Rare Condition, Not-so-rare Therapies
Precision eye care is in the pipeline—and may suggest surprising treatment strategies.
By
Patients with rare eye conditions such as neovascular inflammatory vitreoretinopathy (NIV) often have limited therapeutic options, especially when conventional treatments fail. But researchers at the Stanford University School of Medicine are looking to change that with precision medicine. They turned to proteomics to better identify molecular pathways in NIV pathologies—and available potential targets for therapy.
Using liquid biopsies, the investigators tested for expression of 200 cytokine-signaling proteins and found 64 that were different, 61 of which were upregulated.
“By performing a proteomic evaluation of an ocular sample in a disease state, and determining up-or down-regulation of specific molecules, like cytokines, ideal treatable targets can be identified,” says Jessica Steen OD, an assistant professor at Nova Southeastern University. Several from this study show promise:
Anti-vascular endothelial growth factor (VEGF). After noting elevated VEGF, the researchers tried intravitreal Avastin (bevacizumab, Genentech) in seven eyes. In each case, the vitreous hemorrhage grade resolved without surgery and the patients’ vision returned to baseline.
Methotrexate. The proteomic data suggested the significant role played by the mTOR and class I PI3K signaling pathways, which are critical in the development of T-cells. Thus, the researchers used intravitreal injections of methotrexate, and the number of cells in the anterior chamber dropped dramatically in five eyes with Stage II and Stage III NIV.
Corticosteroids. Because the personalized proteome revealed upregulated cytokines that should be quelled by corticosteroids, the researchers used a fluocinolone acetonide (Retisert, Bausch + Lomb) implant in three eyes to mitigate the adverse effects of oral therapy such as weight gain and osteoporosis. They were able to reverse several clinical features such as retinal neovascularization for three years.
Anti–IL-6. Some study participants continued to have elevated IL-6, possibly responsible for their severe intraocular fibrosis, according to the researchers. For one patient with retinal fibrosis following retinal detachment repair surgery (causing re-detachment), the researchers tried monthly intravenous infusions of tocilizumab (anti–IL-6) over six months post-reattachment surgery. The new treatment allowed her retina to remain attached—a first for reattachment surgery in an NIV patient, the researchers wrote.
They also found TNF-α was not elevated, which explains why infliximab (anti-TNF-α) infusions hadn’t alleviated patient symptoms.
These new findings hold promise for future strategies for NIV and, one day, other ocular conditions.
“Looking ahead, the goal of ophthalmic precision medicine will be to use proteomics and genetic evaluation to predict disease course and prognosis and to determine ideal therapies for patients with a wide range of conditions, including glaucoma, diabetic retinopathy and age-related macular degeneration,” according to Dr. Steen.
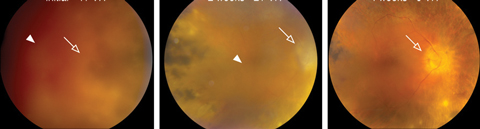  |
| This patient with Stage III NIV has significant vitreous hemorrhage (arrow heads) and vision reduced to count fingers. At left is initial presentation, while the middle and left images are two and four weeks after Avastin injection, respectively. At two weeks, the vitreous hemorrhage was resolved and vision improved to 20/70. By four weeks, vision was 20/50 and the optic nerve head (open arrow) is visible. Click image to enalrge. Photo: Vinit B. Mahajan MD, PhD |
Of course, research has a long way to go before this technique achieves a wider application, considering the variability and genetic complexity in most ocular diseases.
“The authors had the advantage of reducing the variation of gene expression between individuals, as the family of patients studied all had the identical genetic variant resulting in NIV,” says Dr. Steen. “This is not the case in multifactorial retinal conditions such as diabetic retinopathy and macular degeneration, which are a result of multiple genes, many gene products and their interaction with environmental and metabolic factors.”
But one thing is for sure: the potential of precision medicine is closer than ever before.
AMD Assessment Made Easy
Clinicians looking for a simple way to assess a patient’s risk for age-related macular degeneration (AMD) can consider adding a new tool to their practice. Researchers from Italy and France have created the simplified Théa AMD risk-assessment scale (STARS), a 13-item questionnaire that includes risk factors such as age, ethnicity, family history, body mass index, smoking habits, hypercholesterolemia, hypertension and myocardial infarction.
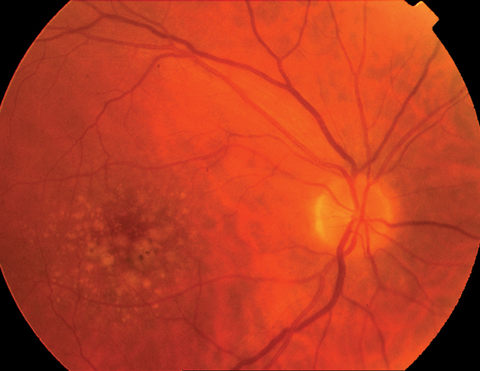 |
| A new questionnaire may help clinicians catch early forms of dry AMD, as seen here. |
“Strengths of this questionnaire are that it can be administered quickly, is validated by an external population and includes many of the risk factors widely considered to be associated with, if not causally linked to, the development of AMD,” says Andrew J. Rixon, OD, of the Memphis VA Medical Center. “While this questionnaire does not contain novel information, it streamlines the risk assessment process in a meaningful way.”
Based on data from 12,639 patients in Italy and 6,897 patients in France, the questionnaire provides an opportunity to increase awareness through AMD public health initiatives, which “ideally results in patients at all risk levels seeking appropriate comprehensive eye care,” Dr. Rixon says. “The earlier the patient and practitioner are aware of risk, the greater the chance for reduction in loss of function.”
While useful, the questionnaire should help inform the broader assessment of the patient, not replace it, Dr. Rixon stresses. “Funduscopic evaluation, cross sectional macular analysis by OCT, fundus autofluorescence and knowledge of the patient’s nutritional status, among others, still supplant strict interpretation of a risk questionnaire in the decision making process.”
| Delcourt C, Souied E, Sanchez A, et al. Development and validation of a risk score for age-related macular degeneration: The STARS questionnaire. Invest Ophthalmol Vis Sci. 2017;58(14):6399-6407. |
SECO, VEE Kick Off 2018 Conference Season
The first quarter of 2018 is packed with educational opportunities for optometrists. Two of the biggest shows interrupt the late-winter blues with CE sessions, learning labs, workshops, specialty tracks, business programs and more: SECO in late February into early March and Vision Expo East just two weeks later. Here’s a look at what each one offers so you can show up prepared:
Atlanta-bound
At the SECO Annual Congress in Atlanta Feb. 28 to March 4, you can expect to hear and learn from some of the most respected eye care practitioners in the profession.
“SECO has changed the game when it comes to value for the dollar and invaluable information that can be put to immediate use,” says Paul C. Ajamian, OD, SECO optometric education program committee chair. “With all-new tracks like ‘Squawk Box’ and ‘Snap Chat’ plus attention to specialized topics like MRSA, GCA and TBI, SECO provides custom-crafted courses, special sessions and learning labs available nowhere else in eye care.”
Here are some conference highlights you won’t want to miss:
MedPro360. Learn proven business management strategies from pros like management consultants Jenn Lim of Delivering Happiness and Donald Miller of Storybrand, plus HGTV’s Vern Yip.
Gear Up for Glaucoma! James Thimons, OD, and Robert Noecker, MD, will provide an in-depth look at the new diagnostic and management technologies and pharmaceutical agents revolutionizing glaucoma care, now and in the future.
Eye Cancers: From Melanoma to Retinoblastoma. J. William Harbour, MD, will discuss diagnostic techniques, differentials, treatment, outcomes and breakthroughs for patients with uveal melanoma and retinoblastoma.
Anterior Segment Solutions. Zaina Al-Mohtaseb, MD, will discuss diagnosing infectious and non-infectious keratitis through cases and videos. He will also touch on cataract surgery in patients with corneal disease and secondary and presbyopia-correcting IOLs.
Retina 2018. Jay Haynie, OD, and Ali Zaidi, MD, will highlight OCT angiography and its role in primary eye care in 2018. Attendees will also hear about the latest clinical trials regarding AMD and diabetic retinopathy.
Cornea Update. Joe Shovlin, OD, FAAO, and Andrew Bartlett, MD, will explore the epidemiology and pathogenesis of ulcerative keratitis.
Secrets of a Vascular Surgeon. Brad R. Grimsley, MD, FACS, will provide an in-depth look at extracranial cerebrovascular occlusive disease as it relates to vision.
For more information or to register, go to attendseco.com.
The Big Apple
New York City’s Jacob Javits Center will welcome thousands of optometrists, opticians and industry executives on March 15 for the International Vision Expo & Conference East (VEE), which runs until the 18th.
Hosted by Reed Exhibitions and the Vision Council, VEE boasts a line-up of heavy hitters on the CE lecture circuit and all-new learning opportunities.
“For the first time, at Vision Expos East and West 2018, we’ll be providing our education attendees with hands-on training in some of today’s most important topics,” says Dr. Gaddie, co-chairman of the conference advisory board. “Our new optical coherence tomography workshop provides the opportunity to work with the latest diagnostic equipment and hear best practices direct from the experts. We’ll also have a new scleral lens workshop, allowing first-hand experience with new techniques as specialty contact lenses gain more traction with optometry.”
Here are some of the must-see sessions at VEE 2018:
Aesthetics Track. Patients are always searching for ways to look younger. Learn how to implement an ocular aesthetics model into your practice and help make their dreams a reality.
Specialty Lens Track. Attendees will hear a comprehensive discussion of specialty lens fitting and evaluation.
Global Contact Lens Forum. This “meeting within a meeting” will deliver the latest insights and solutions used by today’s contact lens practitioners, with a focus on business and growth strategies.
OptiCon. In 2018, OptiCon officially joins the VEE line-up, offering educational programming that will cover four key areas: spectacles, contact lenses, business and exam review. Attendees will also be able to take ABO and NCLE review courses and sit for the exams.
Additional courses throughout the conference will cover all the skills and responsibilities an optometrist is tasked with today—and tomorrow.
For more information or to register, go to east.visionexpo.com.
In the newsResearchers have found an improved gene therapy delivery mechanism that might aid in future glaucoma treatments. By blocking proteasomes when using the feline immunodeficiency virus to deliver marker genes, they found it roughly doubled the transfer of genes entering the trabecular meshwork cells. Such improved delivery methods could boost the efficacy of future gene therapy for glaucoma, the researchers said. Aktas Z, Rao H, Slauson SR, et al. Proteasome inhibition increases the efficiency of lentiviral vector-mediated transduction of trabecular meshwork. Invest Ophthalmol Vis Sci. 2018;59(1):298-310. Eye injuries related to paintball or BB and pellet guns more than doubled from 1990 to 2012, a new study found. Although the injury rate has slightly declined for all sports in this time, these gun injuries accounted for almost half of all hospitalizations, data from the National Electronic Injury Surveillance System revealed—highlighting the need for better prevention efforts for patients participating in air-gun related recreation. Miller KN, Collins CL, Chounthirath T, et al. Pediatric sports- and recreation-related eye injuries treated in US emergency departments. Pediatrics. 2018;141(2):e20173083. [Epub]. After undergoing an extensive, voluntary review process, the Council on Optometric Practitioner Education (COPE) CE accreditation has been deemed “substantially equivalent” to the Accreditation Council for Continuing Medical Education’s CME accreditation requirements, criteria, policies and decision-making process for medical practitioners. Such distinction creates a path for shared inter-professional education, leading the way forward for optometry to become a substantial and accepted part of a larger healthcare system, according to COPE. |

