When we hear about punctal plugs, the first thing that comes to mind is dry eye treatment. Although frequently used for this purpose, there are several other conditions in which punctal occlusion can be implemented into your treatment plan. Indeed, punctal and canalicular occlusion may enhance the effects of topical medications, help catalyze postoperative healing and improve contact lens wear.
Here, I’ll review how punctal occlusion may be used to treat not only dry eye syndrome (DES) but other ocular surface conditions. Also, I’ll discuss several non-traditional uses for occlusion that may greatly enhance your patient’s overall ocular health and comfort.
The Traditional Use for Occlusion
The most common indication for punctal occlusion is DES.1 This multifactorial disease of the tears and ocular surface results from insufficient tear production, excessive tear evaporation or abnormal tear composition.2,3 DES causes symptoms of burning, itching, redness, photophobia and reduced visual acuity.2,4,5
Multiple studies have shown that nearly five million Americans age 50 or older are affected significantly by DES.6 Additionally, millions more Americans experience varying, less severe symptoms of DES.
There are many underlying risk factors for dry eye, including age, female gender, systemic diseases, medications, environmental considerations, contact lens wear and refractive eye surgeries.7 The Beaver Dam Eye Study showed that age was the biggest contributory factor to dry eye syndrome.7 And, because a large percentage of Americans are now more than 50 years of age, we can expect to see even more patients present with dry eye symptoms.
There are two subcategories of DES: aqueous-deficient and evaporative. Aqueous-deficient causes include Sjögren’s syndrome, lacrimal gland insufficiency, lacrimal duct obstruction and reflex hyposecretion.2 Evaporative mechanisms include meibomian gland dysfunction, eyelid aperture disorders, lid-globe incongruity, blink disorders and ocular surface irregularites.2
Types of Occlusion
Punctal occlusion may be performed in a variety of ways:
• Temporary occlusion with collagen plugs may help identify patients who
likely would benefit from permanent occlusion, or may be an ideal
option for individuals who are apprehensive about more permanent
treatment options. Collagen plugs typically dissolve within four to
seven days.
• Semi-permanent occlusion with punctal plugs are comprised of silicone
or thermal labile acrylic polymers, and may last for several months.
• Permanent occlusion can be achieved with the use of silicone plugs and
thermal or laser cautery. While silicone plugs do not dissolve, it is
important to note that they may extrude or migrate out of the puncta
over time.
Irrespective of the subcategory, DES produces tear hyperosmolarity and/or ocular surface inflammation. Tear hyperosmolarity can be caused by either low aqueous flow of excessive tear film or excessive tear film evaporation––both of which can damage the ocular surface by causing an epithelial inflammatory response.2,8
Proper diagnostic testing for DES often helps guide treatment decisions. Diagnostic screening assesses tear film stability, tear production and flow, and ocular surface stability. Typical tests for DES include tear film break-up time, Schirmer testing, corneal topography, impression cytology, and rose bengal, lissamine green or fluorescein dye testing.2 Additionally, tear film osmolarity testing (i.e., TearLab) has been used to identify dry eye patients.
No matter which testing you perform, the first step to effective DES management is to determine whether the patient has ocular surface inflammation. If so, you should consider the use of anti-inflammatory therapies, such as cyclosporine and omega-3 fatty acids supplementation, to optimize ocular surface health before recommending punctal occlusion.
Sometimes, a short course of topical steroids––used simultaneously with the initiation of cyclosporine––will help reduce the sting, allow for rapid symptomatic relief, and/or facilitate the long-term success of cyclosporine dosing. Implementing this strategy to first identify patients with inflammation prevents the potential accumulation of inflamed tears after punctal occlusion, which may exacerbate the ocular surface disease.
The Dry Eye Workshop (DEWS) and the International Task Force (ITF) Delphi Panel on Dry Eye outlined the primary signs and symptoms that could be used to determine DES severity.9 More specifically, the ITF created a four-tier, step-wise approach to DES grading and management:3,9
• Severity Level 1 includes mild to moderate signs and no symptoms. Recommended treatment includes patient education and artificial tears.
• Severity Level 2 includes moderate to severe symptoms, tear film signs, mild corneal punctate staining, conjunctival staining and visual signs. Recommended treatment includes preservative-free artificial tears, gels, ointments, nutritional supplements, cyclosporine A and topical corticosteroids. (Most patients present to our offices when they reach Level 2 signs and symptoms.)
• Severity Level 3 includes severe symptoms, marked corneal superficial punctate keratitis, central corneal staining and filamentary keratitis. Recommended treatment includes all Level 2 options as well as tetracyclines and punctal plugs.
• Severity Level 4 includes severe symptoms, such as significant corneal staining, corneal erosion and conjunctival scarring. Recommended treatment includes systemic anti-inflammatory therapy, oral cyclosporine, moisture goggles, acetylcysteine and punctal cautery.2,9
Again, many patients who suffer from DES have found success with topical artificial tears and anti-inflammatories as well as omega-3 fatty acid supplementation. Whether using medications short- or long-term, ocular surface diseases are chronic, co-morbid conditions that wax and wane over time.
Although many practitioners have been able to effectively treat DES with various medications, such as topical cyclosporine, punctal occlusion is often a forgotten adjunct tool.
Importance of Patient Education and Punctal Occlusion
Be sure to communicate these points to your patients when considering occlusion:
• Punctal occlusion is a safe, quick, reversible and widely performed procedure.
• Punctal plugs help alleviate symptoms of dry eye, but do not cure the disease.
• Punctal plugs will help increase the contact time of your drops.
• Punctal plugs will not interfere with tear production.
• Collagen plugs are temporary and are often used for diagnostic purposes.
• Permanent silicone plugs do not dissolve and can be removed if complications arise.
One reason for this potential oversight may be related to the current FDA labeling of Restasis (cyclosporine, Allergan), which indicates that increased tear production was not documented in patients who were taking topical anti-inflammatory drugs or using punctal plugs.10 This, however, does not mean that these patients did not experience tear production.
Because patients with punctal plugs already have increased tear volume due to mechanical blockage––and those on anti-inflammatory agents show decreased inflammation associated with many of the symptoms of dry eye––it was more difficult to document statistical improvement in these patient groups.10
In 2007, Calvin Roberts, M.D., and associates noted a synergistic effect with punctal occlusion and topical cyclosporine use.11 They concluded that, “while topical cyclosporine is being used more and more for the treatment of moderate dry eye, our study results indicate clinicians should not abandon punctal plugs nor consider punctal plugs and cyclosporine mutually exclusive.”11
Non-traditional Uses for Occlusion
According to the ITF, punctal occlusion is recommended for dry eye patients at Severity Level 3.2 However, punctal plugs can be used to treat conditions other than dry eye that may disrupt normal tear volume and balance.
• Compliance issues. Punctal plugs may play an indirect role in addressing patient non-compliance. Factors that influence patient compliance include: cost of medication, dosing schedule, inability to take drops/meds, forgetfulness, poor understanding of the condition and insufficient trust in their doctors. No matter the reason, poor compliance and adherence to our recommendations can have a significant impact on final outcome.
Simpler, less frequent dosing results in better compliance in a variety of therapeutic classes.12 Additionally, plugs are not dependent on patient adherence or dexterity for therapeutic efficacy. In fact, punctal plugs may help eliminate compliance issues by reducing the need for consistent artificial tear instillation.11 Furthermore, punctal occlusion increases the residence time of topical therapeutic agents that may be prescribed to address other co-morbid conditions, such as ocular surface disease.11,12
• Contact lenses. Patient discomfort is the leading reason for contact lens dropout. When compounded with poor lens care compliance, discomfort can make successful management of the contact lens wearer almost impossible.
Multiple factors can help facilitate an optimal contact lens wear experience, including good ocular and systemic health, proper lens care, satisfactory compliance, and the type of contact lens material. Once lens wear is optimized, contact lens rewetting drops and punctal occlusion are viable options to address comfort throughout the day and increase tear volume. One study indicated that patients with punctal plugs experienced a 34.6% increase in contact lens comfort within three weeks of occlusion.13
The best way to maximize contact lens success is to evaluate the ocular surface prior to the initial fit. If patients show any signs or symptoms of ocular surface disease, treat it accordingly. If patients present with any signs of conjunctival or corneal staining, topical therapy and punctal occlusion may be indicated.
You may need to consider both the lens material and wear schedule for your patients, and transition them into daily wear lenses with low water content, if necessary. Once improved, the patient will be ready to wear contact lenses comfortably. Additionally, making patients comfortable and happy will keep them in their lenses longer and may prevent them from seeking refractive surgical options.
• Acute ocular conditions. As primary eye care providers, we often encounter patients who present with various acute conditions. Although the signs and symptoms may vary, patients often come to us for our expert medical opinion.
Depending on the presentation, appropriate treatment options may include topical lubricants, antibiotics, steroids and combination medications. According to our corneal specialist, John Sheppard, M.D., temporary punctal occlusion increases the contact time of topical medications, which allows the drugs to penetrate into ocular surface tissues and render their desired effect with greater efficacy.
Complications of Occlusion
With the exception of thermal/laser
cauterization, punctal occlusion is a reversible procedure that is
widely used within eye care. Regarding most types of plugs, the safety
profile is very high; epiphora, conjunctival irritation and extrusion
typically are the most common––yet infrequent––complications.
Other rare
complications include canaliculitis and dacryocystitis, which are
caused by common bacterial pathogens, such as Actinomyces israelii,
staphylococci, streptococci and diphtheroids. In the event of
complications, patients may require plug removal as well as therapeutic
treatment anti-inflammatories and antibiotics. Rarely, surgical removal
of plugs is indicated.
Common conditions in which punctal occlusion may yield some benefit include corneal infiltrates, corneal abrasions, recurrent corneal erosions, filamentary keratitis, superior limbic keratitis, trachoma and neurotrophic keratopathy.
A recent example in our clinic was a 32-year-old white male who was referred for a bacterial corneal ulcer secondary to contact lens wear. He presented with pain O.S., mild mucous discharge and light sensitivity. Clinical findings included 1+ lid edema, 3+ conjunctival injection, 3.0mm mid-peripheral corneal ulcer at 5 o’clock and 1+ anterior chamber cells. We performed cultures to determine the causative pathogen.
We prescribed homatropine 5% t.i.d. O.S., moxifloxacin 0.3% q1h (throughout the night) O.S., a 0.4mm temporary collagen plug O.S. (lower puncta) and had him return the following day. Upon examination, the infection improved with resolution of the cellular reaction and the medications were continued for the following week until complete resolution. Although the condition could have improved without occlusion, the punctal plugs helped increase the contact time of the medications.
• Glaucoma. Similar to topical treatment of ocular surface disease, punctal occlusion may benefit glaucoma patients by increasing the penetration and efficacy of IOP-lowering medications. Additionally, occlusion may decrease systemic absorption of glaucoma medications, such as beta blockers, and therefore reduce unwanted side effects. One study group found that nasolacrimal duct occlusion reduces the amount of systemic absorption by up to 60%.14 Nonetheless, clinical studies have found conflicting results regarding the statistical significance of punctal occlusion for glaucoma therapy.15,16
• Prevention of herpes simplex keratitis (HSK) reactivation. Herpes simplex virus (HSV) is the most common cause of corneal blindness secondary to infection in the United States and developed countries.17 The recurrence rate of ocular HSV within two years ranges from 23% to 33%, and about 20% to 25% of those with ocular HSV infections develop T-cell mediated stromal HSK. In addition to stromal inflammation, HSK patients often exhibit decreased tear production and dry eyes.18,19
Thermal cautery could facilitate therapy simply by enhancing the effectiveness of topically applied drugs. Both thermal cautery and cyclosporine discourage HSV reactivation by targeting dry eye, improving tear film quality and decreasing ocular surface irritation.20
Interestingly, Dr. Sheppard suggested that punctal occlusion––in conjunction with topical cyclosporine––might reduce the frequency and duration of HSV recurrences and consequently minimize the risk of serious ocular damage.20 This may be a more agreeable option for patients who are wary about the permanence of cauterization.
• Refractive surgery. Optometrists play an integral role in the peri-operative care of refractive surgery patients. Whether patients are undergoing cataract surgery with premium IOL implantation, laser vision correction, or any other ocular surgical procedure (pterygium removal, glaucoma surgery, etc.), an ocular surface evaluation is an essential aspect of the preoperative evaluation.
Prior to any ocular surgery, our role is to prepare the ocular surface in order to maximize patient outcomes as well as minimize the risk for surgical complications. Pre-existing ocular surface disease, such as DES, can have a tremendously negative impact on the accuracy of the preoperative measurements and overall patient comfort throughout the procedure.
If we can identify these dry eye patients and aggressively treat their ocular surface with artificial tears, anti-inflammatories, nutriceuticals and/or punctal occlusion before surgery, we can ensure a more favorable postoperative outcome. Although punctal plugs cannot address all preoperative ocular surface concerns, occlusion can help address tear volume levels.
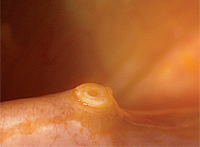
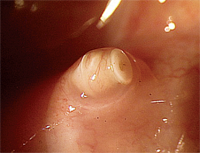
Proper fit of the Odyssey Parasol Plug (left). Pyogenic granuloma formation following punctal plug insertion (right).
The incidence of dry eye after cataract surgery may be as high as 87%.21 Both cataract surgery and laser vision correction transects the corneal nerves, causing deinnervation that typically persists for one to three months following the procedure.
This may produce a neurotrophic cornea, as well as yield clinical signs of epitheliopathy with little to no symptoms other than decreased visual acuity. Other consequences of postoperative dry eye include ocular discomfort, decreased or fluctuating vision and refractive regression.
Whenever patients present with decreased vision following refractive surgery, aggressive ocular surface treatment may determine whether patients need additional surgery. Punctal occlusion may be a viable alternative for these individuals.
Additionally, punctal occlusion promotes wound healing and better visual acuity after certain refractive procedures, such as LASEK. One study documented a lower fluorescein staining score, a better uncorrected distance acuity, and a lower incidence of haze in LASEK patients who received punctal plugs.22
Future Developments in Punctal Occlusion
Currently, punctal plug delivery systems are being developed that can distribute a sustained time-release dose of glaucoma medication over a three-month period.23 The Punctal Plug Delivery System (QLT Inc.) is designed to provide a consistent dose of prostaglandin analog in glaucoma patients.
The initial results of the technology’s phase II clinical study revealed that 60% of subjects experienced an IOP reduction of 5mm Hg or greater at four-week follow-up.23 Even more impressive, the Punctal Plug Delivery System’s four-week retention rate was 95%.23 Clearly, such a device could markedly reduce compliance issues for glaucoma patients.
Optometry plays an integral role in the treatment and management of many ocular surface conditions. Today, we have several treatment options to address not only DES, but also many other conditions that could be improved by increased tear volume and medication efficacy.
Although punctal plugs chiefly have been used to treat dry eye conditions, practitioners now can consider other potential therapeutic benefits.
Dr. Whitley is the director of optometric services at Virginia Eye Consultants in Norfolk, Va.
1. Baxter SA, Laibson PR. Punctal plugs in the management of dry eyes. Ocular Surface. 2004 Oct;2(4):255-65.
2. McDonald M, D’Aversa G, Perry HD, et al. Hydroxypropyl cellulose ophthalmic inserts (lacrisert) reduce the signs and symptoms of dry eye syndrome and improve patient quality of life. Trans Am Ophthalmol Soc. 2009 Dec;107:214-21.
3. Hardten D. Managing dry eye. Ophthalmol Management. 2008 Aug.
4. Perry HD. Dry Eye Disease: Pathophysiology, Classification, and Diagnosis. Am J Manag Care. 2008 Apr;14(3 Suppl):S79-87.
5. Wester S. Punctum plugs: highly engineered treatment for dry eye. Available at:
www.ophthalmologyweb.com/Tech-Spotlights/26480-Punctum-Plugs-Highly-Engineered-Treatment-for-Dry-Eye (accessed December 20, 2011).
6. Moss SE, Klein R, Klein BE. Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol. 2000 Sep;118(9):1264-8.
7. Moss SE, Klein R, Klein BE. Incidence of dry eye in an older population. Arch Ophthalmol. 2004 Mar;122(3):369-73.
8. Suzuki M, Massingale M, Ye F, et al. Tear osmolarity as a biomarker for dry eye disease severity. Invest Ophthalmol Vis Sci. 2010 Sep;51(9):4557-61.
9. Behrens A, Doyle JJ, Stern L, et al. Dysfunctional tear syndrome: a delphi approach to treatment recommendations. Cornea. 2006 Sep;25(8):900-7.
10. Data on file, Allergan.
11. Roberts CW, Carniglia PE, Brazzo BG. Comparison of topical cyclosporine, punctal occlusion, and a combination for the treatment of dry eye. Cornea. 2007 Aug;26(7):805-9.
12. Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001 Aug;23(8):1296-310.
13. Giovagnoli D, Graham SJ. Inferior punctal occlusion with removable silicone punctal plugs in the treatment of dry-eye related contact lens discomfort. J Am Optom Assoc. 1992 Jul;63(7):481-5.
14. Zimmerman TJ, Kooner KS, Kandarakis AS, Ziegler SP. Improving the therapeutic index of topically applied ocular drugs. Arch Ophthalmol. 1984 Apr;102(4):551-3.
15. Opitz DL, Tung S, Jang US, Park JJ. Silicone punctal plugs as an adjunctive therapy for open-angle glaucoma and ocular hypertension. Clin Exp Optom. 2011 Sep;94(5):438-42.
16. Bartlett JD, Boan K, Corliss D, Gaddie IB. Efficacy of silicone punctal plugs as adjuncts to topical pharmacotherapy of glaucoma-a pilot study. Punctal Plugs in Glaucoma Study Group. J Am Optom Assoc. 1996 Nov;67(11):664-8.
17. Judge A, Assil K. E-Medicine. Herpes simplex. Available at:
www.emedicine.com/oph/topic256.htm (accessed November 13, 2011).
18. Doymaz MZ, Rouse BT. Herpetic stromal keratitis: an immunopathologic disease mediated by CD4+ T lymphocytes. Invest Ophthalmol Vis Sci. 1992 Jun;33(7):2165-73.
19. Keijser S, van Best JA, Van der Lelij A, Jager MJ. Reflex and steady state tears in patients with latent stromal herpetic keratitis. Invest Ophthalmol Vis Sci. 2002 Jan;43(1):87-91.
20. Sheppard JD, Wertheimer ML, Scoper SV. Modalities to decrease stromal herpes simplex keratitis reactivation rates. Arch Ophthalmol. 2009 Jul;127(7):852-6.
21. Kojima T, Watabe T, Nakamura T, et al. Effects of preoperative punctal plug treatment on visual function and wound healing in laser epithelial keratomileusis. J Refract Surg. 2011 Dec;27(12):894-8.
22. Albietz JM, Lenton LM, McLennan SG. Chronic dry eye and regression after laser in situ keratomileusis for myopia. J Cataract Refract Surg. 2004 Mar;30(3):675-84.
23. QLT Announces Encouraging Phase II Data from CORE Study Drug Delivery System. Available at:
www.qltinc.com/newsCenter/2011/110829.htm (accessed December 20, 2011).

