 Whose responsibility is it to educate our patients about the importance of nutrition, lifestyle and excess weight gain with respect to diabetes management? Historically, we left this task to the patient’s primary care physician. However, with escalating rates of obesity and metabolic syndrome in North America––in addition to a rapidly expanding incidence of vision loss secondary to diabetic eye disease––optometrists simply can’t sit on the sidelines anymore.
Whose responsibility is it to educate our patients about the importance of nutrition, lifestyle and excess weight gain with respect to diabetes management? Historically, we left this task to the patient’s primary care physician. However, with escalating rates of obesity and metabolic syndrome in North America––in addition to a rapidly expanding incidence of vision loss secondary to diabetic eye disease––optometrists simply can’t sit on the sidelines anymore.
As primary eye care providers, it is our responsibility to educate and motivate our patients to maintain a healthy weight through proper nutrition and lifestyle modification. Ultimately, their vision and systemic well-being depend on our guidance.
Metabolic Syndrome and the Diabetes Epidemic
According to the International Diabetes Federation (IDF), metabolic syndrome is a collective term that encompasses several of the most dangerous risk factors for heart attack, including pre-diabetes, abdominal obesity, high cholesterol and high blood pressure.1 Affected individuals have a five-fold risk of developing type II diabetes, and are three times more likely to have a heart attack or stroke than healthy individuals. Currently, the IDF estimates that up to 25% of adults worldwide have metabolic syndrome.1
Data from the 2011 National Diabetes Fact Sheet show that nearly 26 million Americans have been diagnosed with diabetes, and another 79 million are considered pre-diabetic.2 Additionally, seven million Americans suffer from the disease but remain undiagnosed.2
Diabetes is the leading cause of new cases of blindness among adults aged 20 to 74. The National Eye Institute reports that nearly half of Americans with diabetes have diabetic retinopathy.2 Of those, nearly 5% have sight-
threatening retinopathy, with significantly higher rates among African, Latino and Native American populations.2
However, one of the most alarming aspects of this epidemic is the increasing frequency of both type 1 and type 2 diabetes in American youth. Between 2009 and 2011, the incidence of both conditions increased by more than 20%.3,4
This is a real crisis. However, the good news is that we can do something about it. Type 2 diabetes is preventable, and it accounts for 95% of all cases.2 If we educate our patients about the relationship between weight, exercise, dietary intake and diabetic eye disease, we can reduce the incidence of type 2 diabetes and help prevent associated vision loss.
What’s the Solution?
The typical North American diet contains high amounts of processed, calorie-dense foods that offer little nutritional value, and consequently promote weight gain. Serving sizes, both in restaurants and at home, are expanding in direct proportion with the waistlines of millions of Americans.
Further, many people––particularly children––are consuming too many soft drinks and sugary beverages that can promote type 2 diabetes. If these general trends continue into the foreseeable future, more people will experience signs and symptoms of diabetic eye disease at increasingly younger ages.
According to the Diabetes Prevention Program (DPP), lifestyle changes for pre-diabetics have a significant impact on diabetes prevention.5 The DPP was a two-year, multicenter, randomized clinical trial that was designed to determine if modest weight loss via dietary alteration and increased physical activity could prevent or delay the onset of type 2 diabetes more effectively than treatment with metformin.
Participants began the study being overweight and exhibiting blood glucose levels that were higher than normal, but clinically insufficient for a diagnosis of diabetes. The study results showed that diabetes incidence was reduced by 58% in participants who received intensive training in proper dietary intake, physical activity and behavioral modifications, compared to just 31% who received metformin to lower blood glucose levels.5
At 10-year follow-up, the DPP researchers determined that the onset of diabetes could be delayed for at least a decade in patients who continued to eat properly and exercise regularly following the study’s conclusion.6 Considering these results, it is critical to educate our patients about the protective benefits of lifestyle modification.
 Weight Control
Weight Control
Excess weight gain is one of the fundamental causes of type 2 diabetes. Indeed, the risk of developing diabetes increases seven-fold in overweight people, and 20- to 40-fold in obese people.7 The most widely accepted way to determine a patient’s weight status is to calculate his or her Body Mass Index (BMI), which is a ratio based upon an individual’s weight and height.
Waist circumference is another predictor of diabetes. According to a cohort of the Nurses’ Health Study, the risk of type 2 diabetes increased progressively in quintiles of patients with the largest waist circumferences (35 inches or greater in women, and 40 inches or greater in men).8,9
Additionally, according to the Harvard School of Public Health, losing 7% to 10% of your current weight can reduce your chances of developing type 2 diabetes by as much as 50%.10 For patients who don’t exercise and/or have poor diets at baseline, this sort of weight reduction goal is relatively easy to achieve. For example, those who weigh 150lbs would have to lose just 10lbs to 15lbs.
Increased Physical Activity
In the DPP, 2.5 hours of exercise per week (i.e., brisk walking) was independently helpful at reducing subjects’ risk of diabetes.5 However, according to another cohort from the Nurses’ Health Study, physical activity alone does not eliminate an individual’s risk for type 2 diabetes.8
It is worth noting that other studies challenge this finding, and indicate that physical activity is indeed an independent factor in diabetes prevention.11 Specifically, weight control is the most important factor to consider—and certainly, physical activity helps facilitate weight loss.
To achieve optimal health benefits, adults should physically exert themselves for at least 30 minutes per day. Even more importantly, however, children should engage in at least 60 continuous minutes of physical activity each day.11
Dietary Control
In order to lose weight, patients need to expend more calories than they consume. A diet that closely adheres to the recommendations made by the Omni-Heart study is a great way to help reduce weight, while ensuring that food intake is of high quality.12
Diets constructed in accordance with these suggestions are rich in vegetables and fruits, and low in saturated/trans fats, sodium and added sugar.
A standard 2,100-calorie diet should include 11 servings of vegetables and fruit, as well as one to two servings each of whole grains, low-fat dairy, lean proteins, legumes and nuts. (Every patient’s ideal caloric intake level should be calculated by his or her dietitian.)12
Closely adhering to such recommendations, however, leaves little room for foods that are rich in sugar, such as processed sweets and soft drinks.
Go for Whole Grain
Processed foods and refined grains comprise a large portion of the average North American’s diet. These foods yield high glycemic indices and loads, meaning that they increase blood sugar levels significantly more than healthier, non-processed alternatives.
Whole grains contain more fiber and generally have a lower glycemic index than refined grains.13 A diet rich in whole grains is associated with a reduced risk of type 2 diabetes, whereas high intake levels of processed foods are directly linked to an increased risk of diabetic disease.14,15
Thus, all patients should make an effort to replace refined grains with whole-grain foods. Despite the health benefits of whole grains, their caloric content often can be similar to that of refined grains––so it is important to be mindful of proper serving sizes.
Avoid Sugary Drinks
There is no real cordial way to address this point, but––Americans must stop drinking calorie-laden soft drinks! Soda, sweet tea, blended juice drinks and specialty coffees all contain large quantities of empty calories in the form of simple sugars. They have a high glycemic load and do not provide satiety, so people do not actually consume less food at their next meal.
Multiple studies have shown that women who drank at least one sugar-sweetened soft drink or fruit punch beverage per day were at an increased risk for developing type 2 diabetes.16,17
How Can We Help Motivate Our Patients?
Some of our patients know that excess weight gain is directly linked to poor systemic health. However, many of them do not know that high body weight can increase their risk for several serious ocular conditions.
The discussion of weight management often is difficult for optometrists to initiate during an eye exam. In most situations, an individual’s body weight can be quite personal, and the practitioner may be fearful of being perceived as judgmental. In addition to this potential stigma, patients generally do not expect this conversation to occur in an eye care setting.
To be effective, you need to approach the patient in a culturally sensitive and age-appropriate manner. Counseling alone will not result in weight loss and lifestyle alteration.
Thus, the ultimate goal is to increase the individual’s motivation and confidence. So, how can you achieve this?
Initiate the Conversation
Research shows that patients respond best to objective terms, such as “weight” and “BMI,” rather than more pointed terms, such as “overweight” or “obese.”
People often view such neutral phrasing as being the most motivating and least disparaging.18,19
Here is an example of how to initiate the conversation with your patient, including recommended questions from the American Medical Association:
• “We define a healthy weight according to body mass index, or BMI, which is based on your height and weight. A healthy BMI is less than 25, overweight is between 25 and 30, and severely overweight is defined as a BMI greater than 30. Based on your height and weight your BMI is ‘X.’ This can affect the health of your eyes by increasing your risk for diabetic retinopathy and age-related macular degeneration.”
Once the patient is aware of the risks associated with an increased BMI, he or she will be more open to further discussing weight control. Asking permission shows respect and will help the patient feel more comfortable during the conversation.
Here’s an example:
• “I am concerned about your weight and the impact that it may have on your ocular health. I would like to discuss this relationship with you today––is that ok?”
Motivational Interviewing
It is important to keep the conversation going to achieve patient motivation. The Yale Rudd Center for Food Policy and Obesity encourages the use of motivational interviewing for improving diet, exercise levels and weight control. Its primary aim is to help empower patients to make their own decisions about behavioral modification. Here are some examples of questions that will help to motivate your patients to make positive lifestyle changes:20
• “How ready do you feel to change your eating patterns and/or lifestyle behaviors?”
• “What kinds of things have you done in the past to change your eating habits?”
• “What types of physical activity do you enjoy?”
It’s a Team Effort
Once they are ready to make a change, patients will require additional support. Proper guidance is critical to ensure that they achieve healthy, long-term weight loss goals. With the abundance of fad diets and conflicting information on the Internet and television, how can we expect them to sort through it all and make realistic decisions?
The American Diabetes Association educates patients about the importance of their health care team. Consider referring your patients to a registered dietitian, certified diabetes educator and exercise physiologist.
The management of diabetes requires a collective effort, and active communication with the patient’s primary care provider is essential for effective long-term care. And don’t forget to remind your patients that they are the most important part of their own health care team!
It All Starts With Pediatrics
We need to empower, support and motivate the entire family to inspire children and teens toward a healthier future. But, how can we influence families to change behaviors when increased intake of high-calorie foods and reduced levels of physical activity is becoming the norm in contemporary America? Rather than handing them a prescription on how to achieve and maintain a healthy weight, we need to be more interactive and assume a role of motivator and counselor.21-24
Non-judgmental questions combined with attentive listening will help you uncover the beliefs and values of the patients and their parents. The following questions are examples that likely will not cause the individual to become defensive:
• To the child: “Do you know your approximate weight and height? I am going to use this information to calculate your BMI.”
• To the parent: “Your child’s BMI is very high. It is important that she gains control of her weight before it becomes a bigger problem that also can affect her vision.”
Making a Change
Once the parents are aware of the medical and visual implications of excess weight gain and poor dietary/lifestyle habits, they will be motivated to help their children. The fundamental goal is to achieve permanent, long-term changes, which typically should involve lifestyle modifications for the entire family.
Be sure to reiterate that initial goals should be realistically achievable, and that changes should be made incrementally. Also, stress that even minimal weight loss can decrease diabetes rates in those who are at risk.21-24
Asking the parents open-ended questions will help initiate the conversation:
• “Mrs. Smith, what changes have you made in your family’s diet so far?”
Motivating Children
Your office environment can play an important role in motivating your patients toward a healthier lifestyle. Run in-office and online contests. Start simple, for example, and challenge kids to eat five to 10 fruits and vegetables per day.
Then, instruct them to maintain a log for one month and submit it to your office to enter a prize drawing. Similar contests for at least one hour of physical activity per day also are effective.
Another great initiative is Let’s Move, Michelle Obama’s campaign designed to help curtail childhood obesity. The initiative’s website (www.letsmove.gov) advises that all health care providers include a BMI screening as an aspect of patient care, actively prescribe increased levels of physical activity and healthy eating habits, and to become more involved as a leader in their local communities.
With appropriate education about the value of proper nutrition and lifestyle modification, you can help your patients achieve and maintain a healthy body weight. This, in turn, will help protect them against the onset of debilitating systemic and ocular disease.
Keep in mind that healthy dietary practices often transform into life-long habits. Therefore, the earlier you inspire younger patients to eat nutritiously and engage in regular physical activity, the less likely they will be to develop diabetic eye disease in the future.
Dr. Capogna is an active partner at Peninsula Vision Associates in Niagara Falls, Canada, and frequently lectures on nutrition and patient care. Dr. Pelletier is a partner at IRIS in Welland, Ontario, where she practices primary care optometry and lectures about nutrition and eye health. Together, they coauthored the top-selling books “Eyefoods: A Food Plan for Healthy Eyes” and “Eyefoods for Kids: A Tasty Guide to Nutrition and Eye Health,” as well as developed the website www.eyefoods.com.
1. International Diabetes Federation. Worldwide definition of metabolic syndrome. Available at: www.idf.org/metabolic-syndrome. Accessed February 11, 2014.
2. Centers for Disease Control and Prevention. National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States, 2011. Available at: www.cdc.gov/diabetes/pubs/pdf/ndfs_2011.pdf. Accessed February 11, 2014.
3. American Diabetes Association. Statistics about diabetes: Data from the 2011 national diabetes fact sheet. Available at: www.diabetes.org/diabetes-basics/statistics/?loc=db-slabnav. Accessed February 11, 2014.
4. Liese AD, D’Agostino RB Jr, Hamman RF, et al. The burden of diabetes mellitus among US youth: prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics. 2006 Oct;118(4):1510-8.
5. Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Eng J Med. 2002 Feb 7;346(6):393-403.
6. Knowler WC. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009 Nov 14;374(9702):1677-86
7. Hu FB, Manson JE, Stampfer MJ, et al. Diet, lifestyle, and the risk of type 2 diabetes mellitus in women. N Engl J Med. 2001 Sep 13;345(11):790-7.
8. Rana JS, Li TY, Manson JE, Hu FB. Adiposity compared with physical inactivity and risk of type 2 diabetes in women. Diabetes Care. 2007 Jan;30(1):53-8.
9. Klein S, Allison DB, Heymsfield SB, et al. Waist circumference and cardiometabolic risk: a consensus statement from Shaping America’s Health: Association for Weight Management and Obesity Prevention; NAASO, The Obesity Society; the American Society for Nutrition; and the American Diabetes Association. Am J Clin Nut. 2007 May;85(5):119701202.
10. Harvard School of Public Health. Simple Steps to Preventing Diabetes. Available at: www.hsph.harvard.edu/nutritionsource/preventing-diabetes-full-story/. Accessed February 11, 2014.
11. Mayer-Davis EJ, D’Agostino R Jr, Karter AJ, et al. Intensity and amount of physical activity in relation to insulin sensitivity: the Insulin Resistance Atherosclerosis Study. JAMA. 1998 Mar 4;279(9):669-74.
12. Appel LJ, Sacks FM, Carey VJ, et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA. 2005 Nov 16;294(19):2455-64.
13. Chiu CJ, Milton RC, Klein R, et al. Dietary carbohydrate and the progression of age-related macular degeneration: a prospective study from the Age-Related Eye Disease Study. Am J Clin Nutr. 2007 Oct;86(4):1210-8.
14. Fung TT, Hu FB, Pereira MA, et al.Whole-grain intake and the risk of type 2 diabetes: a prospective study in men. Am J Clin Nutr. 2002 Sep;76(3):535-40.
15. Liu S, Manson JE, Stampfer MJ, Hu FB, et al A prospective study of whole-grain intake and risk of type 2 diabetes mellitus in US women. Am J Public Health. 2000 Sep;90(9):1409-15.
16. Schulze MB, Manson JE. Sugar-sweetened beverages, weight gain and incidence of type 2 diabetes in young and middle-aged women. JAMA. 2004 Aug 25;292:927-34.
17. Bazzano L, Li TY, Kamudi J, Hu F. Intake of fruit, vegetables and fruit juices and risk of diabetes in women. Diabetes care. 2008 Jul;31(7):1311-7.
18. Yale University: The Rudd Center for Food Policy and Obesity. How to talk about ‘weight’ with your overweight and obese patients. Available at: www.yaleruddcenter.org/resources/bias_toolkit/toolkit/Module-2/2-01-HowToTalk.pdf. Accessed February 11, 2014.
19. Wadden TA, Didie E. What’s in a name? Patients’ preferred terms for describing obesity. Obes Res. 2003 Sep;11(9):1140-6.
20. DiLillo V, Siegfried NJ, Smith-West D. Incorporating motivational interviewing into behavioral obesity treatment. Cognitive Behavioral Prac. 2003;10:120-30.
21. Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007 Dec;120 Suppl 4:S164-92.
22. Rosenbloom AL, Silverstein JH, Ameniya S, et al. Type 2 diabetes in children and adolescents. Pediatr Diabetes. 2009 Sep;10 Suppl 12:17-32.
23. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2012 Feb 1;307(5):483-90.
24. Puhl RM, Peterson JL, Luedicke J. Parental perceptions of weight terminology that providers use with youth. Pediatrics. 2011 Oct;128(4):e786-93.
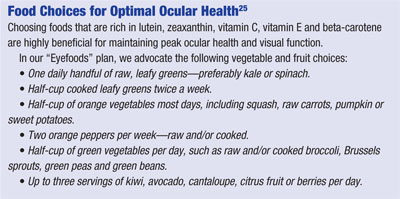
25. Capogna L, Pelletier B. Eyefoods: A Food Plan for Healthy Eyes. St. David’s, Ontario: LB Media Concepts Inc.; 2011.

