ocular allergy is comprised of several distinct clinical entities representing a veritable alphabet soup of acronyms. These include seasonal allergic conjunctivitis (SAC), perennial allergic conjunctivitis (PAC), vernal keratoconjunctivitis (VKC), contact allergic conjunctivitis (CAC), giant papillary conjunctivitis (GPC) and atopic keratoconjunctivitis (AKC). Some of these conditions are acute and visually benign, while others are chronic and pose the threat of permanent vision loss.1,4,6,11
Acute allergic conjunctivitis. SAC and PAC represent the milder and more common types of ocular allergy, and both are classified as acute. SAC is the most common form of allergic conjunctivitis, is often accompanied by allergic rhinitis, and its incidence and duration is tied closely to the arrival of plant-derived allergens.12
In PAC, allergens such as dust mites and pet dander are often triggers, and though patients often notice exacerbations and remissions, this condition occurs throughout the year. Itching is a hallmark sign of these conditions, and papillary response, watery or stringy discharge, conjunctival hyperemia and mild to moderate conjunctival chemosis are generally present to variable degrees.1,13
Despite the significant discomfort for patients, these two entities do not pose a significant risk to vision.
Chronic allergic conjunctivitis. VKC and AKC, chronic forms of allergic conjunctivitis, have prolonged, complex inflammatory reactions involving a number of immune responses, which includes T-cells, eosinophils, basophils, neutrophils and associated cytokines. While all types of allergic conjunctivitis have a type I hypersensitivity response, the cell-mediated type IV response typified in these conditions is responsible for their sight-threatening effects.14,15 Risk of permanent vision loss rises sharply with these conditions due to the potential for secondary conjunctival and corneal scarring and, although rare, corneal perforation. VKC generally presents in males younger than age 30, while AKC exhibits a weaker gender predilection. AKC usually presents after the age of 30, with visual complications in the fourth and fifth decades. Ninety-five percent of cases are associated with a history of atopic dermatitis.4,6,11
GPC, the third form of chronic allergic conjunctivitis, is caused by chronic irritation, usually from contact lenses, ocular prostheses, exposed surgical sutures, scleral buckles, corneal surface irregularity and filtering blebs. GPC is a mechanically induced allergic reaction and generally resolves when the source of the mechanical irritation is removed. Later in the condition, giant papillae can be greater than 1mm in diameter.4,15,16
CAC occurs when the conjunctiva exhibits a type IV delayed hypersensitivity reaction to ocular medications or their preservatives. This usually presents after patients have been exposed to a medication, solution, contact lens material or preservative for several days.4,6,11
Diagnosis. All types of allergic conjunctivitis are diagnosed based on signs and symptoms. A family history of atopic disease or asthma may support suspicion of ocular allergies. Itching is the hallmark sign of ocular allergy, and its absence makes this diagnosis unlikely. In contrast, conjunctival scrapings may reveal eosinophils, but their absence does not rule out ocular allergies.
Conjunctival provocation testing with suspected allergens may help determine the effectiveness of therapeutics if a patient has a history of severe allergies. A blood test, the radioallergosorbent test or ELISA testing of tears may be performed to identify specific allergens.
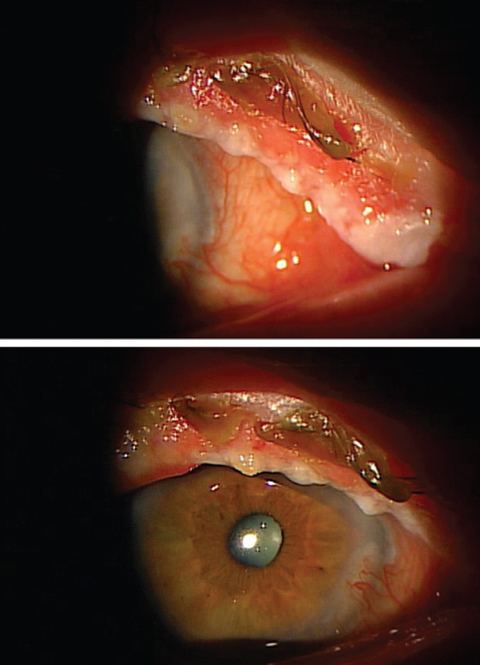 |
| In the case of this acute bacterial blepharoconjunctivitis patient, a culture was obtained, which revealed S. aureus overgrowth. A pseudomembrane is seen emerging from the upper lid in the second picture (bottom). |
Bacterial Conjunctivitis
Last but not least, bacterial conjunctivitis is caused by direct inoculation with infectious secretions. Three presentations of bacterial conjunctivitis exist: acute, hyperacute and chronic.
Acute bacterial conjunctivitis. The most common causes of acute bacterial conjunctivitis are Streptococcal pneumonia, Staphylococcus aureus, Haemophilis influenzae and Moraxella catarrhalis. Severe presentations should prompt suspicion of Neisseria species.4
Because S. aureus is ubiquitous in skin flora, it can present at any time and has no demographic predilection. S. pneumoniae infections are more common among children in cooler climates, while H. influenza is more commonly seen in children in warmer climates and tends to have a more severe presentation.17
Symptoms include sudden onset of redness, burning and discharge occurring in both eyes, though one may precede the other by one to two days. Clinical findings can include conjunctival and eyelid edema, erythema, papillae, mucopurulent discharge and punctate corneal staining. In contrast to viral or allergic conjunctivitis, bacterial discharge often has a yellow-green appearance along with matting of the eyelids. Lymphadenopathy typically seen in viral conjunctivitis is absent, except in cases of Neisseria infections. In rare cases, the cornea can become compromised.4,18,19
Hyperacute conjunctivitis. Although they are responsible for only a small number of cases of conjunctivitis, Neisseria gonorrhoaea and meningitides should be suspected in cases of severe conjunctivitis. Signs include hyperpurulent discharge, severe lid edema, corneal ulceration, lymphadenopathy and pseudomembranes. If a corneal ulcer is present, aggressive treatment is necessary due to the risk of perforation within 24 hours.18,19
In these cases of hyperacute conjunctivitis, culture is mandatory. Culture media include Giemsa stain, Chocolate agar and Thayer-Martin. Patients who test positive for Neisseria should also be tested for concurrent sexually transmitted diseases including syphillus, chlamydia and HIV.4,6
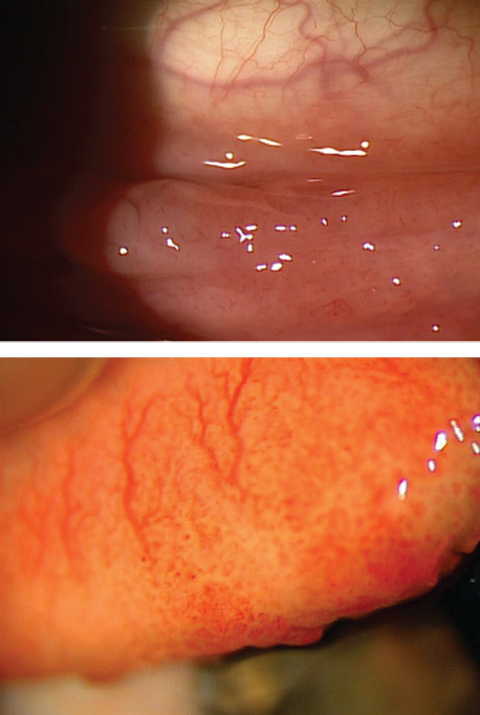 |
| These images highlight the difference in appearance between follicles (above) and papillae (below). |
Chronic bacterial conjunctivitis. When the signs and symptoms of bacterial conjunctivitis have been present for more than four weeks, there are two likely infectious causes to consider: a chronic overgrowth of normal flora, typically seen as blepharitis, and chlamydia.11,20
The most common cause of blepharitis is Staphylococcus. If ulceration is seen near the lacrimal structures and puncta, Moraxella lacunata should also be considered as a causative agent. As practitioners, we see this every day, and we all know the typical signs and symptoms: tearing, foreign body sensation, conjunctival hyperemia, thickening of lid margins, telangectatic vessels, rosettes, collarettes, inferior superficial punctate keratitis and even sterile infiltrates. Blepharitis is easy to diagnose based on the clinical picture, but it is extremely difficult to eradicate due to the always-present skin flora.
Chlamydia, caused by Chlamydia trachomatis, is typically diagnosed in young, sexually active patients who present with a red eye that does not respond to other treatments and is present for three to four weeks. Chlamydia trachomatis is an intracellular obligate bacterial species and is capable of causing a mild unilateral or bilateral chronic conjunctivitis associated with redness, watering and discharge. Preauricular lymphadenopathy and large follicles primarily of the lower fornix are common findings. Mild conjunctival scarring and corneal infiltrates may also be seen. Tarsal conjunctival scrapings may be obtained for laboratory confirmation. Referral to a primary care or genitourinary physician is appropriate. Patients and their partner(s) should be tested for other sexually transmitted diseases.4,5,11
Diagnosis. This is based on clinical findings, but more specific information can be obtained with a culture, Giemsa and gram stains.
We strive to provide comprehensive, complete eye care for our patients. By successfully diagnosing conjunctivitis, you can help to alleviate or even eliminate a condition that diminishes quality of life—garnering increased patient respect and, hopefully, a lifelong patient.
Table 2. Conjunctivitis Treatment Options | ||
| Type | Severity | Treatment |
| Allergic conjunctivitis | Mild | Allergen avoidance. Cool compresses. Artificial tears. |
| Moderate | Add dual-acting histamine receptor antagonist and mast cell stabilizer. | |
| Severe | Add topical corticosteroid. | |
| Bacterial conjunctivitis | Acute | Consider laboratory evaluation; treat empirically with broad-spectrum ophthalmic antibiotic for seven to 10 days. |
| Hyperacute (purulent) | Laboratory evaluation is imperative. Ceftriaxone, saline lavage of fornices Q1hr, followed by ophthalmic antibiotic. Corneal involvement requires hospitalization with IV antibiotics. Consider evaluating and treating for concurrent STDs. | |
| Chronic | Warm compresses and eyelid massage in addition to eyelid hygiene Topical antibiotic; consider an oral tetracycline. | |
| Viral conjunctivitis | Mild (PCF and nonspecific follicular conjunctivitis) | Cold compresses and artificial tears. Stress hygiene. |
| Severe (EKC) | Add ophthalmic vasoconstrictor, removal of membranes/pseudomembranes. Consider ophthalmic steroid, particularly if corneal involvement is noted. Ophthalmic Betadine early can decrease infectivity of free virus. | |
Dr. Bruce is an assistant professor of optometry at Northeastern State University’s Oklahoma College of Optometry in Tahlequah, Okla.
Dr. Bendure is an adjunct professor at Northeastern State University’s Oklahoma College of Optometry in Tahlequah, Okla.
1. Holland EJ, Mannis MJ, Barry LW, eds. Ocular Surface Disease: Cornea, Conjunctiva, and Tear Film. Philadelphia: Elsevier; 2013. |

