 |
A 15-year-old teen presented for a routine examination with complaints of decreased vision in the left eye for many years. He received his first pair of glasses at age nine from another clinician. His relevant measurements included: plano OD, +4.50 OS, giving a visual acuity of 20/20 OD and 20/60 OS. He was instructed to use the glasses and return in six weeks to evaluate patching therapy but was not seen back until the current visit—six years later.
He reports receiving average grades in school, ranging from A to C. The patient recorded a 4 on the Quality of Life checklist. This subjective survey consists of 19 items assigned point values ranging from 0 to 4, with 0 indicating the patient never experiences difficulty and 4 indicating the patient always experiences difficulty. A score of 20 is typically indicative of a learning-related vision disorder.
Many times, children who are not engaged in schoolwork and are avoiding visually demanding activities will have a low score. If they were still trying at school work, the score would often be much higher. But, this case offers a different explanation.
 |
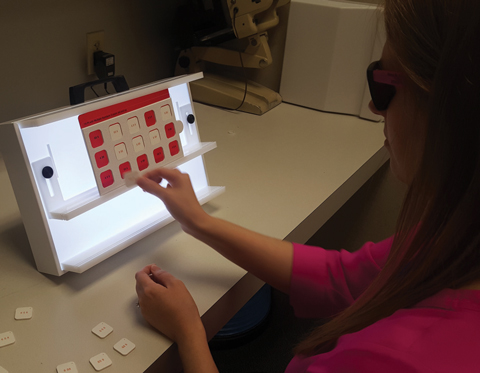 |
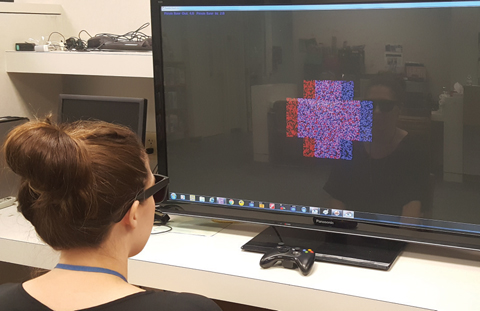
| At top, binocular activities using the VisionBuilder program are a great way to enhance patient cooperation. At bottom, The MFBF Matching Game is used as a precursor to binocular activities to ensure the elimination of suppression. |
Exam
The uncorrected Snellen acuities were 20/15, 20/100, 20/15 at distance and 20/40, 20/200, 20/15 at near. The previous glasses were lost within weeks of the last examination, six years prior. Stereopsis showed 50 seconds of arc on Wirt circles but nothing on global forms. This is a conundrum; however, the best explanation is that the patient used monocular cues to determine and report which circle was popping out and got lucky reporting towards the higher levels of stereopsis.
“Just look retinoscopy” showed a significant difference in the quality of the patient’s reflexes, as the left eye showed a dingier, dirtier reflex.
Retinoscopy at distance was +0.50 OD, +5.00-1.00 X 180 OS. This provided acuities of 20/20 OD and 20/40 OS at distance and near. To use the least amount of lens power to obtain the best visual performance, we determined that plano OD (20/20), +4.00 OS (20/40) was the appropriate starting point.
We considered Worth’s 4-dot testing which, in bright and dim illumination, did not show suppression. This was an improvement. We observed no enhancement in stereopsis; however, this may have been because the patient’s primary strategy was to use monocular cues, which were unchanged. Over time, as the patient learns to use his binocular system in a more balanced way, he should perform much better on stereo testing.
The low score on the symptomsurvey makes more sense now—suppression is a wonderful patient adaptation to reduce double vision and other binocular-related issues.
Diagnosis
The patient was diagnosed with anisometropic amblyopia in his left eye. The initial treatment included a contact lens fitting to reduce the image size, improve comfort and increase the field of clarity. Spectacles would of course be prescribed as backup, as it is the standard of care. After fitting with a standard two-week disposable in the left eye, the acuity remained at 20/40 at distance and near.
The next step in the treatment sequence in many offices would normally be two hours of patching, five days a week. Due to the growing evidence base (see, “A Fine PEDIGree” below), we decided to forego patching and take a binocular approach using vision therapy. As amblyopia is more than simply an acuity issue, this approach would improve accommodation, binocularity and eye movements; additionally, it would break suppression. The global view of the treatment was aimed at improving the visual system and how the patient integrated his vision with his other sensory systems, creating a system in which vision is guiding and dominant. We estimated that between 35 to 40 sessions of weekly vision therapy with home-based support was required, in this case, to ensure success.
A Fine PEDIGreeTreating amblyopia without patches was pioneered and improved by many optometrists more than 50 years ago. Research is critical to refining and understanding the scientific why behind the innovative methods of the past’s refractive experts and innovators. Over the past 20 years, the Pediatric Eye Disease Investigator Group (PEDIG) has provided this necessary research; ultimately, it has shattered and changed the main premise of the classical amblyopia treatment approach. Due to the multi-centered research, we now know the following:1 • Full-time patching is equal to six hours in severe amblyopia. • Six hours is equal to two hours of patching in moderate amblyopia. • One drop of atropine once a day is equal to six hours of patching in severe cases of amblyopia. • Occlusion foil patching is equal to using an opaque patch in moderate amblyopia. The research showcased too many discoveries to list. It’s thrilling to see that researchers are addressing the concept of throwing patches and drops out the window in favor of binocular therapy. In a recent study, the PEDIG group compared a binocular iPad game with patching in patients ages 5 to 13. The study found a 2.5- and 2.8-line improvement in acuity in a group of 5 to 7-year-olds but overall, only 22% in the game group completed greater than 75% of the treatment time (60 minutes per day). In the entire treatment group of 385 children, the acuity improved 1.05 lines in the binocular iPad group vs. 1.35 in the patching group at 16 weeks.2,3 The study determined the lack of participation was, in essence, because the game was too boring. A new study in the works vies for greater compliance with an interactive game called Dig Rush.2 PEDIG researchers will determine the impact of 60 minutes of game play five day per week while using the prescribed glasses vs. only the prescribed spectacles.2 Practitioners are looking forward to these results to give further evidence for the binocular approach many practitioners currently employ in their treatment protocols. 1. Hendricks DH. Rethinking conventional wisdom on amblyopia. Rev Opthalmol. 2013;20(12):44-6. |
Follow-Up
After 35 sessions of vision therapy, the patient’s acuities were 20/15, 20/20, 20/15 at distance and 20/20, 20/20, 20/10 at near. Stereopsis was demonstrated at 25 sec of arc on Wirt circles and the patient was able to see the global forms.
In this case, a teen was treated with a mixture of spectacles, contacts and vision therapy to obtain the desired outcome. While the standard of care has shifted over the past 20 years and the standard remains patching on some level, the binocular approach acts to both improve acuity and enhance all other visual skills, including binocularity. It leads to both short and long-term gains and, in our clinical experience, reduces regression (the tendency for those treated with patches only to lose their gains over time).
If your office is not able to tackle amblyopia and, taking it even further, strabismus, using the binocular approach, reach out to the doctors in your area that use the binocular approach every day. Simply use the doctor locator options on the pages for the Optometric Extension Program Foundation (oepf.org/page/map) or the College of Optometrists in Vision Development (locate.covd.org). We promise that your patients will thank you for taking this step to ensure their visual health and long-term success.

