 |
Q:
I have a patient who had LASIK two years ago and presented with a traumatic corneal abrasion. After the defect healed, I was surprised to see what looked like DLK. What gives?
A:
We most commonly think of diffuse lamellar keratitis (DLK) as a complication in the immediate postoperative days following LASIK. “Although rare, DLK can be a potentially devastating complication after LASIK, and we are all taught to keep a keen eye out for this flap-based inflammatory response at the early stage post-operative visits,” says Chris Kruthoff, OD, of Northwest Eye Clinic in Golden Valley, MN. “However, this sterile inflammatory response can occur at any point, even years after this procedure, with any traumatic manipulation of the epithelium or flap.”
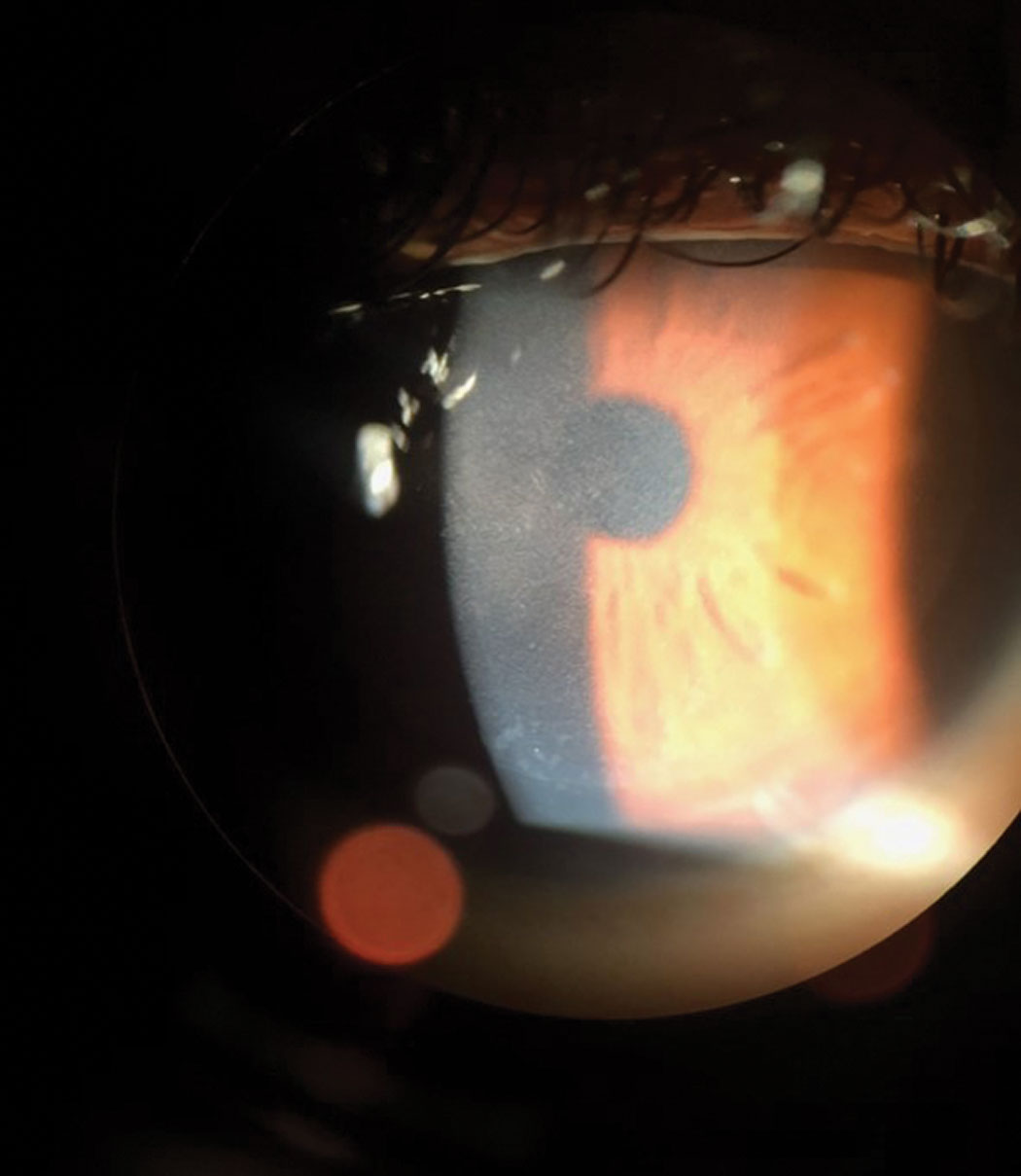 |
| Keep DLK in mind with any potential insult to the cornea down the road. Click image to enlarge. |
Sterile or Infectious?
The presence of diffuse anterior stromal inflammation after an abrasion should lead to one major question—is this a sterile response, or is this infectious? “Infectious keratitis should always remain the top concern after any corneal abrasion,” notes Dr. Kruthoff. Key findings include anterior chamber reaction, worsening pain, a non-healing epithelial defect and infiltrate formation. “While the corneal inflammation was troubling, we were confident it was non-infectious, with no anterior chamber reaction and the patient noting only mild discomfort.”
Based on these considerations and the clinical picture at hand, a diagnosis of Stage 2 DLK secondary to the corneal abrasion was made.
Hit It Hard
DLK presents as a collection of small, fine corneal infiltrates and forms at the interface of the corneal flap following LASIK. The condition can be graded on a four-stage scale as follows:
- Stage 1—Peripheral white blood cell accumulation with a clear central cornea.
- Stage 2—Diffuse spreading of these inflammatory cells across the entire cornea including the central cornea.
- Stage 3—Accumulation and clumping of white blood cells centrally. This stage is critical, as prompt flap lifting and irrigation is warranted to prevent corneal scarring and permanent vision decrease.
- Stage 4—Further corneal scarring and stromal melt. This stage is very rare and is associated with hyperopic shift and vision loss.
With any occurrence of DLK, either in the immediate post-op period or more long term such as this case, institute aggressive steroid therapy to prevent progression to the later stages. In this case, the patient was instructed to increase her prednisolone to one drop every hour while awake, with daily follow-up visits to ensure that she did not progress to the critical Stage 3 threshold.
“In my experience, DLK may take up to two days to show true improvement and decrease in staging as the steroid builds to counter the inflammatory response,” says Dr. Kruthoff. After increasing the steroids, the patient returned the next day to ensure that the condition was improving. By the following day, the DLK was showing clear signs of regression. “We initiated a very slow steroid taper, and, by two weeks out, her cornea had completely cleared with uncorrected visual acuity of 20/20,” Dr. Kruthoff said.
The presence of DLK can be a very concerning finding for doctor and patient alike. Consulting with a cornea specialist or the original LASIK surgeon is always a good idea if the diagnosis is uncertain. Occasionally, prompt flap irrigation may be needed. While we most often associate DLK with the immediate postoperative period following LASIK, keep this condition in mind with any potential insult to the cornea down the road.
“DLK can be a potential sequelae to ocular surface trauma at any point after LASIK,” says Dr. Kruthoff. “Prompt diagnosis and aggressive management may quite well save your patient’s vision.”

