 |
A 61-year-old man was referred for elevated intraocular pressure (IOP). He had no visual or ocular complaints and reported no ocular trauma.
His best-corrected visual acuity was 20/20 in each eye with a moderately hyperopic correction. His anterior chambers were deep, more so in the left eye than the right. A Krukenberg spindle of pigment was noted on his left corneal endothelium. His IOPs were 15mm Hg OD and 38mm Hg OS. Central corneal thickness was slightly less than 500µm in each eye. Optical coherence tomography (OCT) showed early abnormalities in the left eye. Threshold perimetry revealed mild visual field defects nasally in his left eye. Gonioscopically, trabecular pigmentation was mild throughout the right angle and very dense throughout the left. His right iris assumed a planar configuration to the angle recess while his left iris was markedly concave.
Making the Call
I diagnosed this patient with unilateral pigmentary glaucoma in the left eye with pigment dispersion coming from an anomalous iris configuration that was not present in the right eye. Patients with pigment dispersion syndrome and pigmentary glaucoma demonstrate liberation of iris pigment within the anterior chamber. Often, this appears as a vertical, granular brown band along the central corneal endothelium known as a Krukenberg spindle.1-3 Pigment accumulation may also be evident on the lens and iris.
Dense pigmentation is seen gonioscopically, often covering the trabecular meshwork (TM) for 360˚ with increased prominence in the inferior quadrant. When pigment accumulates on Schwalbe’s line, it is referred to as Sampaolesi’s line. The angle recess remains unchanged and open. Radial, spoke-like transillumination defects of the mid-peripheral iris are common, though not present in every patient.4
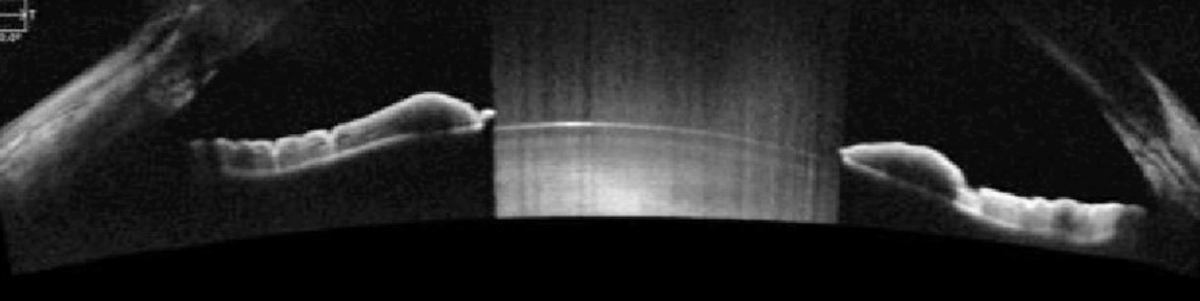 |
| This patient’s anterior OCT shows a markedly concave iris. Click image to enlarge. |
Pathophysiology
Pigment release occurs as a result of the proximity between the posterior iris pigment epithelium and the zonular fibers of the lens. The abrasive nature of this physical contact leads to mechanical disruption of the posterior iris surface and release of pigment granules into the posterior chamber, which follows the flow of the aqueous convection current into the anterior chamber angle.5-7
Many patients with pigment dispersion syndrome and pigmentary glaucoma demonstrate a concave approach of the iris as it inserts into the anterior chamber angle, giving the iris a “backward-bowed” appearance on gonioscopy.7 This posterior bowing of the iris places the posterior iris into apposition with the lens zonules. As the iris responds to light, iridozonular friction results in pigment liberation from the posterior iris. Sometimes the degree of pigment loss in the mid-peripheral areas produces visible transillumination defects corresponding to packets of iris zonular fibers.5 While the majority of these patients have a concave iris approach, others may have a flat or planar approach, making the mechanism of pigment release less clear.6
Researchers theorize that, in cases with a markedly concave iris insertion, the iris functions as a flap valve lying against the anterior lens surface. When a pressure gradient develops that is greater in the anterior chamber, the iris is forced backwards, closing the valve and trapping the aqueous from moving into the anterior chamber. The increased pressure forces the iris into the concave approach causing a “reverse pupillary block.” This increases the irid-zonular friction and apposition, leading to pigment release from the posterior iris.8,9 This seems to increase upon blink.9-11
Fallout
When excessively released pigment accumulates in the TM, there are two possible consequences. First, pigment may reside benignly in the trabecular meshwork. Here, IOP is unaffected and the condition remains pigment dispersion syndrome. Alternatively, when the pigment causes IOP to rise and damage occurs, the patient develops pigmentary glaucoma.6
Interestingly, pigment granules blocking the TM are not the likely to raise IOP long term.12 Endothelial cells lining the trabecular beams of the TM quickly phagocytize small amounts of accumulated pigment, preserving the normal architecture of the TM.13-15 However, in chronic cases of pigment dispersion, greater amounts of pigment are more difficult for the cells to phagocytize. When this occurs, the endothelial cells that line the TM beams disintegrate, contributing to a rise in IOP.15
As pigment dispersion syndrome’s only impact on ocular health is potential development of pigmentary glaucoma, these patients should be treated as glaucoma suspects. Monitor these patients for IOP elevation and optic nerve changes periodically. Patients with pigment dispersion syndrome who were followed for more than 10 years without developing pigmentary glaucoma have lower risk of later development.16 The risk of developing pigmentary glaucoma from pigment dispersion syndrome is 10% at five years and 15% at 15 years.17 Myopic males in this age range were more likely to convert to pigmentary glaucoma, and an IOP greater than 21mm Hg at initial examination was associated with an increased risk of conversion.17
 |
| This patient demonstrates heavy trabecular meshwork pigmentation. Click image to enlarge. |
Therapies
Medical treatment of pigmentary glaucoma involves reduction of IOP with aqueous suppressants.1 Beta blockers, carbonic anhydrase inhibitors and alpha-adrenergic agonists are all acceptable options.
Prostaglandin medications can lower IOP in eyes with pigment dispersion.18 Researchers have not specifically reported rho-kinase inhibitors, either in isolation or in combination with latanoprost as a therapy for pigmentary glaucoma. This class of medication is approved for open-angle glaucoma (which theoretically encompasses pigmentary glaucoma) and ocular hypertension. Rho-kinase inhibitors act through trabecular relaxation and increased outflow.19 However, it is unknown if the heavy degree of trabecular pigmentation would be a hinderance to this effect.
Procedures
Patients with pigmentary glaucoma respond well to argon laser trabeculoplasty and selective laser trabeculoplasty (SLT).20-23 One series shows post-SLT IOP elevation was a serious adverse event.22 Lower power settings may be necessary in patients with heavily pigmented angles.
Laser peripheral iridotomy (LPI) can convert the iris from a concave to a planar approach.6-8 It also decreases the biomechanical factor, causing contact between the iris and zonular fibers, and may lower IOP. Nevertheless, the effects of LPI on visual field changes and progression have not been established in pigmentary glaucoma.23,24
My patient was treated with topical latanoprost in his left eye after detailed discussion of risks and benefits as well as possible cosmetic asymmetry from prostaglandin use. His IOP reduced to 18mm Hg in his treated eye and he’s currently being followed without adverse events or progression.
| 1. Farrar S, Shields M. Current concepts in pigmentary glaucoma. Surv Ophthalmol. 1993;37(4):233-52. 2. Roberts D, Miller E, Kim L. Pigmentation of the posterior lens capsule central to Wieger’s ligament and the Scheie line: a possible indication of the pigment dispersion syndrome. Optom Vis Sci. 1995;72(10):756-62. 3. Lehto I, Ruusuvaara P, Setala K. Corneal endothelium in pigmentary glaucoma and pigment dispersion syndrome. Acta Ophthalmol. 1990;68(6):703-9. 4. Ritch R. Pigment dispersion syndrome. Am J Ophthalmol. 1998;126(3):442-5. 5. Campbell D. Pigmentary dispersion and glaucoma: a new theory. Arch Ophthalmol. 1979;97;1667-72. 6. Campbell D, Schertzer RM. Pathophysiology of pigment dispersion syndrome and pigmentary glaucoma. Curr Opin Ophthalmol. 1995;6(2):96-101. 7. Potash S, Tello C, Liebmann J, Ritch R. Ultrasound biomicroscopy in pigment dispersion syndrome. Ophthalmol. 1994;101(2q):332-9. 8.Karickhoff J. Pigmentary dispersion syndrome and pigmentary glaucoma: a new treatment, and a new technique. Ophthalmic Surg. 1992;23(4):269-77. 9.Karickhoff J. Reverse pupillary block in pigmentary glaucoma: follow-up and new developments. Ophthalmic Surg. 1993;24(8):562-3. 10. Campbell D. Iridotomy, blinking, and pigmentary glaucoma. Invest Ophthalmol Vis Sci. 1993;34(4 suppl):993. 11. Liebmann J, Tello C, Ritch R. Pigment dispersion syndrome, iris configuration, and blinking. Invest Ophthalmol Vis Sci. 1994;35(5 suppl):1558. 12. Murphy C, Johnson M, Alvarado J. Juxtacanalicular tissue in pigmentary and primary open angle glaucoma. The hydrodynamic role of pigment and other constituents. Arch Ophthalmol. 1992;110(12):1779-85. 13. Rohen J, van der Zypen EP. The phagocytic activity of the trabecular meshwork endothelium: an electron microscopic study of the vervet (ceropithicus aethiops). Graefes Arch Clin Exp Ophthalmol. 1968;175:143-60. 14. Sherwood M, Richardson TM. Evidence for in vivo phagocytosis by trabecular endothelial cells. Invest Ophthalmol Vis Sci. 1980;19(4 suppl):66, 15. Richardson TM, Hutchinson BT, Grant WM. The outflow tract in pigmentary glaucoma: a light and electron microcroscopy study. Arch Ophthalmol. 1977;95:1015-25. 16. Mastropasqua L, Ciancaglini M, Carpineto P, et al. Early stadiation of pigmentary dispersion syndrome and long-term analysis of progression to pigmentary glaucoma. Ann Ophthalmol Glaucoma. 1996;28(5):301-7. 17. Siddiqui Y, Ten Hulzen RD, Cameron JD, et al. What is the risk of developing pigmentary glaucoma from pigment dispersion syndrome? Am J Ophthalmol. 2003;135(6):794-9. 18. Grierson I, Pfeiffer N, Cracknell K, et al. Histology and fine structures of the iris and outflow system following Latanoprost therapy. Surv Ophthalmol. 2002;47 Suppl 1:S176-84. 19. Aref AA, Geyman LS, Zakieh AR, Alotaibi HM. Netarsudil and latanoprost ophthalmic solution for the reduction of intraocular pressure in open-angle glaucoma or ocular hypertension. Expert Rev Clin Pharmacol. 2019;12(12):1073-79. 20. Liebmann J, Ritch R, Robin A, et al. Argon laser trabeculoplasty in pigmentary glaucoma: long-term follow-up. Ophthalmol. 1993;100(6):909-13. 21. Koucheki B, Hashemi H. Selective laser trabeculoplasty in the treatment of open-angle glaucoma. J Glaucoma. 2012;21:65-70. 22. Harasymowycz PJ, Papamatheakis DG, Latina M, et al. Selective laser trabeculoplasty (SLT) complicated by intraocular pressure elevation in eyes with heavily pigmented trabecular meshworks. Am J Ophthalmol. 2005;139(6):1110-3 23. Buffault J, Leray B, Bouillot A, et al. Role of laser peripheral iridotomy in pigmentary glaucoma and pigment dispersion syndrome: a review of the literature. J Fr Ophthalmol. 2017;40(10):889-97. 24. Michelessi M, Lindsley K. Peripheral iridotomy for pigmentary glaucoma. Cochrane Database Syst Rev. 2016;2:CD005655. |

