 |
A 72-year-old Hispanic female presented to our office for her postoperative eye exam. She had undergone an uncomplicated cataract surgery along with intraocular lens (IOL) implantation four weeks earlier in her left eye.
The right eye had prior cataract extraction approximately eight weeks earlier. She was extremely happy with her visual outcome and had stopped using her drops.
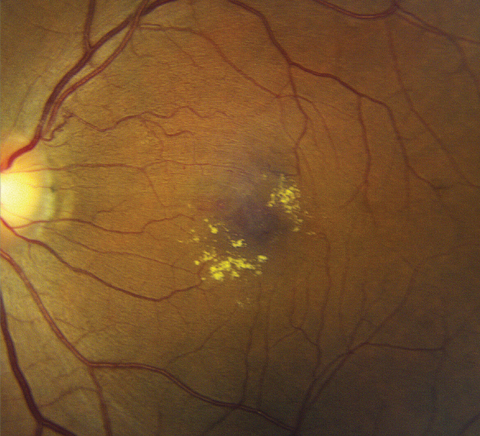 |
| Posterior pole image of the left eye of our patient. How do you explain these finding in a patient who recently had cataract surgery? |
Evaluation
On exam, her best-corrected visual acuity was 20/20 OD, 20/30 OS. Confrontation fields were full-to-careful finger counting in both eyes. The pupils were equally round and reactive to light. There was no afferent pupillary defect.
Anterior segment examination was significant for posterior chamber IOL implants that were well centered and clear visual axes.
Dilated fundus exam showed moderate-sized cups with good rim coloration and perfusion in both eyes. The right eye was completely normal. Upon exam, the left eye showed changes.
Optical coherence tomography (OCT) and optical coherence tomography angiography (OCT-A) images were also obtained and are available for review.
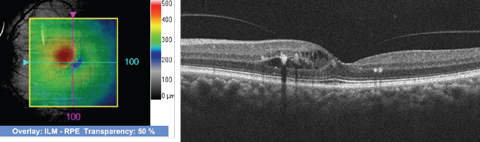 |
| SD-OCT images through the macula of the 72-year-old patient’s left eye. Click image to enlarge. |
Take the Retina Quiz
1. What do the yellow changes in the macula represent?
a. Drusen.
b. Lipofuscin.
c. Hard exudate.
d. Calcium.
2. How would you characterize the spectral-domain OCT?
a. Localized ischemia.
b. Intraretinal neovascularization.
c. Macular thickening with intraretinal fluid.
d. Macular thickening with subretinal fluid.
3. Based on the clinical appearance, what is the overall diagnosis?
a. Coats’ disease.
b. Macular telangiectasis.
c. Branch retinal vein occlusion.
d. Irvine-Gass Cystoid macular edema.
4. How should this patient be managed?
a. Focal laser treatment to the macula.
b. Intravitreal kenalog.
c. Intravitreal anti-VEGF injection.
d. Observation.
For answers, see below.
Discussion
The yellow precipitates in the macula represent hard exudate. On clinical exam, it was evident that the macula was thickened and there was edema. The spectral domain optical coherence tomography (SD-OCT) confirmed retinal thickening as well as intraretinal fluid and mild cystoid macular edema. The 3D thickness map highlights this nicely, where the red area represents a localized area of retinal thickening.
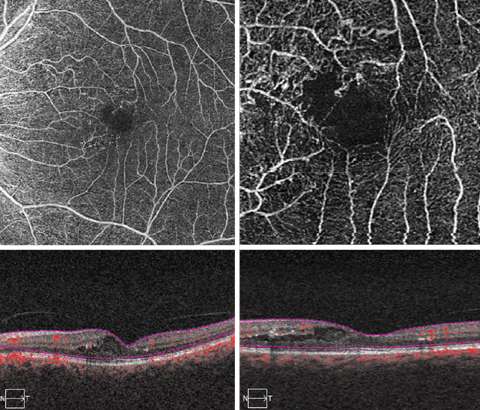 |
| These OCT-A scans show our patient’s macula in great detail. Click images to enlarge. |
Diagnosis Decisions
So, what is going on with our patient? Are these changes related to her cataract surgery? The OCT-A provides some valuable insight as to the cause. Microvascular changes are clearly visible on the OCT-A scan as well as some collateral vessel formation around the superior portion of the foveal avascular zone.
Based on these findings, we can surmise that our patient has a small branch retinal vein occlusion (BRVO). Another clue to this etiology is the presence of the anomalous vessel superior to the disc that can be seen in the color fundus photo. It looks like it may be a dilated collateral vessel. Perhaps this is the location where the occlusion occurred.
It’s difficult to know for how long she has had the occlusion or where she is in the course of the disease. It was not present two months prior when she was being examined for her cataracts. The usual presentation of BRVO is a triangular or wedge-shaped area of hemorrhage that extends beyond the site of where the artery crosses the vein. Our patient doesn’t have that. This could be because it is almost resolved and we are seeing her in the resolution phase, or because it was a very mild retinal vein occlusion to begin with.
As the hemorrhage from the occlusion resolves, there are still some leaking and incompetent retinal vessels that are releasing exudate that extends into the macula, resulting in macular edema. One thing is for certain: it’s not related to her cataract surgery.
There is a strong association between hypertension and the development of retinal vein occlusion. Our patient does, in fact, have hypertension, but it is well controlled with Norvasc (amlodipine, Pfizer) and hydrochlorothyiazide. So, is the small BRVO a result of her high blood pressure? It is impossible to know the true effect of the patient’s hypertensive status on her vision because approximately half of all patients with RVOs have hypertension. Regardless, it is important that the hypertension be controlled.
Management
Anti-VEGF therapy has emerged as the standard of care in treating macular edema associated with retinal vein occlusions. Lucentis (ranibizumab, Genentech), Avastin (bevacizumab, Genentech) and Eylea (aflibercept, Regeneron) are all potential treatment options for our patient.
Even though our patient has mild macular edema and this condition could resolve on its own, we referred her to the retinal specialist for consideration of treatment.
| 1. Interim Guidelines for Management of Retinal Vein Occlusion; Royal College of Ophthalmologists (December 2010). www.rcophth.ac.uk/wp-content/uploads/2015/07/Retinal-Vein-Occlusion-RVO-Guidelines-July-2015.pdf. Accessed: December 15, 2017. |
Retina Quiz Answers
1) a; 2) c; 3) d; 4) d.

