 |
History
A 77-year-old Caucasian male presented to the office with a chief complaint of poor vision in his left eye for five days. He explained that, upon waking, he noticed his vision was bad.
He recounted having been treated by a retinal specialist the last time this happened, that time to his right eye. He reported no pain. His history included medically controlled diabetes and hypertension. He denied allergies of any kind.
 |
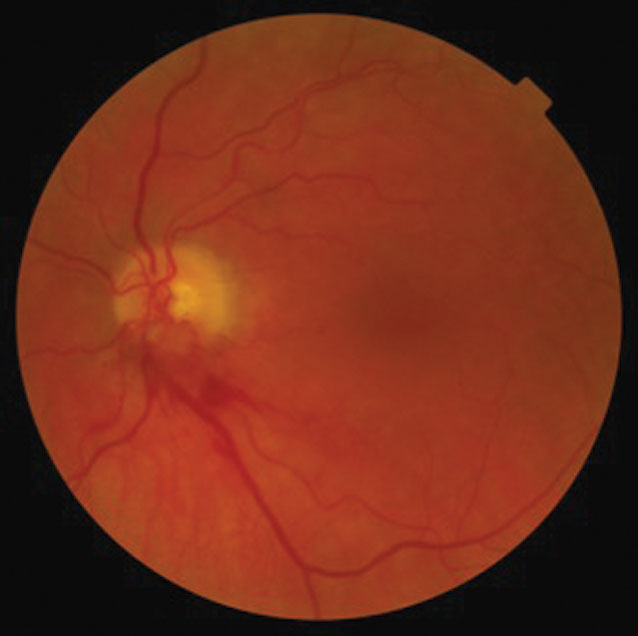 |
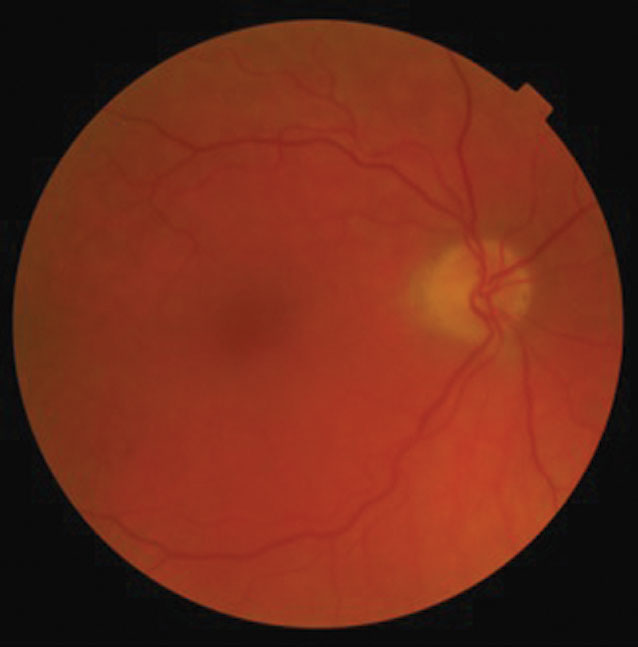
| This 77-year-old patient has had poor vision in his left eye for nearly a week. Can the details of his exam and these fundus images explain the cause of his disturbance? |
Diagnostic Data
His best-corrected entering visual acuities were 20/20 OD and 20/200 OS at distance and near. His external examination uncovered a central scotoma in the left eye upon facial Amsler testing.
All other external findings were normal, and there was no evidence of afferent pupillary defect. Biomicroscopic examination of the anterior segment was normal in the right eye, but found suspended red cells in the anterior chamber of the left. Goldmann applanation tonometry measured 15mm Hg OU.
Your Diagnosis
Does the case presented require any additional tests, history or information? What steps would you take to manage this patient? Based on the information provided, what would be your diagnosis? What is the patient’s most likely prognosis?
Discussion
Additional studies included laser interferometry to assess best visual acuity and B-scan ultrasonography to assess the posterior segment.
The diagnosis in this issue is vitreous hemorrhage in the left eye, presumably secondary to proliferative diabetic retinopathy (PDR). Alternate sources of sudden, painless vision loss include retinal venous occlusion, retinal artery occlusion, retinal detachment, vitreous hemorrhage from retinopathy of the hypercoagulable state and subretinal hemorrhage secondary to choroidal neovascular membrane formation. The PDR vector is likely secondary to the patient’s previous PDR history and poor diabetic control.
Proliferative diabetic vitreoretinopathy is dangerous because it has the potential to produce two forms of catastrophic visual loss: non-clearing vitreous hemorrhage and tractional retinal detachment. In the late 1970s through the 2000s, the predominant method of regressing PDR was via the guidelines of the Diabetic Retinopathy Study (DRS), which was sponsored by the National Eye Institute (NEI) of the National Institutes of Health (NIH).1 The study endorsed panretinal photocoagulation (PRP), or scatter photocoagulation, beginning the trend of what is now known as “evidence-based medicine.” The method was successful by creating numerous peripheral laser burns using large spots and large power. The resulting chorioretinal damage permitted choroidal oxygen to perfuse into the ischemic retinal tissue for use.2 The resulting reduction in retinal tissue, secondary to iatrogenic laser injury, reduced overall oxygen demand. The advantage to this therapy was reduced severe vision loss as defined by the DRS; however, the disadvantage was caustic and widespread collateral retinal damage.2,3
When the anti-vascular endothelial growth factor (anti-VEGF) injection revolution was demonstrated to be effective in cases of PDR, it offered a method of regressing neovascularization without producing collateral retinal tissue loss.4 The disadvantages of anti-VEGF include risk of infection, retinal detachment, vitreous hemorrhage and retinal pigment epithelial detachment.5
The diabetic retinopathy vitrectomy study (DRVS) by the NEI of the NIH demonstrated that early three-port pars plana vitrectomy was preferable to simply monitoring the vitreous hemorrhage as it settled into the inferior posterior chamber, creating the opportunity to apply PRP.6,7
Today, patients should be advised to sleep “sitting up” so that the vitreous blood can settle on the bottom of the posterior chamber. If there is significant inflammation, you can employ atropine 1% BID and topical steroidal anti-inflammation therapy. If intraocular pressure is elevated, you can control it with topical aqueous suppressive medications, such as beta-blockers and alpha adrenergics. If necessary, you can also initiate oral carbonic anhydrase therapy as long as there are no contraindications. Consider an anti-VEGF injection first to assess the possibility of a non-surgical solution.8 If it is unsuccessful, or if there is a vitreous rebleed, it may be time to discuss vitrectomy.
The retinologist who placed an anti-VEGF injection in the patient’s left eye within five days of the referral confirmed all of these points as accurate and considered a vitrectomy as well.
Dr. Gurwood thanks Shruti Desai, OD, Nick Karbach, OD, and Denise Gurwood, OD, for contributing this case.
1. Diabetic Retinopathy Study Research Group. Photocoagulation treatment of proliferative diabetic retinopathy: the second report of diabetic retinopathy study findings. Ophthalmology. 1978;85(1):82-106. 2. Photocoagulation treatment of proliferative diabetic retinopathy: relationship of adverse treatment effects to retinopathy severity. Diabetic Retinopathy Study report no. 5. Dev Ophthalmol. 1981;2:248-61. 3. The Diabetic Retinopathy Study Research Group. Indications for photocoagulation treatment of diabetic retinopathy: Diabetic Retinopathy Study report no. 14. Int Ophthalmol Clin. 1987;27(4):239-53. 4. Mitchell P, Bandello F, Schmidt-Erfurth U, et al. The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology. 2011;118(4):615-25. 5. Massin P, Bandello F, Garweg JG, et al. Safety and efficacy of ranibizumab in diabetic macular edema (RESOLVE Study): a 12-month, randomized, controlled, double-masked, multicenter phase II study. Diabetes Care. 2010;33(11):2399-405. 6. Diabetic Retinopathy Vitrectomy Study Research Group. Early vitrectomy for severe vitreous hemorrhage in diabetic retinopathy. Two-year results of a randomized trial. Diabetic Retinopathy Vitrectomy Study report 2. Arch Ophthalmol. 1985;103(11):1644-52. 7. Diabetic Retinopathy Vitrectomy Study Research Group. Early vitrectomy for severe vitreous hemorrhage in diabetic retinopathy. Four-year results of a randomized trial. Diabetic Retinopathy Vitrectomy Study report 5. Arch Ophthalmol. 1990;108(7):958-64. 8. Nguyen QD, Shah SM, Khwaja AA, et al. Two-year outcomes of the ranibizumab for edema of the macular in diabetes (READ-2) study. Ophthalmology. 2010;117(11):2146-51. |

