 |
During a medical exam, an internal medicine doctor noted a difference in pupil size—left pupil larger than right—in a 62-year-old Caucasian male, which was never noted on prior visits. In addition to a referral to our clinic, his internist scheduled him to have an intracranial magnetic resonance imaging (MRI) and angiography (MRA).
The patient himself was unaware of this change; however, upon questioning he noticed increased light sensitivity out of the left eye for at least three months. He denied any other neurologic issues or symptoms. His medical history was remarkable for hypothyroidism and high cholesterol and was taking levothyroxine and atorvastatin. He denied ever using any motion sickness patches or over-the-counter eye drops.
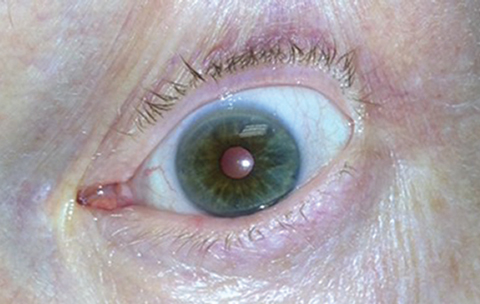
The patient’s best-corrected visual acuities were 20/25 in each eye. Pupils measured 3mm OD and 4.5mm OS in bright light and 7.5mm OD and 7.5mm OS in dark light. Reverse flashlight testing revealed no afferent pupil defect. Extraocular muscles were full and smooth. No third, fourth or sixth nerve palsy or other neurologic deficit was noted. Anterior segment exam was remarkable for 2+ nuclear sclerosis. When examining the pupils under the slit lamp, the right pupil showed an even and normal constriction and dilation when turning the slit beam on and off. However, the left eye showed a generalized sluggish constriction as well as sectoral iris paralysis temporally (Figure 1). Posterior segment exam was unremarkable. No disc edema, disc pallor, artery or vein occlusions existed and the retina was flat and attached.
The Verdict: Tonic Pupil
The history and clinical findings were most consistent with a tonic pupil. We instilled 0.125% pilocarpine in the left eye, which, after 30 minutes, constricted the pupil to 3mm, confirming the diagnosis (Figure 2). We discussed the tonic pupil with our patient as well as informing his physician. Our patient was otherwise in good general health and no further workup was necessary. The MRI and MRA were subsequently cancelled. He was very minimally bothered by the light sensitivity and wears sunglasses when needed.
 |
| Fig. 1. The pupils of both eyes in bright light measuring 3mm and 4.5mm in the right and left eyes, respectively. Click photo to enlarge. |
Discussion
Often, patients who present with an acute isolated dilated pupil are put through extensive and unnecessary testing and referrals. Clinicians fear there is a serious underlying etiology when the majority of causes for acute isolated dilation are benign; these include tonic pupil, pharmacologic dilation and transient pupillary mydriasis.
By far the biggest fear of a patient presenting with a dilated pupil is a third nerve palsy. Although in theory a compressive lesion of the third nerve may cause an isolated dilated pupil without any extraocular motility deficit or eyelid ptosis, in practice this rarely occurs.1 In these rare cases of third nerve palsies presenting initially with only pupillary involvement, a review of the literature found that these patients also either presented with headache, seizure or other neurological deficits, or the extraocular motility deficits developed early in the course of their illness.2,3
Tonic pupil, as seen with our patient, is a common cause of isolated pupil dilation. Clinical features include diminished or absent pupillary reaction to light stimulus, segmental iris paralysis, no afferent pupillary defect by reverse flashlight testing and preserved constriction to accommodation.1,2 Most commonly seen in women ages 20 to 40, tonic pupils arise from damage to the ciliary ganglion, the cause of which is rarely identified.2 In response to this damage, aberrant regeneration of fibers originally destined for the ciliary body instead innervate the iris sphincter.2 This results in diminished response to light and an enhanced tonic reaction to accommodation.1
When this aberrant regeneration is restricted to certain segments of the iris, sectoral iris paralysis occurs.1 This phenomenon is best seen under the slit lamp while focusing on the iris and turning the slit beam on and off. Additionally, because the ciliary ganglion is now denervated, it generates more postsynaptic acetylcholine receptors, allowing for such a low dose of pilocarpine to cause pupillary constriction.1 Pilocarpine is not formulated in 0.125% concentration; however, it can easily be made in office by mixing one drop of 1% pilocarpine to seven drops of any artificial tear. A tonic pupil is generally a benign condition and no further workup is necessary; however, the presentation has been reported in patients with connective tissue disorders, temporal arteritis and orbital trauma.
 |
| Fig. 2. In the same patient, we observed constriction of the left pupil 30 minutes after instilling 0.125% pilocarpine. Click photo to enlarge. |
Differential Diagnosis
When pharmacologic pupillary dilation is suspected, a careful and thorough history will often reveal the source. Anticholinergic agents such as scopolamine patches and pesticides as well as various over-the-counter eye drops containing mydriatic properties can all cause pupil dilation. If no agent is identified during questioning, 1% topical pilocarpine can be instilled to test for pharmacologic blockade. A pupil that is dilated due to pharmacologic blockade will not constrict to the pilocarpine, but one dilated secondary to a third nerve palsy will.1,2 The effects of pharmacologic pupil dilation are transient and the pupil will return to its normal size in a relatively short time frame.
Transient pupillary mydriasis or episodic mydriasis has been observed in patients with a history of migraine.1 One report looked at 24 patients who presented with episodes of transient pupillary mydriasis.4 Nineteen patients were female, 14 had a history of migraines and the median age was 31.4 The median duration of the episodes was 12 hours with a frequency of two to three episodes per month.4 No underlying neurological disorders were identified in any subjects after testing and workup.4 If the transient or intermittent nature of these episodes can be established either by the patient’s medical history or observed during clinical evaluation in isolation without any other findings, they generally do not require any additional workup or neuroimaging.1
While isolated acute pupillary dilation can be alarming at first, it is almost always the result of a more benign process. The main concern with this finding is to ensure it is not in association with a third nerve palsy. That is why clinicians must review and understand the various clinical features of these other benign disorders to save the patient from undergoing various unnecessary testing and anxiety.
| 1. Moeller JJ, Maxner CE. The dilated pupil: An update. Curr Neurol Neurosci Rep. 2007 Sep;7(5):417-22. 2. Taber KH, Hayman LA, Tang RA. A guide to the isolated dilated pupil. Arch Fam Med. 1997 Jul-Aug;6(4):385-8. 3. Wilhelm H, Klier R, Tóth B, Wilhelm B. Oculomotor nerve paresis starting as isolate internal ophthalmoplegia. Neuro-Ophthalmology. 1995;15:211-5. 4. Jacobson DM. Benign episodic unilateral mydriasis. Clinical characteristics. Ophthalmology. 1995 Nov;102(11):1623-7. |

