California Relaxes OD Regulations
New legislation significantly widens scope of practice.
By
Years of efforts by optometric advocates have paid off in California as Governor Jerry Brown recently signed a bill expanding optometry’s scope of practice. The bill permits California ODs with proper certification to use therapeutic pharmaceutical agents (TPA) in a number of new ways, including expansions on treating pain, hypotrichosis, glaucoma and blepharitis. The bill also permits optometrists to use noninvasive medical devices and technologies FDA indicated for conditions optometrists already treat; they can even employ some invasive procedures that require needles.
Bill Highlights
Specifically, the legislation focuses on TPA use in cases of blepharitis and hypotrichosis and prescribing Tramadol for up to three days. It also clarifies that certified ODs are permitted to prescribe currently allowable drugs “off-label.”
It opens up new diagnostic avenues for certified ODs, such as the ability to use intravenous injection for angiography, collect blood by skin puncture to test for diabetes, perform skin tests to diagnose ocular allergies and administer flu, shingles and pneumonia vaccines. Finally, ODs can now use a needle to remove foreign bodies and treat steroid-induced glaucoma.
Past Efforts
“California optometrists worked diligently over five years to advocate for scope of practice changes that strengthen our profession and our ability to care for Californians’ eyes,” said Sage Hider, OD, president of the California Optometric Association.1
Similar legislation proposed in the past faced adversity. A 2013 bill would have expanded the role of optometrists to diagnose and treat common systemic diseases, including diabetes, hypertension and hypercholesterolemia. It would have also authorized TPA use and removed limitations on the types of diagnostic tests ODs could order. By 2014 the bill merely authorized ODs to give limited immunizations before ultimately being pulled altogether.
Better Future
With this bill’s passage, California ODs can finally expand their scope of practice and better serve their patients.
“This important legislation is a step forward for the optometric profession, empowering doctors of optometry to more fully utilize our extensive training, education and experience to help expand eye and health care access,” Dr. Hider said.1
| 1. California Optometric Association. COA champions bill to expand optometric practice in California. October 9, 2017. |
Eye Dominance May Impact Dyslexia
Dyslexia, a significant problem for 5% to 17% of school-aged children, may have an ocular biomarker, according to new research.1 A recent study suggests the blue cone-free area at the center of the fovea is different in eyes of patients with dyslexia compared with eyes of those without the condition.2
Investigators in France studied 30 control patients without dyslexia and 30 subjects with dyslexia. While the controls all had asymmetrical blue cone-free areas—leading to the normal dominant/non-dominant relationship between the eyes—the same was not true for the 30 patients with dyslexia. Each of the 30 patients with dyslexia had symmetrical blue cone-free areas, causing an undetermined eye dominance.2
Without a dominant eye, the researchers speculate the patient’s brain is confused by the two different images, causing the characteristic blurring and distortion described by many dyslexic patients.2
While the study authors believe these findings suggest eye dominance as a possible cause for dyslexia, research has a long way to go before its true relationship to the diagnosis is understood.
“I’d say the findings may represent a comorbidity, as opposed to cause and effect,” says Bill Potter, OD, chief of Optometry and Contact Lens Services at Millennium Eye Care in West Freehold, NJ. Generally, “the brain is really good at suppressing the eye that is generating an aberrant image.” Thus, according to Dr. Potter, the research raises more questions than it answers, such as, “Does dyslexia in a one-eyed patient, or a 20/200 amblyope, differ from that of the binocular patient? Cause vs. comorbidity remains the question.”
More research is necessary to test this new theory—and work through all of the questions it raises, including possible treatment options.
1. Habib M, Giraud K. Dyslexia. Handb Clin Neurol. 2013;111:229-35. |
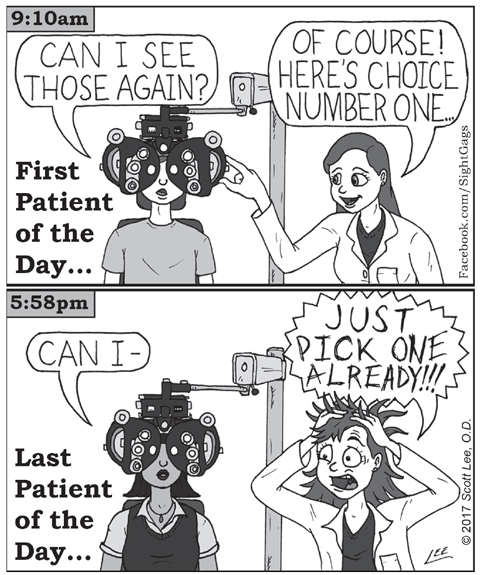 |
| Sight Gags By Scott Lee, OD. Click image to enlarge. |
Drug Patents Under Fire
Allergan continues the battle to protect its control of the patents for its dry eye drug Restasis, this time in the Eastern District of Texas, where a federal judge recently invalidated four key patents.1
In September, the company transferred the patents to the Saint Regis Mohawk Tribe in upstate New York in response to a patent challenge filed in an administrative proceeding with the United States Patent and Trademark Office. By paying the tribe to take possession of the patents and then leasing them back, the company hopes to capitalize on the tribe’s sovereign immunity to shield the patents from the challenge—a move met by criticism from Congress and consumer groups.1
Although the court case and the administrative patent challenge are separate proceedings, the Texas judge had harsh words for the company’s move to avoid repercussions of the patent challenge: “Sovereign immunity should not be treated as a monetizable commodity that can be purchased by private entities as part of a scheme to evade their legal responsibilities,” he wrote.1
The patent transfers have no bearing on the legal battle in Texas, where manufacturers continue to fight over the validity of the patents.1 If the ruling stands, the patents will be invalidated, regardless of the deal with the Mohawk Tribe.2
This recent push for a generic dry eye treatment option may not necessarily be in the patients’ best interest, however. Cost has always been a barrier to proper prescribing, according to Marc Bloomenstein, OD, director of optometric services at Schwartz Laser Eye Center in Scottsdale, Ariz., and “the notion that a generic is more cost-effective will definitely make clinicians more inclined to reach for a pen and Rx pad. However, the perceived cost benefit will come at the price of choice.” That choice, Dr. Bloomenstein says, is between a branded drug with “the best combination of molecule, strength and vehicle to maximize efficacy while minimizing side effects” and a generic drug with the same molecule but a different concentration and vehicle that lacks human testing to prove its efficacy.
“Optometry’s interest is centered around providing our patients with safe and efficacious medications to treat their conditions,” he says. “With this challenging disease, I worry that a generic market, without proper testing in humans, will dilute results and cause huge frustrations for doctors and patients.”
Those wary of a generic option can rest assured it’s far in the future still. Not only does Allergan plan to appeal the decision, but the Food and Drug Administration has yet to approve generic equivalents of Restasis, according to a press release.1
1. Thomas K. Patents for Restasis are invalidated, opening door to generics. New York Times. October 16, 2017. www.nytimes.com/2017/10/16/health/allergan-restasis-patent-.html. Accessed October 17, 2017. |
Potential DR Therapy
Scientists have identified a possible target for reducing dysfunctional blood vessel growth in diabetic retinopathy (DR). The researchers suspect a receptor stimulates glycolysis, which promotes pathological angiogenesis in retinopathies.1,2
| Patients with diabetic retinopathy may one day have a new therapy option. Photo: Mohammad Rafieetary, OD |
“If we block the adenosine receptor A2a, the blood vessels will not leak, and not as many new blood vessels will grow,” said Yuqing Huo, MD, PhD, chief of the Vascular Inflammation Program at the Vascular Biology Center at the Medical College of Georgia at Augusta University.1
Adenosine receptor A2a is found on the endothelial cells that line blood vessels. When oxygen levels are good, adenosine A2a receptor expression is low. But in diabetes, where oxygen levels go down, their expression increases.1 The increased expression “means repairing existing blood vessels and growing new ones in a process called angiogenesis,” said Dr. Huo. But when “cells don’t use energy efficiently or build blood vessels well, it’s actually called ‘pathological angiogenesis.’”1 With DR, the blood vessels “grow too much, too fast,” says Dr. Huo, leading to bleeding or contraction, and then to hemorrhage, retinal detachment and blindness.1
The researchers hypothesize that adenosine, via the A2a receptor, helps endothelial cells in the diabetic eye use glycolysis.2 The research shows that blocking glycolysis dramatically inhibits blood vessel proliferation and sprouting of endothelial cells that overexpress the receptor.1,2 When oxygen levels were more normal, deleting adenosine receptor A2a didn’t have that much impact on glycolysis, possibly because the receptor’s expression is not that high when oxygen levels are normal, the scientists suspect.1,2
Luckily, an adenosine receptor A2a inhibitor is already in clinical trials for Parkinson’s disease, paving the way for more studies.1
This is another fascinating scientific endeavor, says Mohammad Rafieetary, OD, of Charles Retina Institute in Germantown, Tenn. “Ultimately, diabetic retinopathy’s complications, which include vision loss, are primarily the result of hypoxia or ischemia.” Anything that can lessen this hypoxia-induced demise can help limit the degree and extent of the disease, which ends with loss of vision. “I am hopeful to see advancements in the basic science such as these translate into clinical applications.”
1. Baker T. Likely new treatment target identified for diabetic retinopathy. Jagwire News. October 2017. jagwire.augusta.edu/archives/48024. Accessed October 25, 2017. |
In the newsAfter analyzing medical records of 365 patients with posterior vitreous detachment (PVD) symptoms, Swedish researchers found those who sought care on the first day of their symptoms had a statistically significant higher risk of retinal tears. Those with only floaters and long duration of symptoms were lower-risk patients, the investigators said, emphasizing the importance of prompt referral for those with sudden onset of symptoms. Bond-Taylor M, Jakobsson G, Zetterberg M. Posterior vitreous detachment - prevalence of and risk factors for retinal tears. Clin Ophthalmol. 2017;2017(11):1689-95. Studying a child’s central inner retinal function may be a future predictive measure for myopia, according to a new study. Investigators measured cycloplegic refraction and axial length and took a global flash multifocal electroretinogram at baseline for 56 emmetropic children ages six to nine. The 43 children with myopic changes on follow up also had reduced response in the central inner retina. Because this reduced response preceded the myopia, the researchers speculate this might be an inducement to myopia, not a secondary effect. Li SZ, Yu WY, Choi KY, et al. Subclinical decrease in central inner retinal activity is associated with myopia development in children. Invest Ophthalmol Vis Sci. 2017;58(10):4399-4406. New research found epithelium-off 15mW accelerated crosslinking pulsed-light therapy stabilized progression and improved vision in patients with stage two keratoconus. The researchers suggest this treatment modality reduces treatment time, increases patient comfort and reduces post-op glare, subepithelial nerve plexus damage and postoperative haze. Mazzotta C, Baiocchi S, Bagaglia SA, et al. Accelerated 15 mW pulsed-light crosslinking to treat progressive keratoconus: Two-year clinical results. J Cataract Refract Surg. 2017;43(8):1081-8. |

