
Q: I have a patient who has developed post-herpetic neuralgia (PHN) following a severe zoster outbreak that affected the eye. How should I manage this patients pain?
A: The answer depends on whom you ask. H.S. Ghazi-Birry, O.D., M.D., Ph.D., of the Southern College of Optometry in Memphis, Tenn., says to start with 300mg of the anti-epileptic Neurontin (gabapentin, Pfizer) once a day on day one, twice a day on day two and three times a day on day three. If the pain persists, the dose can be titrated up to a maximum of 1,800mg/day, he says.
If the Neurontin is ultimately ineffective, Dr. Ghazzi-Birry says, to prescribe Trileptal (oxcarbaze-pine, Novartis) or Keppra (levetiracetam, UCB Pharma) for a few weeks. Response to one anti-epil- eptic does not predict a response to others, he says.
He adds that he would also have the patient use either a topical 5% lidocaine gel and topical lidocaine patch12 hours on, 12 hours off or employ capsaicin cream to the affected area three to five times daily for at least three weeks.
If this combination therapy does not alleviate the pain, Dr. Ghazi-Birry says the patients age would then play a role in his decision making. If the patient is under age 65, 25mg of either nortriptyline or desipramine (anti-depressants) can be added and increased by 25mg every three weeks with a maximum dosage of 125mg for at least 12 weeks, he says. He recommends nortriptyline because it tends to produce fewer anticholinergic effects, he says. These drugs are best tolerated when started in a low dosage and given at bedtime, he says.
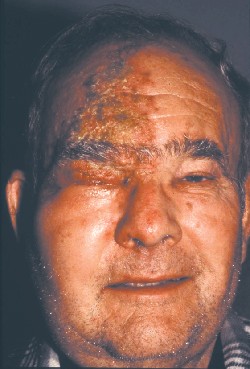 |
| Patients with herpes zoster may have to contend with post-herpetic neuralgia. |
Dr. Ghazi-Birry says he would not prescribe either drug to patients past age 65, due to an increased risk of postural hypotension-induced falls and an increase in intraocular pressure, which can be of particular concern for this age group. Instead, he would have the over-65 patient take one to two tablets of Tylenol #2 or #3 (aceto- minofen and codeine) once every four hours, with a maximum dosage of eight tablets over 24 hours.
If the patient under 65 does not respond to the nortriptyline or
desipramine, prescribe Tylenol #2 or #3 one to two tablets, every four hours, with a maximum of 10 tablets every 24 hours, Dr. Ghazzi-Birry says. (He adds that the dosage of both Tylenols would be less in patients past 65, due to the anticipated inhibition of respiratory drive, which tends to have more of a clinical impact with advancing age.)
If the under-65 patient is on nortriptyline, Dr. Ghazzi-Birry says to switch him or her to Paxil (paroxetine, GlaxoSmithKline) or Zoloft (sertraline HCl, Pfizer), as the use of nortriptyline and Tylenol #2/3 can induce central nervous system depression leading to fogginess, excessive sedation and reduction in mental sharpness. Finally, if neither age-appropriate treatment works, Dr. Ghazi-Birry says, refer the patient to a pain clinic.
Thomas Boland, M.D., of Scran- ton, Pa., says treatment depends on how long the patient has had PHN. If the patient develops it in the immediate post-op or post-herpetic period (within the first month or six weeks), I would probably start him or her off on an oral steroid, such as prednisone 40mg once a day, he says. Then, I would taper the prednisone over the next two to three weeks depending on how the patient is doing.
If the PHN is significant at three months after the zoster outbreak, Dr. Boland says he would prescribe 10mg of amitriptyline to be taken at bedtime. He adds that the dosage would be doubled every couple of weeks, if needed, and that he would couple the amitriptyline with 500mg of Valtrex (valacyclovir HCl, GlaxoSmithKline) once a day, indefinitely, to suppress any inflammation stemming from the herpes zoster outbreak.

