 |
A 38-year-old female presented to the eye clinic complaining of progressive blurred vision in the right eye. She had a long-standing medical condition directly related to her retinal diagnosis. She also had a strong family history of cancer—her paternal grandmother had breast cancer, her maternal grandmother had pancreatic cancer, her maternal grandfather had pheochromocytoma and her father had gastric cancer.
Upon examination, her visual acuities were 20/30 OD and 20/20 OS with no improvement after refraction. Her extraocular motilities showed full range of motion, her confrontation fields were full to finger counting in both eyes and her pupils were round and reactive to light with no afferent defect. Her intraocular pressures were 20mm Hg OD and 19mm Hg OS.
Anterior segment exam in both eyes and left eye fundus exam were unremarkable. But the fundus exam in her right eye (Figure 1) was notable. A widefield image of the retina was also taken (Figure 2), as well as an OCT of the peripapillary region (Figure 3). We also had an intravenous fluorescein angiography (FA) from a previous encounter (Figure 4).
 |
| Fig. 1. This fundus photo shows the optic nerve and macula of the 38-year-old patient’s right eye. Click image to enlarge. |
 |
| Fig. 2. Note the peripheral changes in this widefield view of the same eye. Click image to enlarge. |
Take the Quiz
1. What is the diagnosis of this retinal tumor?
a. Retinal capillary hemangioma.
b. Cavernous hemangioma.
c. Astrocytic hamartoma.
d. Infectious granuloma.
2. Which medical condition is mostly associated with the retinal tumor?
a. Tuberous sclerosis.
b. Neurofibromatosis.
c. Von Hippel-Lindau disease.
d. Sarcoidosis.
3. Which other vital organ can be associated with this condition?
a. Brain.
b. Kidneys.
c. Adrenal glands.
d. All of the above.
4. Which option is to be considered for the treatment of these retinal tumors?
a. Laser photocoagulation.
b. Photodynamic therapy.
c. Observation.
d. All of the above.
For answers, see below.
Diagnosis
Our patient had a juxtapapillary retinal capillary hemangioma (RCH) that was previously treated with photodynamic therapy (PDT) in 2013 but since developed exudates nasal to the fovea. In addition, the patient also had a superior RCH with marked exudation and another RCH located inferotemporally with mild exudates that was previously treated with argon laser photocoagulation in 2012 and 2013 (not shown on fundus images).
Upon reviewing the previous images, we noticed the FA displayed early hyperfluoresence in both the juxtapapillary tumor and inferotemporal tumor with prolonged intensity and minimal leakage. The OCT of the peripapillary region of the tumor (Figure 3) displays intraretinal fluid and thickening that was not present in the earlier visit.
The compilation of the findings of the fundus images in comparison with previous studies led us to conclude the patient had developed a new RCH in the superior periphery with significant exudation and that the previous juxtapapillary RCH had newly developed leakage.
Discussion
Retinal capillary hemangioma is a benign vascular tumor that extends from the inner retina towards the retinal surface. These RCHs can leak fluid and result in exudative retinal detachments. They are typically described as pink lesions often accompanied by an afferent feeder vessel and an efferent draining vessel to and from the lesion.
RCH can be unilateral or bilateral. One study shows bilateral lesions occurred in 57.9% (unilateral 42.1%) of patients and that 84.7% of the retinal lesions were located in the periphery—the rest were located in proximity to the optic nerve.1 Although RCH can be an isolated sporadic lesion, it is highly associated with our patient’s long-standing systemic disease, von Hippel-Lindau (VHL) disease, a multisystem cancer syndrome that can lead to the development of both benign and malignant tumors. A positive familial history of VHL and the existence of RCH are the diagnostic criteria for VHL syndrome.2 Without a family history, a person with RCH must also have multiple RCHs in the eye or a hemangioblastoma of the central nervous system in order to meet the criteria.2
VHL is inherited through an autosomal dominant fashion and is caused by a mutation in the VHL tumor suppressor. The prevalence is approximately one in every 36,000 births, and penetration is nearly complete by age 65.2 Approximately half of VHL cases are familial, with the other half being sporadic due to new mutations. VHL disease is a highly diverse condition that presents itself with more than 40 types of lesions being described in 14 different organs, including retinal capillary hemangiomas, cerebellum or spinal hemangioblastomas, renal pheochromocytomas and carcinomas.2 The tumors associated with the highest mortality are renal carcinomas and cerebellum/spinal hemangioblastoma—which is why patients require periodic imaging and should be closely monitored by multidisciplinary medical clinicians.3
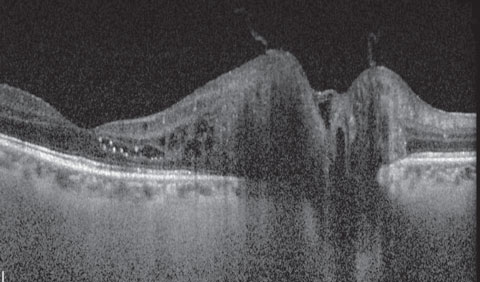 |
| Fig. 3. What can be gleaned from this OCT scan of the optic nerve and macula? Click image to enlarge. |
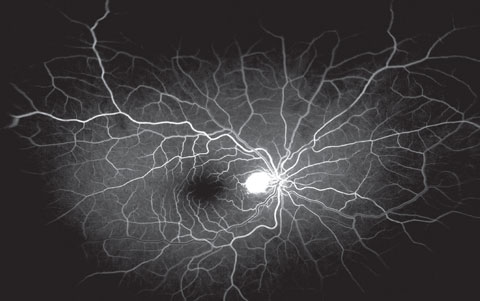 |
| Fig. 4. This is the early venous phase of the fluorescein angiogram of our patient—note the hyperfluorescent lesion involving the optic nerve. Click image to enlarge. |
Management
Many proposed treatments exist with RCH, but the efficacy of treatment, as well as the indications for treatment, are based on the tumor’s location, size and associated findings. Close observation is often the case for peripheral lesions less than 500µm with no associated exudation, as these peripheral lesions can remain fairly stable.4 Observation is also indicated for juxtapapillary lesions that do not have active leakage, as they can have a natural history of stability and other alternative treatments may lead to negative sequelae.5,6 Argon laser photocoagulation has been indicated for peripheral lesions less than 3mm with no subretinal fluid.7 The photocoagulation itself can either be targeted at the tumor, the feeder vessels or both and has been reported to be 91% to 100% effective in preserving visual acuity at a mean follow-up time of 5.1 years.7 This treatment is particularly effective for tumors that are 1.5mm or smaller.7,8 Cryotherapy is an alternative treatment that is proposed when tumors are more anteriorly located, have a moderate degree of subretinal fluid or are larger than 3.0mm.9
Furthermore, research shows photodynamic therapy may induce the occlusion of both juxtapapillary and peripheral retinal capillary hemangiomas and can lead to the cessation of leakage.10
Anti-VEGF therapy has been tried with both peripheral RCH and juxtapapillary RCH with mixed results. Unfortunately, no large clinical trial has yet examined the efficacy of anti-VEGF agents in the management of VHL patients. In small pilot studies, there has been some success on decreasing exudation, but the anti-VEGF drugs did not seem to have an effect on reduction in the tumor size.11
For our patient, both her superior peripheral RCH and juxtapapillary RCH were treated. An argon laser photocoagulation was performed in the superior retinal tumor, which led to the retraction of lipid exudation by the following visit. Furthermore, a half-fluence photodynamic therapy was conducted at the peripapillary region, and the patient regained her vision back to 20/20 OD.
Dr. Kim practices at Nova Southeastern University in Ft. Lauderdale, Fla. where he is also a faculty instructor.
|
1. Wong WT, Agrón E, Coleman HR, et al. Clinical characterization of retinal capillary hemangioblastomas in a large population of patients with von Hippel-Lindau disease. Ophthalmology. 2008 Jan;115(1):181-8. 2. Salazar R, González-Castaño C, Rozas P, Castro J. Retinal capillary hemangioma and von Hippel-Lindau disease: diagnostic and therapeutic implications. Arch Soc Esp Oftalmol. 2011 Jul;86(7):218-21. 3. Maher ER, Yates JRW, Harries R, et al. Clinical-features and natural-history of von Hippel-Lindau disease. Quart J Med. 1990;77:1151–1163 4. Singh AD, Nouri M, Shields CL, et al. Treatment of retinal capillary hemangioma. Ophthalmology. 2002;109:1799–806. 5. Schmidt-Erfurth UM, Kusserow C, Barbazetto IA, Laqua H. Benefits and complications of photodynamic therapy of papillary capillary hemangiomas. Ophthalmology. 2002;109:1256–66. 7. Schmidt D, Natt E, Neumann HP. Long-term results of laser treatment for retinal angiomatosis in von Hippel-Lindau disease. Eur J Med Res. 2000;5:47–58. 6. Goto S, Oshima Y, Tsujikawa M, Nishida K. Massive exudative retinal detachment after photodynamic therapy for peripheral retinal capillary hemangioma. Retin Cases Brief Rep. 2013 Winter;7(1):86-8. 8. Blodi CF, Russell SR, Pulido JS, Folk JC. Direct and feeder vessel photocoagulation of retinal angiomas with dye yellow laser. Ophthalmology. 1990;97:791–7. 9. Welch RB. The recognition and treatment of early angiomatosis retinae and use of cryosurgery as an adjunct to therapy. Trans Am Ophthalmol Soc. 1970;68:367–424. 10. Mitropoulos PG, Chatziralli IP, Peponis VG, et al. Photodynamic therapy for juxtapapillary retinal capillary hemangioma. Case Rep Ophthalmol Med. 2014;2014:756840. 11. Wong WT, Liang KJ, Hammel K, et al. Intravitreal ranibizumab therapy for retinal capillary hemangioblastoma related to von Hippel-Landau disease. Ophthalmology. 2008;115(11):1957–64. |
Retina Quiz Answers:
1) a; 2) c; 3) d; 4) d.

