 |
Q:
Can a donor cornea from a patient with pseudoexfoliation syndrome (PEX) be used for grafting?
A:
“Technically, yes,” says Christopher Luft, OD, of Woodstock, GA. “Though this multifactorial, systemic microfibrillopathy affects more than meets the eye.”
As technology advances and our understanding of healthy corneal tissue improves, the number of corneas suitable for grafting and transplantation has significantly increased, according to Dr. Luft. While criteria is in place to prevent serious complications for the host, a successful transplant is largely dependent on the donor’s systemic health profile, time-from-death to graft procurement and properly functioning tissue with a focus on the corneal endothelium.1
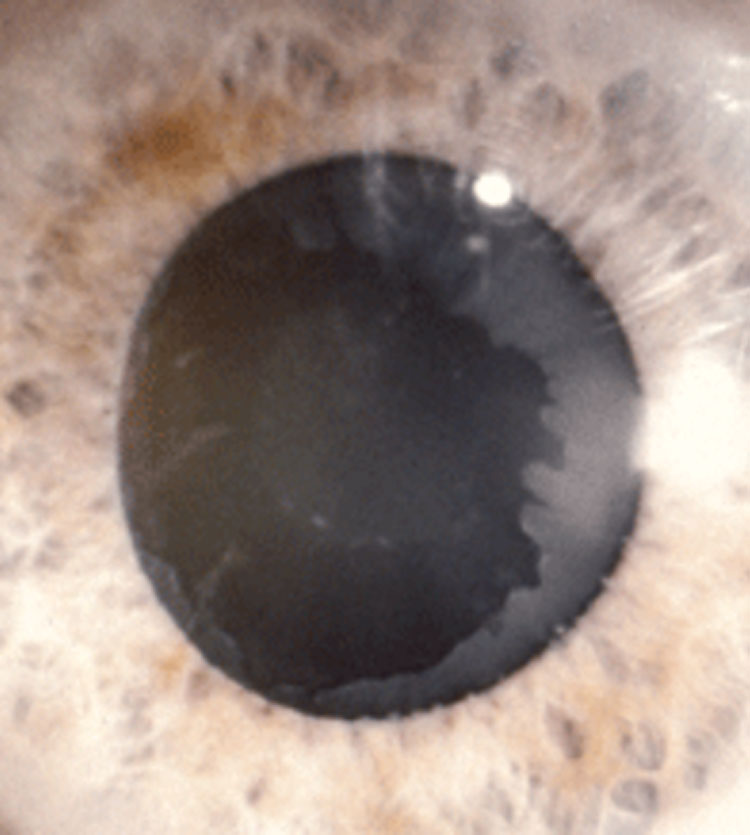 |
| The peripupillary and lenticular fibrillar material in this PEX patient can affect dilation and cause corneal and zonule decompensation and pressure spikes. Photo: Stephen A. Obstbaum, MD. Click image to enlarge. |
Weighing Your Options
A recovery technician first completes an aseptic full body exam to rule out any signs of high-risk behavior, gross pathology and scars or identifiable marks.1 The technician must pay close attention to any medical issues that occurred within the last week of the donor’s life.1
A post-mortem blood draw is then performed and used to identify systemic disease. Infectious diseases, such as hepatitis, HIV, rabies and syphilis, malignancy around the anterior segment of the eye and other infections are contraindications for corneal grafting.1 Neurodegenerative disease, drug use, travel history and acute infections may prohibit donation completely.1
Once a potential donor is determined to be a candidate, the graft is extracted and the corneal tissue is stored.1 Grafts are suitable for transplantation for up to 14 days.1
Assessing PEX
Specular microscopy is an objective way of analyzing the structure of the endothelial cells of the host cornea to determine underlying pathology.1,2 Endothelial cell density must fall within a certain range (around 2000 cells per mm2).1,2 Endothelial cell shape and orientation in the setting of polymegethism and pleomorphism, along with other endotheliopathies, are contraindications, as they affect quality of vision and may lead to graft failure.1
When it comes to PEX, no immediately disqualifiable contraindications exist.2,3 PEX is a systemic, age-related condition characterized by the production and deposition of extracellular, granular material, most notably in the anterior segment of the eye.2-4 If this material is transplanted from the cornea to the host, PEX may cause corneal endothelial cell decompensation by breaking down the hexagonal connections of the endothelium and promoting apoptosis, which can lead to bullous keratopathy and, ultimately, graft failure.2-4 Pre-op cytokine levels and fibrogenic growth factors associated with PEX may also be transferred to the host, causing a pro-inflammatory cascade and progressive damage to corneal tissue.4
With that being said, Dr. Luft notes that it is unknown whether these particles, if transplanted, will multiply and transfer the condition to a healthy cornea and anterior chamber. He adds that his colleagues believe they are an incidental part of the process and wash away with circulating aqueous over time with no visual significance.
Implantation success is directly related to graft health. While there are no upfront contraindications, proceed with caution when transplanting from tissues with PEX to a healthy host. While PEX particles entering a host may not cause lasting adverse effects to the grafted cornea or anterior chamber, the threat of potential complications should not be taken lightly.
| 1. Liaboe C, Vislisel J, Schmidt G, et al. EyeRounds.org. Corneal transplantation: from donor to recipient. EyeRounds.org/tutorials/cornea-transplant-donor-to-recipient. Published May 19, 2015. Accessed August 17, 2020. 2. Palko JR, Qi O, Sheybani A. Corneal alterations associated with pseudoexfoliation syndrome and glaucoma: a literature review. J Ophthalmic Vis Res. 2017;12(3):312-24. 3. Tase S, Shimizu T, Hayashi T, et al. Descemet’s membrane endothelial keratoplasty for pseudoexfoliation syndrome: a case series. BMC Ophthalmol. May 28, 2019. [Epub ahead of print]. 4. Naumann GOH, Küchle M. Primary corneal graft failure. Arch Ophthalmol. 1996;114(8):1031. |

