 |
One of the greatest challenges of treating younger patients with binocular vision and accommodative issues is finding an appropriate add power. One size does not fit all. Let’s dig a little deeper into two ways we can do this: the monocular estimation method (MEM) and the fused cross-cylinder (FCC) test. Some practitioners have been taught that the two methods are interchangeable and you can do one or the other to measure the lag or lead of accommodation. In reality, the two could not be more different.
The FCC Test
We perform the FCC test in dim illumination. With the phoropter in place, set the cross-cylinder lenses in front of the patient. Have the patient close their eyes, place the horizontal/vertical grid at 40cm and add +0.50D of sphere. When the patient opens their eyes, ask them which lines appear darker and clearer. If they report that the lines are equal or horizontal, add plus lenses until the vertical lines are now the blackest or clearest. This is the desired endpoint. If the patient reports that the lines are vertical, on the other hand, add minus lenses until the lines are equal or horizontal. This is the desired endpoint in this situation.
The expected values of the FCC test are +0.50D +/-0.50, which is why we start with +0.50D of sphere. One caveat to keep in mind is that if minus is found, it is best not to use that same amount of minus during the remainder of the near testing sequence. If a higher amount of plus is found, it is considered a lag of accommodation or under-accommodation. By contrast, if a lower amount of plus, or a minus endpoint, is found, it is considered a lead of accommodation or over-accommodation.
Though we are trained to look for “the number,” we should also be using the patient’s responses to assess how they interpret their visual space in this situation. There are numerous variations to the procedure in regard to the starting lens. While I (Dr. Taub) use the previously discussed sequence, Dr. Harris starts with no added lenses, just the distance refraction, to determine if the patient sees what is expected and then adds plus that equates to the stress-point retinoscopy number he obtained in his chair tests. Others start with +1.50D and take it away in increments until the first vertical is reported.
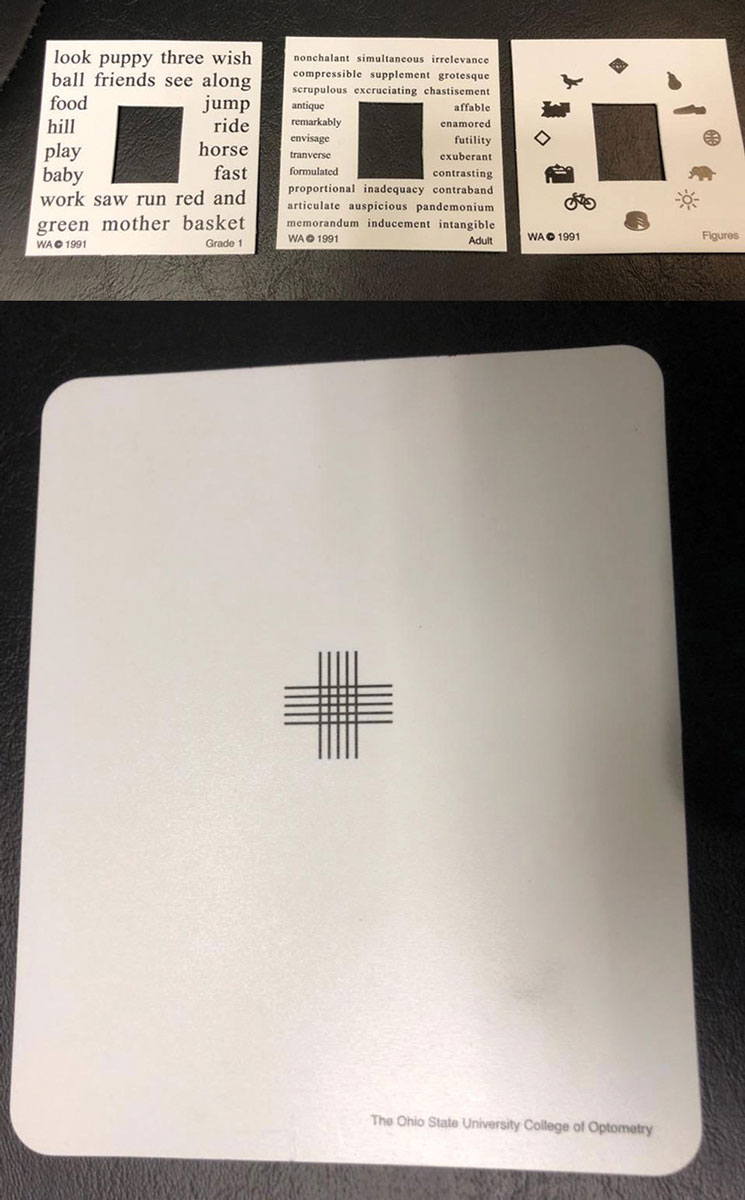 |
| MEM cards (top) and FCC test cards (bottom) are both useful tools to help identify appropriate add powers in patients with binocular vision and accomodative issues. Click to enlarge. |
The MEM
This is one of many options for near-point retinoscopy. The purpose, like the FCC test, is to assess the accommodative response. You can complete the MEM at any point in the examination, either with the habitual glasses or the potential new prescription. Attach an MEM card of the appropriate cognitive level (pictures and basic or complex words) to the retinoscope and hold it at the patient’s Harmon Distance—the distance from the patient’s elbow to their middle knuckle, or the closest distance at which the person should be performing activities. Any closer than this, regardless of the lenses prescribed, the amount of near visual stress increases significantly.
Use loose lenses or skiascopy bars to neutralize the patient’s reflex while they name the pictures and read the words out loud. The trick is to insert the lens quickly and not leave it in place too long to avoid impacting the accommodative response. The lens and light from the retinoscope should not move simultaneously; the lens should be in place before the retinoscope begins sweeping.
The result is based on the assumption that the accommodative stimulus at distance is zero, so the MEM can also determine if the patient is over- or under-minused. The expected result is +0.25D to +0.50D +/-0.50. As with the FCC test, greater amounts of plus indicate a lag of accommodation, while plano to minus indicates a lead of accommodation.
Spot the Differences
In looking at these two tests, there are obvious differences. The FCC test is part of the near-point sequence. While it seems that every doctor has their own near-point sequence, I complete the FCC test after the binocular balance, which is then followed by the negative and positive relative accommodation tests. This provides the clinician with a potential near-point lens, through which we can conduct further binocular and accommodative testing. The MEM, on the other hand, is essentially a stand-alone test that is not part of the near-point sequence. Dr. Harris adds the base-out and base-in duction results in this sequence.
We perform FCC in the phoropter and the MEM in free space. Once you put a patient behind the phoropter, you can never be too sure where their attention is focused. The phoropter is a foreign object that is placed close to the face, and that in and of itself, in our experience, can cause near-point changes.
Target-wise, the FCC test uses vertical and horizontal lines, while the MEM uses pictures and words of varying sizes. The accommodative response is different based on the targets and cognitive components. It is one level of accommodation to identify a picture and read a word out loud and another to look at black lines and determine which are clearer or darker. Both require concentration, but the tasks are quite different.
The MEM is an objective test, while the FCC test is subjective. I prefer the MEM for this reason, as I have learned to trust what I see as the accommodative response as opposed to what the patient says they appreciate. The patient’s interpretation of the black lines can sometimes be problematic, leading to results that do not make sense or seem antithetical to the rest of the examination data. This is one of the reasons some clinicians drop the FCC test from their examination sequence. Eliminating a test that prompts more questions than it answers is the most logical response in this case.
Even though the FCC test is subject to interpretation, its results should not be discounted. Think of the FCC test as a measure of how efficient and effective a patient is at using their visual system. If there isn’t an obvious endpoint and the patient is wavering between several different but equal responses, maybe this is actually telling us how we should prescribe and treat moving forward.
Without a distinct endpoint, near-point lenses are less of a treatment choice. Vision therapy is a more appropriate option to provide the patient meaningful experiences that they can use to build their visual library. When using the results of either test to prescribe a near-point lens, you must leave the patient with their +0.50D buffer (the expected result of each test) in place. For example, if the patient presents with an FCC test or MEM result of +1.00D, you would not want to prescribe a +1.00D add. The most you should consider is +0.50D. Prescribing away the buffer can lead to further near-point issues and have an impact on the distance refraction.
The MEM and the FCC test cannot be used interchangeably. The presence of the phoropter, differing targets and the objective vs. subjective nature of the tests make them completely different. It is up to you which you prefer for your patients, but make sure to choose one.

