 |
A 66-year-old male presented urgently with mildly blurred vision and a “pressure feeling” in his right eye. It began on Saturday and he waited until Monday to come in as, he said, it “wasn’t that bad.” He wore no visual correction, but pinhole acuity was 20/30 in the right eye. He had longstanding vision decrease in his left eye from an old macular scar.
He had a mild injection of his right bulbar conjunctiva. There was, perhaps, a mild bit of corneal edema in his right eye with a few centrally located endothelial keratic precipitates and a rare anterior chamber cell floating freely. His intraocular pressures (IOPs) were 50mm Hg OD and 18mm Hg OS. Years earlier, he had undergone laser iridotomy in each eye for an anatomically narrow angle, which had subsequently opened. Gonioscopy was deferred on this visit.
While the symptomatically elevated IOP might be a diagnostic dilemma, in this case the etiology was apparent, especially in light of the fact that this was his third episode within the past year. Even the patient himself understood the diagnosis before coming in: he was having a recurrence of glaucomatocyclitic crisis (GCC).
Defining GCC
The condition, also known as Posner-Schlossman syndrome, is characterized by these features:
1. Elevated IOP appearing nearly simultaneously with inflammatory cells in the anterior chamber followed by between one and 20 unpigmented keratic precipitates on the corneal endothelium. Posterior synechiae are never formed.
2. An eye that is white or that has minimal dilation of the conjunctival vessels without ciliary flush.
3. The anterior chamber angles are open gonioscopically.
4. The condition is unilateral (although, rarely bilateral cases are possible).
5. The presenting symptoms include slight discomfort, colored halos, visual blurring and an absence of frank pain. The patient may also be completely asymptomatic.
6. The attacks last from hours to a month, but typically occur spontaneously and resolve within two weeks.
7. The episodes may recur with varying frequency and are unpredictable and unprovoked.
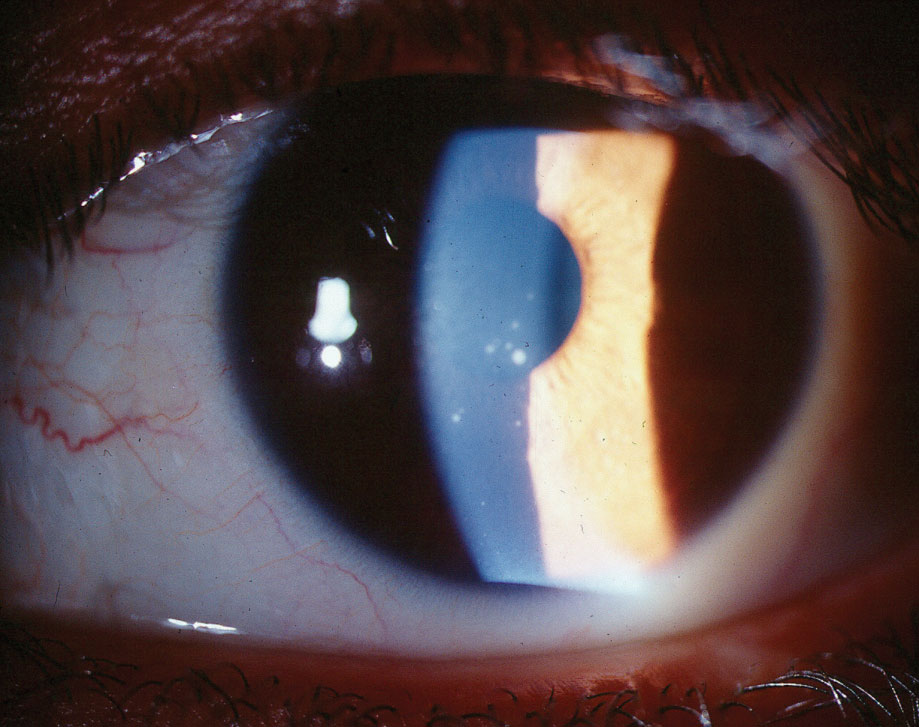 |
| This patient demonstrates centrally located keratic precipitates in glaucomatocyclitic crisis. Click image to enlarge. |
Diagnosis
GCC typically occurs between ages 20 and 50.1-3 It is considered uncommon after age 60 and before age 20, though research shows instances of patients exceeding these ranges.4 GCC is typically recurrent and unilateral.5-7 When it recurs, it afflicts the same eye. Bilateral, simultaneous involvement is uncommon.8,9
Classic uveitic symptoms of pain, photophobia and lacrimation are absent in GCC. Also, a markedly elevated IOP—ranging between 30mm Hg to 40mm Hg—is often seen, although some cases show IOP exceeding 70mm Hg.1,2,6,7,10 The elevated IOP serves to disrupt the sodium-potassium pump on the corneal endothelium with resultant corneal edema and associated symptoms of blurred vision and halos.
The patient may complain of mildly blurred vision, ocular and periorbital discomfort, or may report no symptoms at all.5-7,10 There may be a slightly injected eye with a mild anterior chamber inflammatory reaction with centrally located keratic precipitates.1,2 Flare, common in uveitis, is not common in GCC and synechiae typically do not form.
GCC is an idiopathic inflammatory disease preferentially affecting the trabecular meshwork.11-13 Both herpes zoster and cytomegalovirus (CMV) is associated with GCC.11-13 Additionally, aqueous aspirations of patients in GCC have been positive for genomic fragments of herpes simplex virus (though no live virus has been sampled).14Currently, ample evidence exists for viral involvement in GCC, particularly CMV.15-17 However, CMV is not invariably present in the aqueous humor of all eyes with GCC; thus the understanding of the pathophysiology of this syndrome remains incomplete.
Researchers have postulated that viral-induced inflammation of the trabecular meshwork (acute trabeculitis) impedes the tissue’s aqueous processing ability, though this does remain speculative. The support for inflammation being concentrated in the trabecular meshwork is the fact that GCC is a non-granulomatous uveitic syndrome with no pronounced inflammatory cellular response causing mechanical obstruction of the trabecular meshwork, nor synechiae development leading to angle closure.
Management
As GCC is an inflammatory condition, the most effective treatment of both the inflammation as well as the secondary IOP elevation is a topical corticosteroid.1,5-8 In that the inflammation is mild, doses of a steroid such as prednisolone acetate 1% greater than hourly is not necessary. As synechiae are unlikely to occur and patients are only minimally uncomfortable, cycloplegia is usually unnecessary. However, the use of a mild cycloplegic agent may be employed on a case-by-case basis.
Research documents successful reduction of IOP in GCC with carbonic anhydrase inhibitors, topical beta-blockers and alpha-2 adrenergic agonists.18-20 However, all medications employed to reduce IOP should only be used adjunctively with primary anti-inflammatory therapy. Since GCC is an inflammatory condition, avoid miotics and prostaglandin analogs, as they can potentially exacerbate inflammation. In extremely recalcitrant cases, trabeculectomy remains a viable option in IOP management.21,22 Recent research shows ab interno procedures with trabectome can assist in managing uncontrolled IOP in GCC.23
While permanent glaucomatous damage is not typical, it can occur, especially in patients with frequent recurrences and prolonged attacks.1,2,5,24,25 Since a significant number of eyes with GCC likely have a viral etiology, such as herpes or CMV, antiviral therapy remains a option.26-29
Valcyte (valganciclovir, Genentech), an oral anti-CMV agent, can both manage the acute form of the syndrome and suppress recurrent outbreaks.26,27 The dosage is 900mg BID for two weeks, followed by 450mg BID as long-term suppression therapy.26,27 Cessation of therapy usually results in recurrence.26,27 It is unlikely that all cases of GCC are due to CMV (or any virus), so a blanket recommendation to use oral antiviral medications to manage or suppress GCC has little evidence-based support.26,27
For this patient, we reviewed the clinical situation, prescribed topical prednisolone acetate 1% QID and dorzolamide/timolol BID. He felt back to normal within two days and the steroid was tapered after a week. At two weeks, he had no signs of inflammation and IOP, untreated, was now at 19mm Hg.
|
1. Posner A, Schlossman A. Syndrome of unilateral recurrent attacks of glaucoma with cyclitic symptoms. Arch Ophthalmol. 1948;39:517-35. 2. Jap A, Sivakumar M, Chee SP. Is Posner Schlossman syndrome benign? Ophthalmol. 2001;108(5):913-8. 3. Ritcher R, Shields MB, Krupin T. The Glaucomas. St Louis; Mosby 1989:1205-20. 4. Burnstein Y, Shelton K, Higginbotham EJ. Glaucomatocyclitic crisis in a child. Am J Ophthalmol. 1998;126(1):136-7. 5. Harrington JR. Posner-Schlossman syndrome: A case report. J Am Opt Assoc. 1999:70;11:715-23. 6. Harstad HK, Ringold A. Glaucomatocycltic crises (Posner-Schlossman syndrome): a case report. Acta Ophthalmologica. 1986; 64(2):146-51. 7. Raitta C, Vannas A. Glaucomatocyclitic crisis. Arch Ophthalmol. 1977; 95(4):608-12. 8. Levatin P. Glaucomatocyclitic crises occurring in both eyes. Am J Ophthalmol. 1956;41:1056-9. 9. Puri P, Verma D. Bilateral glaucomatocyclitic crisis in a patient with Holmes Adie syndrome. J Postgrad Med. 1998;44(3): 76-7. 10. Hahn IH, Stillman MC. A case of glaucomatocyclitic crisis in the emergency department. Ann Emerg Med. 2006;47(2):167-9. 11. Bloch-Michel E, Dussaix E, Cerqueti P, et al. Possible role of cytomegalovirus infection in the etiology of the Posner-Schlossman syndrome. Int Ophthalmol. 1987;11(2):95-6. 12. Tanaka Y, Harino S, Hara J. Cellular immunity as judged by varicella skin test in Posner Schlossman patients. Folia Jpn. 1985;36:972-6. 13. Teoh SB, Thean L, Koay E. Cytomegalovirus in aetiology of Posner-Schlossman syndrome: evidence from quantitative polymerase chain reaction. Eye. 2005;19(12):1338-40. 14. Yamamoto S, Pavan-Langston D, Tada R, et al. Possible role of herpes simplex virus in the origin of Posner-Schlossman syndrome. Am J Ophthalmol. 1995;119(6):796-98. 15. Li J, Ang M, Cheung CM, et al. Aqueous cytokine changes associated with Posner-Schlossman syndrome with and without human cytomegalovirus. PLoS One. 2012;7(9):e44453. 16. Yang SY, Chen MJ, Chen KH, et al. Cytomegalovirus and herpes simplex virus as causes of bilateral anterior uveitis in an immunocompetent patient. J Chin Med Assoc. 2011;74(1):48-50. 17. Rodier-Bonifas C, Cornut PL, Billaud G, et al. Cytomegalovirus research using polymerase chain reaction in Posner-Schlossman syndrome. J Fr Ophtalmol. 2011;34(1):24-9. 18. Hung PT, Chang JM. Treatment of glaucomatocyclitic crises. Am J Ophthalmol. 1974;77(2):169-72. 19. Ohno S, Ichiisi A, Matsuda H. Hypertensive effects of Carteolol on intraocular pressure elevation and secondary glaucoma associated with endogenous uveitis. Ophthalmologica. 1989;199:41-5. 20. Muthusamy P. Apraclonidine in the management of glaucomatocyclitic crisis. Eye. 1994;8(3):367-8. 21. Dinakaran S, Kayarkar V. Trabeculectomy in the management of Posner-Schlossman syndrome. Ophthalmic Surg Lasers. 2002;33(4):321-2. 22. Zhong Y, Cheng Y, Liu X, Feng P. Trabeculectomy in the management of glaucomatocyclitic crisis with visual field defect. Ocul Immunol Inflamm. 2010;18(3):233-6. 23. Pahlitzsch M, Torun N, Gonnermann J, et al. Trabeculectomy ab interno (trabectome): yet another possibility in the treatment of uncontrolled glaucomatocyclitic crisis under systemic valganciclovir therapy? Eye (Lond). 2015;29(10):1335-9. 24. Theodore F. Observations on glaucomatocyclitic crisis (Posner-Schlossman syndrome). Br J Ophthalmol. 1952;36:207-10. 25. Kass MA, Becker, B, Kolker AE. Glaucomatocycltic crisis and primary open angle glaucoma. Am J Ophthalmol. 1973;75:668-73. 26. Sobolewska B, Deuter C, Doycheva D, Zierhut M. Long-term oral therapy with valganciclovir in patients with Posner-Schlossman syndrome. Graefes Arch Clin Exp Ophthalmol. 2014;252(1):117-24. 27. Wong VW, Chan CK, Leung DY, Lai TY. Long-term results of oral valganciclovir for treatment of anterior segment inflammation secondary to cytomegalovirus infection. Clin Ophthalmol. 2012;6:595-600. 28. Megaw R, Agarwal PK. Posner-Schlossman syndrome. Surv Ophthalmol. 2017;62(3):277-85. 29. Chan NS, Chee SP, Caspers L, Bodaghi B. Clinical features of CMV-associated anterior uveitis. Ocul Immunol Inflamm. 2018;26(1):107-15. |

