A 35-year-old white male presented complaining of blurred vision in both eyes for the past two weeks. His ocular history is unremarkable, but his medical history is significant for type 1 diabetes for the past 25 years. He takes insulin shots daily and reports that his blood sugar fluctuates. He did not know his blood sugar levels nor was he aware of his glycosolated hemoglobin (HbA1c) levels.

Best-corrected visual acuity was 4/200 in the right eye and 20/60 in the left. Confrontation visual fields were restricted in the right eye, but were full to careful finger counting in the left. Pupils were sluggishly reactive with a 2+ relative afferent pupillary defect in the right eye.
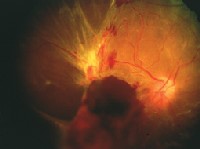
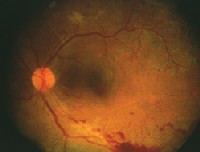
The anterior segment exam was unremarkable, and there was no iris neovascularization in either eye. IOP measured 16mm Hg O.U. We observed changes throughout the retina of each eye during the dilated fundus exam, as seen in the photos.
The dilated fundus exam (O.D. left, O.S. right) showed obvious hemorrhagic changes.
Take the Retina Quiz
1. What is the likely cause of the fundus changes seen O.U.?
a. Diabetic retinopathy.
b. Central retinal vein occlusion.
c. Eales disease.
d. Sclopteria.
2. How would you further characterize the fundus changes O.D.?
a. High-risk proliferative diabetic retinopathy (PDR).
b. Retinal detachment.
c. Vitreous hemorrhage.
d. All of the above.
3. How would you further characterize the fundus changes O.S.?
a. High-risk PDR.
b. PDR but not high-risk.
c. Retinal detachment.
d. Vitreous hemorrhage.
4. Which treatment will this patient likely undergo O.D.?
a. Panretinal photocoagulation (PRP).
b. Vitrectomy, membrane peel and endolaser.
c. Silicone oil.
d. Both b and c.
5. Which treatment option(s) is indicated O.S.?
a. PRP.
b. Vitrectomy, membrane peel and endolaser.
c. Silicone oil.
d. Both b and c.
6. What do we consider a normal HbA1c level in diabetic patients?
a. Less than 6%.
b. Less than 7%.
c. Less than 8%.
d. Less than 9%.
For answers, click here.
Discussion
This patient is in the advanced stages of proliferative diabetic retinopathy (PDR). This resulted in his severe vision loss.
It is sad that patients such as this one continue to present with severe vision loss from the advanced stages of proliferative diabetic retinopathy, especially when we have information from the numerous multi-centered clinical trials that can help avoid vision loss from diabetic retinopathy.
Diabetic patients should strive to keep fasting blood sugars below 140mg/dl and preferably closer to 70-120mg/dl. The HbA1c level is perhaps the most important barometer of blood sugar control. Glycosylated hemoglobin forms when glucose in the blood attaches to the hemoglobin. Blood cells typically stay in circulation for two to three months, so the HbA1c level is a good measure of a persons average blood glucose level during that period. If the blood sugar has been high during the previous few months, the HbA1c level will be high. Normal HbA1c levels are less than 6.5%. Diabetics should strive for levels of less than 7%.1
Our patient obviously has been negligent in caring for his diabetes. He admitted that blood sugar was poorly controlled and that he was not aware of his HbA1c levels. Lack of attention to these details was predictive for what was taking place in his retinasand probably the rest of his body.
Our patients right eye clearly shows the presence of vitreous hemorrhage, extensive fibrovascular proliferation and a total tractional retinal detachment. The changes in this eye obviously have been going on for much longer than the two weeks that our patient has been symptomatic. Those symptoms more likely reflect his left eye, which is not as bad.
On careful exam we can see the presence of pre-retinal and vitreous hemorrhage along the inferior temporal quadrant in the left eye that was related to retinal neovascularization in this area. He also has some fine neovascularization on his disc. Both eyes reflect high-risk PDR.
The National Eye Institutes landmark Diabetic Retinopathy Study, published in the late 1970s, provided a scientific basis for panretinal photocoagulation (PRP) in eyes with high-risk PDR. This study, the first and largest collaborative controlled clinical trial in the history of ophthalmology at the time, found that PRP reduced the overall rate of severe vision loss (less than 5/200) by 50% and in treated eyes decreased the rate of severe vision loss from 15.9% to 6.4%.2,3
The Diabetic Retinopathy Study also established high-risk groups with PDR that benefit from immediate PRP. High-risk PDR involves any of the following conditions:
Neovascularization of the disc (NVD) greater than or equal to one-third to one-fourth of the disc area in size.
NVD with preretinal or vitreous hemorrhage.
Neovascularization elsewhere greater than or equal to one-half the disc area with preretinal hemorrhage.
The Diabetic Retinopathy Study found that severe vision loss develops in 25-40% of patients in the high-risk group within two years without treatment.3
Our patient clearly had high-risk PDR in both eyes; the right was much worse than the left. The patient underwent pars plana vitrectomy, membrane peel, endolaser, scleral buckle procedure and silicone oil injection in the right eye. The final visual outcome was 5/200.
The patient underwent PRP in the left eye, which resulted in an involutional response of the neovascularization. Vision in that eye eventually stabilized with a 20/40 visual acuity.
1. Powers AC. Diabetes mellitus. In: Braunwald E, Fauci AS, Hauser SL, et al. Harrisons Principles of Internal Medicine. 15th ed., New York: McGraw Hill, 2001:2109-37.
2. The Diabetic Retinopathy Study Research Group: Indications for photocoagulation treatment of diabetic retinopathy. Diabetic Retinopathy Study Report Number 14. Invest Ophthalmol Clin 1994;27:239-53.
3. The Diabetic Retinopathy Study Research Group: Four risk factors for severe visual loss in diabetic retinopathy: The third report from the Diabetic Retinopathy Study. Arch Ophthalmol 1979 Apr;97(4):654-5.

