 |
Q:
A 26-year-old female with sector injection presented with a history of a week on topical prednisolone QID with no improvement. What is my next step, and what are other differential diagnoses?
A:
“In my experience, it’s unusual for simple episcleritis to be unresponsive to topical steroids after seven to 10 days,” says Steven Ferrucci, OD, chief of optometry at the Sepulveda VA Ambulatory Care Center and Nursing Home in North Hills, CA. “Nodular episcleritis, which is less common and characterized by a raised nodule within the affected area, tends to last longer and may take up to two to four weeks to resolve.”
If the episcleritis has not responded after a week or two, and the clinician is confident in their diagnosis, Dr. Ferrucci advises increasing the topical prednisone to a pulse dose, say every two hours for four days, or change steroids. “Durezol (difluprednate, Novartis) is a great choice and worth a try before switching to or adding orals,” says Dr. Ferrucci. Adding an oral NSAID such as ibuprofen or indomethacin for a few weeks is often useful as well. “I typically prefer ibuprofen, 800mg three times a day, as it is relatively inexpensive, available over the counter and many patients already have it in their medicine cabinet,” he says.
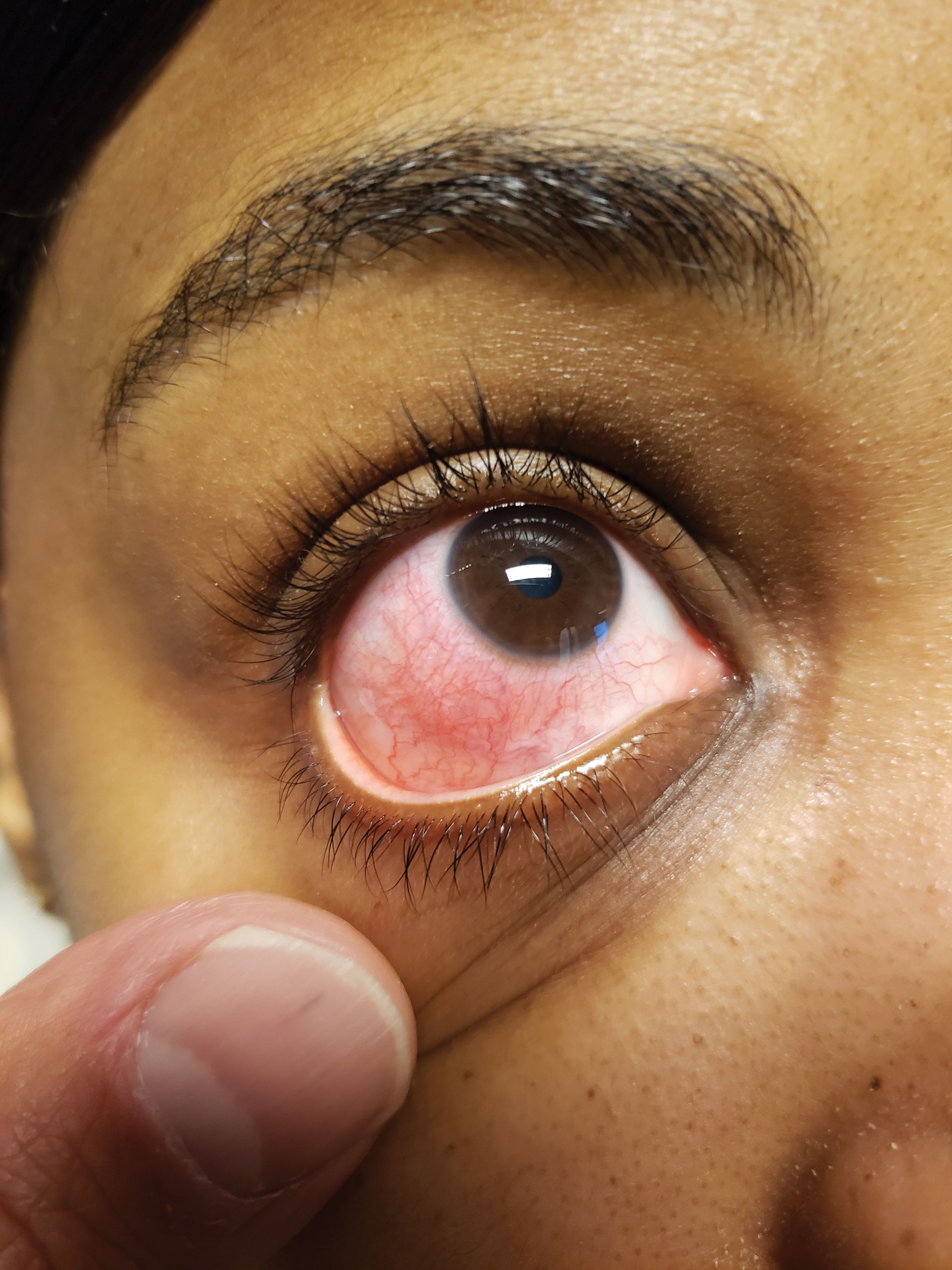 |
| Consider underlying systemic conditions first before diagnosing episcleritis. Click image to enlarge. |
Workups
The vast majority of episcleritis is idiopathic and not associated with underlying systemic disease, but approximately 25% or so may be linked to systemic disease, with the most common condition being rheumatoid arthritis. This patient later admitted to this diagnosis, so Dr. Ferrucci recommends a thorough review of systems, as well as lab testing to look for an underlying cause.
Patients with nodular episcleritis, or those with severe and recurrent/persistent diffuse episcleritis may require a limited workup. Include complete blood count with differential, antinuclear antibody, rheumatoid factor, erythrocyte sedimentation rate, venereal disease research laboratory test and a fluorescent treponemal antibody absorption test.
A chest X-ray can help rule out some of the most common underlying diseases such as rheumatoid arthritis and lupus. If you suspect an underlying systemic disease, you might want to refer to their primary care physician or directly to a rheumatologist who can do a more extensive investigation.
“Of course, it is always a good idea to reconsider the initial diagnosis,” Dr. Ferrucci says. One of the leading causes of sector injection that may throw clinicians off is a conjunctival abrasion. Before you jump to the diagnosis of episcleritis, be sure you stain with fluorescein to rule out a defect that would best be treated with an antibiotic, not a steroid. Bacterial conjunctivitis, phlyctenular conjunctivitis, subconjunctival hemorrhage and scleritis should also be on the differential list.
Perhaps the most important to rule out is scleritis, which typically does not respond to topical agents and requires systemic anti-inflammatory control, Dr. Ferrucci notes. One hallmark of scleritis is a deep, boring eye pain not present with episcleritis. Other signs may include an anterior chamber reaction and reduced visual acuity.
Blanching
According to Dr. Ferrucci, some practitioners advocate the use of 2.5% phenylephrine to aid in the diagnosis. The phenyl will blanch the superficial conjunctival and episcleral vessels but will not blanch the deeper scleral vessels. If the patient’s eye clears up with installation, the diagnosis of episcleritis is strengthened. If the eye does not clear up, scleritis should be considered.
Once all the differentials are considered and everything but episcleritis is ruled out, don’t be timid in your use of topical steroids, and don’t forget to consider underlying systemic conditions. A consult to the appropriate specialist could make a big difference in the patient’s health.

