Practitioners have been called upon to adopt an unprecedented amount of flexibility due to the uncertainties caused by the COVID-19 pandemic. Business plans that were forward-looking into one-, three- or even five-year periods must now require significant revision. It may seem odd to discuss adding new services to your practice while trying to recover losses to your core business, but it is essential to address both the immediate needs and the growth of your practice. Looking for ways to capture new patients, offer new services to existing patients and grow your practice remain crucial aspects of your business even during a crisis.
In his venerable work Out of the Crisis, W. Edwards Deming presented 14 key management points.1 The first of which is, “Create constancy of purpose toward improvement of product and service, with the aim to become competitive, to stay in business and to provide jobs.” You can leverage existing resources to add orthokeratology (ortho-K) to your practice without a large capital investment. This article offers both strategic and practical ideas on how to incorporate ortho-K into your business plan.
Setting up a comprehensive myopia management program includes considerations of behavioral changes (e.g., more outdoor time), anti-muscarinic agents (primarily low-dose atropine), soft multifocal contact lens and overnight ortho-K interventions.2,3
Ortho-K lenses are sometimes, although rarely, prescribed for use during the day. Our colleagues outside the United States have access to other options, including novel spectacle lens designs, which are projected to become available in the United States in 2022.4-6 Even if you do not have access to, or choose not to offer, pharmacological or spectacle interventions, you can offer the contact lens options. Regardless, remain informed of approved and off-label technologies and future developments. If you don’t, your patients or their parents will.
 |
|
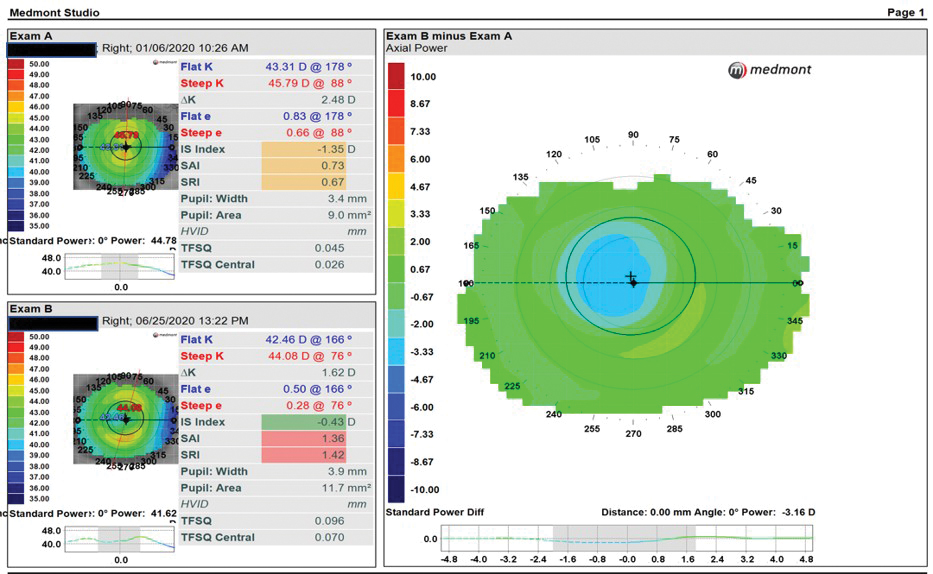
Fig. 1. Subtractive axial maps in a successful ortho-K fit show successful reduction of refractive error and a well-centered treatment zone over the pupil. Click image to enlarge. |
Program Administration
When dealing with special populations such as pediatric patients, you must obtain informed consent from the parents and assent from the patient, if possible. This process varies across the globe, but informed consent must be provided verbally and in writing with signatures from the responsible parties.7,8 Copies of these documents should be retained in the patient’s file.
Provide the parent a packet of materials that includes the informed consent document, discussion of the procedure and device prescribed, schedule of visits, discussion of fees and what they cover, payment plans, warranties, how lost or damaged lenses will be replaced and cancellation policies. Also include training materials, a care kit, instructions for lens care and the handling and wearing schedule. Provide clear guidance on what to do if they experience an adverse event and provide your after-hours contact information.
Indications
Ortho-K lenses are enjoying a resurgence due to the worldwide myopia epidemic. They represent approximately 8% of the rigid contact lens market (0.7% of all contact lens fits) in the United States and 3% of all lens fits worldwide (range <1% to 30%).9,10 The FDA requires optometrists to complete a certification course for each design before they can offer them in their practice (Table 1).11 The indications for ortho-K include the temporary reduction of myopia, slowing of myopia progression and as an alternative for soft contact lens wearers experiencing dry eye.1,11,12
Table 1. Comparison of Indications for Some FDA-approved Ortho-K Lens Designs in the United States | |||
| Product | Manufacturer | Sphere Limit (D) | Cylinder Limit (D) |
| Corneal Refractive Therapy (CRT) | Paragon Vision Sciences/Cooper Vision | Up to -6.00 | Up to -1.75 |
| Emerald | Euclid Systems | Up to -5.00 | Up to 1.50 WTR/-0.75 ATR |
| *Vision Shaping Treatments *(VST) | Bausch + Lomb | -1.00 to -5.00 | Up to -1.50 |
(*VST includes a family of 15 different designs)
Ortho-K Candidates
Above all else, the patient and/or parent needs to be motivated to partner with you in their care over an extended period of time.Ortho-K does not permanently correct myopia, and clinicians must carefully assesss patient and parent expectations. Also, the effects regress after cessation of wear at variable rates for individual patients. Elimination or even slowing of myopia progression cannot be guaranteed, and adverse events (though uncommon) do happen. Patients with histories of non-compliance, allergies, preexisting lid or corneal disease may need to be treated to resolution prior to considering a fit.13-19 The ability of the patient or family to comply with care, hygiene, handling and return visits, requires special consideration prior to embarking on any overnight wear of a contact lens.
None of the currently FDA-approved designs have an age restriction. None of the designs approved in the United States possess an indication for myopia control. Outside the United States, the Bloom lens (Menicon) carries this indication.20 Both adult and pediatric patients who have never worn a lens before may adapt faster than previous soft lens wearers who may be inclined to compare ortho-K designs with their habitual soft lenses.
Patients who have reduced their wearing time due to dryness or discomfort as well as those who wish to temporarily reduce their myopia make great candidates. If the intent is to slow myopia progression, then the earlier you identify onset and progression of myopia, the earlier you can intervene. Research has found a more rapid progression of their myopia in the year prior to onset and a slower rate after onset in children between six and 14 years old.21
Evidence for Efficacy
The Blue Mountains Eye Study from Australia found myopic maculopathy increases with the amount of myopia, with 43% of cases occurring in myopes less than 5.00D.22 This has led to the often-quoted statement that there is “no safe amount of myopia.”23 Any amount of myopia reduction is important, with a 40% decrease in risk of maculopathy for each 1.00D reduction in progression.24
Clinicians must monitor axial length changes to accurately track progression since orthokeratology reshapes the corneal surface. The corneal epithelium under the treatment zone thins while the midperipheral area in the reverse curves thickens to create the effect.25 A change in axial length of 0.1mm roughly equates to 0.20D to 0.25D.1
Comparisons of the safety and efficacy of ortho-K across studies is difficult because of variations in inclusion criteria, presence/absence of controls, lack of masking and methodological differences. Nonetheless, a summary of four representative meta-analyses reported remarkably consistent reductions in the progression of axial length in the range of -0.25mm to -0.27mm (Table 2).1,12,26-29
Table 2. Representative Summary of Effects of Ortho-K | ||||
| Author | Design | Duration (Years) | Sample size (N) | Reduction in Axial length (mm) |
| Cho and Cheung (2012) | RCT | 2 | 78 | -0.36±0.24 |
| Li et al. (2016) | Meta | 2 | 667 | -0.27 |
| Hiraoka et al. (2012) | RCT | 5 | 43 | -0.42 |
| Santodomingo-Rubido et al. (2017) | RCT | 7 | 14 | -0.13 |
Evidence for Safety
The risks associated with ortho-K are less well understood but are likely similar to those of other designs. Risk factors include overnight wear, use of tap water, and topping off solutions.12,26 The majority of published reports come from Asia and ortho-K is more widely used, where conditions of sanitation may vary, and suggest causative organisms encountered are overwhelmingly Pseudomonas aeruginosa or Acanthamoeba.17,30-32
Incidence data on rates of microbial keratitis are elusive but may be similar to overnight soft lens wear—between 19.5 to 25.4 per 10,000 wearers.12 Adverse events (corneal infiltrative events, including infection) in soft lenses appears to be comparable to adults and may be less in the eight- to 11-year-old age range.33 It is not clear whether this is true of ortho-K. In a retrospective study of gas permeable (GP) lens wearers who experienced Acanthamoeba keratitis, 24% wore ortho-K lenses but no odds ratio could be calculated.30 Research also shows that Pseudomonas aeruginosa binding to the corneal epithelium increases after overnight ortho-K wear.34
Initial Examination
The initial exam deviates only slightly from your usual standard routine for a contact lens wearer. There are a few additional tests that are important to facilitate the fit and track individual success, such as cycloplegic refraction, axial length, topography or tomography, pupil size and corneal diameter measurements.35 Many devices are capable of collecting this information, including a number of combination instruments. These contemporary devices can easily upload data to your lab to further assist in fitting. Be consistent when using these devices for each visit because agreement varies significantly between instruments.36,37
Cycloplegic refraction decreases the likelihood of over-minusing the patient. Some consider this an optional step, but, since a baseline fundus evaluation is important, it can be easily incorporated into the first visit. Tracking changes in axial length over time is a more reliable measure than changes in refractive error that are influenced by the reshaping of the corneal surface. Assessing pupil size in both ambient and low light conditions helps ensure the treatment zone of the lens will be optimized to reduce risks of flare or glare. Assessing corneal diameter ensures the overall diameter of the lens will not exceed that of the cornea and improve lens centration.
Tomography, such as the Pentacam (Oculus), relies on a rotating Scheimpflug camera and not a reflection of a Placido disc. It is not subject to errors induced by an unstable tear film and measures true corneal height as well as elevation data.38
Table 3. Summary of Different Fitting Approaches40 | ||
| Method | Advantage | Disadvantage |
| Empirical | Easy, no inventory; Good initial success | Dependent on consultation to refine the fit |
| Diagnostic and trial lenses | Patient gets to experience lens; Can modify fit in real time; Practitioner control | Requires more skill and experience |
| Software | Precision fitting; Higher initial lens success; customizable for unique cases | Relies on high-quality imaging of topography |
| Nomogram | Good first lens fit; Decreased chair time; Shortens learning curve | Requires diagnostic skill |
Placido disc topographers generally do not cover as large a region of the cornea as a tomographer, but there are some devices that allow you to stitch or tile together images from different fields of gaze to cover a larger surface area, such as the Medmont E300 (Medmont). This can be important when evaluating whether corneal astigmatism is confined to the central cornea or extends out toward the limbus, improving parameter and design selection. The two types of devices may offer the ability to model contact lens fits without putting a lens on the eye and may even generate simulated fluorescein patterns from the height data.
The ability to create subtractive or comparative maps is an essential feature on both devices. Topographical findings that make ortho-K more challenging include irregular astigmatism, high astigmatism, limbus-to-limbus astigmatism, decentered corneal apex and asymmetries.39 Topographical attributes that are positive indicators include well-centered apex near the geometrical center of the cornea, K values between 41.00D and 45.00D, with-the-rule astigmatism <1.50D and average corneal eccentricity between 0.25 and 0.80.39 Axial maps are useful for comparing patients while obtaining a general overview, tangential maps provide more data on localized shape changes induced by ortho-K, and difference maps will allow you to track changes (Figure 1).39
 |
|
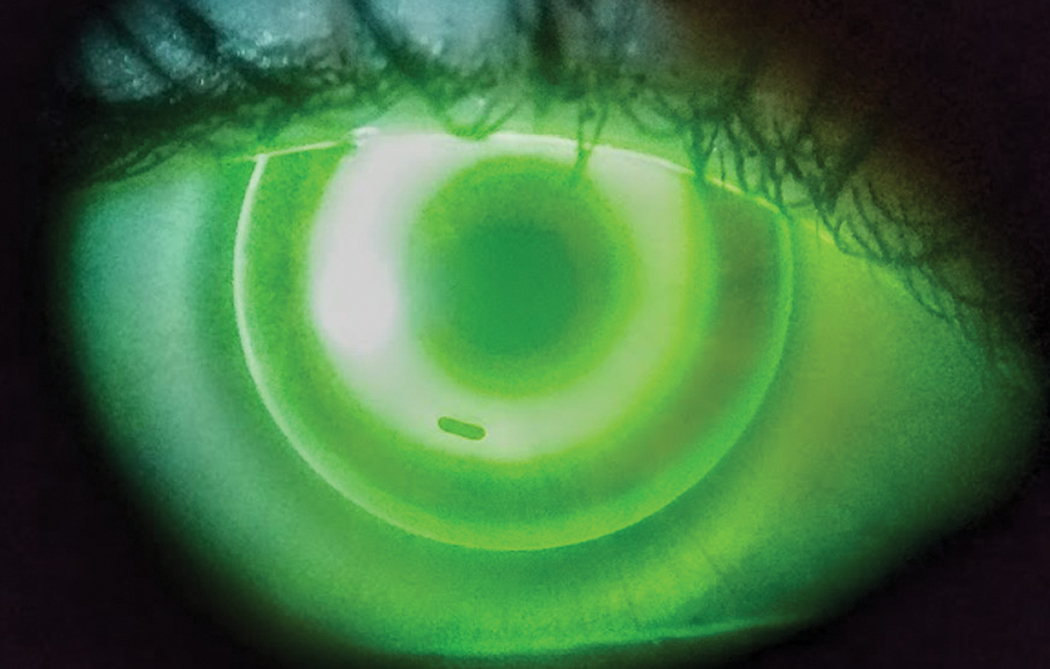
Fig. 2. In this well-centered ortho-K lens at the initial visit, note the small bubble under the return zone inferiorly. These can be ignored and will generally dissipate as the reshaping occurs in the first 24-hour period. You could also instruct the patient to overfill the lens with a viscous artificial tear prior to insertion. Click image to enlarge. |
Fitting
The data you collect helps determine whether to select a diagnostic trial lens, employ a fitting nomogram, submit electronically to the lab or to empirically design the lens using software.35 All are viable options (Table 3).40 As you gain more experience, you will likely want more control of the design process and may wish to use design software. Avoid using design software until you gain the deeper understanding of how to manipulate parameters to achieve a desired effect. Trial lenses can expedite the fitting process for anxious parents/patients, where empirically designed lenses can be more customized to topographical features.
You want a well-centered lens, with an aligned area of approximately 4mm in the treatment zone, pooling in the return zone where the reverse curves are 1mm to 2mm wide, then an alignment zone of similar width and finally enough edge lift to create a band of pooling of 0.5mm and ensure adequate tear exchange. The lens should move on the blink but not to the point it moves outside the corneal diameter (Figure 2).35
Once the amount of flattening for the myopia + Jessen factor have been incorporated into the base curve, you will seldom need to modify this parameter unless you determine undertreatment. In that case, you may flatten the base curve or increase the diameter of the treatment zone. More commonly, you will find you may need to modify the reverse curve, or the toricity of the reverse or alignment curves. The reverse curve contributes to decreasing the myopia slightly as you flatten this curve, thereby reducing the sagittal depth and eliminating a central island identified by topography. But mostly the reverse curve improves lens centration by manipulating the sagittal depth of the lens.
A low riding lens leaves a “frowny face” on your topography, and a high riding lens creates a “smiley face.” Modify the reverse curves and/or alignment curves by increasing or decreasing the sagittal depth, respectively. Smaller adjustments may be made by changing the landing zone angle on some lenses. In cases of corneal astigmatism that is limbus-to-limbus, these curves may need to be toric rather than spherical.35
Ortho-K for hyperopia and presbyopia (monovision) is an option; however, it’s not as well studied as it is for myopia. Nonetheless, studies with GP designs with base curve radii fit 0.4mm to 0.7mm steeper than flat K have shown success and reversibility with up to 28 hours of wear.40 The designs also have an impact on steepening of the treatment zone, flattening in the reverse zone and a positive shift in spherical aberration (as well as other HOAs).40-43
Follow-up Scheduling
The timing of return visits after dispensing are dictated by the individual needs of the patient. A typical schedule would be the morning after the first overnight wear period, one week and then one, three and six months.8 Once the desired effect is achieved, six-month intervals are fine. Assess the centration by topography and unaided visual acuities at every visit along with the ocular health, compliance and reinforce education. At one week, you will add a manifest refraction and you should be at or near your target of +0.50D to +0.75D of hyperopia.37 At six months, include axial length measurements to assess progression.
Continue educating yourself and consider adding this valuable service to your practice. Understanding myopic progression and control should become part of every primary care practice. There are numerous opportunities to acquire the proper training on ortho-K through continuing education programs at major meetings, dedicated societies and manufacturer online certification courses.
Adding ortho-K to your practice is a win for both patients and the economic health of your practice. It is immensely satisfying to change lives and reduce the risk of future morbidities through early intervention. You will also see how highlighting this service will benefit your practices.
Dr. Fuller is a professor and founding supervisor of the Cornea & Contact Lens–Refractive Surgery residency at The Eye Center at Southern College of Optometry. He is also a Diplomate of Cornea, Contact Lenses and Refractive Technologies for the American Academy of Optometry.
1. Bullimore MA, Richdale K. Myopia control 2020: Where are we and where are we heading? Ophthalmic Physiol Opt. 2020;40(3):254-70. 2. Li FF, Yam JC. Low-voncentration atropine eye drops for myopia progression. Asia Pac J Ophthalmol (Phila). 2019;8(5):360-5. 3. Walline JJ, Lindsley KB, Vedula SS, et al. Interventions to slow progression of myopia in children. Cochrane Database Syst Rev. 2020;1(1):CD004916. 4. Lam CSY, Tang WC, Tse DYY, et al. Defocus incorporated multiple segments (DIMS) spectacle lenses slow myopia progression: a two-year randomised clinical trial. Br J Ophthalmol. 2020;104(3):363-8. 5. Bennett T. New myopia-control eyeglasses for children show positive outcomes. Prim Care Optom News. 2020;25:5. 6. Bennett T. SightGlass targets global myopia progression with new spectacles. Prim Care Optom News. www.healio.com/news/optometry/20200709/sightglass-targets-global-myopia-progression-with-new-spectacles. July 9, 2020. Accessed October 21, 2020. 7. White P, Cho P. Legal issues in contact lens practice with special reference to the practice of orthokeratology. Ophthalmic Physiol Opt. 2003;23(2):151-61. 8. Cho P, Cheung SW, Mountford J, White P. Good clinical practice in orthokeratology. Cont Lens Anterior Eye. 2008;31(1):17-28. 9. Nichols JJ, Starcher L. Contact lenses 2019. CL Spectrum. 2020;35:18-25. 10. Morgan PB, Efron N, Woods CA, Santodomingo-Rubido J. International survey of orthokeratology contact lens fitting. Cont Lens Anterior Eye. 2019;42(4):450-4. 11. FDA. Types of contact lenses. www.fda.gov/medical-devices/contact-lenses/types-contact-lenses. January 16, 2018. Accessed October 21, 2020. 12. Bullimore MA, Johnson LA. Overnight orthokeratology. Cont Lens Anterior Eye. 2020;43(4):322-32. 13. Polse KA, Brand RJ, Keener RJ, Schwalbe JS. The Berekeley Orthokeratology Study, part III: safety. Am J Optom Physiol Opt. 1983;60(4):321-8. 14. Jun J, Zhiwen B, Feifu W, et al. Level of compliance in orthokeratology. Eye Contact Lens. 2018;44(5):330-4. 15. Robertson DM, Cavanagh HD. Non-compliance with contact lens wear and care practices: a comparative analysis. Optom Vis Sci. 2011;88(12):1402-8. 16. Szczotka-Flynn LB, Pearlman E, Ghannoum M. Microbial contamination of contact lenses, lens care solutions, and their accessories: A literature review. Eye Contact Lens. 2010;36(2):116-29. 17. Van Meter WS, Musch DC, Jacobs DS, et al. Safety of overnight orthokeratology for myopia: a report by the American Academy of Ophthalmology. Ophthalmology. 2008;115(12):2301-13. 18. Wang J, Liu L, Boost M, et al. Risk factors associated with contamination of orthokeratology lens cases. Cont Lens Anterior Eye. 2020;43(2):178-84. 19. Bui TH, Cavanagh HD, Robertson DM. Patient compliance during contact lens wear: perceptions, awareness and behavior. Eye Contact Lens. 2010;36(6):334-9. 20. Menicon. Menicon announces the launch of menicon bloom myopia control management system. www.menicon.com/corporate/news/view/47. May 24, 2019. Accessed October 21, 2020. 21. Mutti DO, Hayes JR, Mitchell GL, et al. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Investig Ophthalmol Vis Sci. 2007;48(6):2510-9. 22. Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31(6):622-60. 23. Fricke TR, Jong M, Naidoo KS, et al. Global prevalence of visual impairment associated with myopic macular degeneration and temporal trends from 2000 through 2050: systematic review, meta-analysis and modelling. Br J Ophthalmol. 2018;102(7):855-62. 24. Bullimore MA, Brennan NA. Myopia control: why each diopter matters. Optom Vis Sci. 2019;96(6):463-5. 25. Swarbrick HA. Orthokeratology review and update. Clin Exp Optom. 2006;89(3):124-43. 26. Cho P, Cheung SW. Retardation of Myopia in Orthokeratology (ROMIO) Study: a two-year randomized clinical trial. Invest Opthalmol Vis Sci. 2012;53:7077. 27. Li SM, Kang MT, Wu SS, et al. Efficacy, safety and acceptability of orthokeratology on slowing axial elongation in myopic children by meta-analysis. PLoS One. 2016;41(5):600-8. 28. Hiraoka T, Kakita T, Okamoto F, et al. Long-term effect of overnight orthokeratology on axial length elongation in childhood myopia: a five-year follow-up study. Invest Opthalmol Vis Sci. 2012;53:3913. 29. Santodomingo-Rubido J, Villa-Collar C, Gilmartin B, et al. Long-term efficacy of orthokeratology contact lens wear in controlling the progression of childhood myopia. Curr Eye Res. 2017;42:713-20. 30. Cope JR, Collier SA, Schein OD, et al. Acanthamoeba keratitis among rigid gas permeable contact lens wearers in the United States, 2005 through 2011. Ophthalmology. 2016;123(7):1435-41. 31. Watt KG, Swarbrick HA. Trends in microbial keratitis associated with orthokeratology. Eye Contact Lens. 2007;33(6 pt 2):373-7. 32. Watt K, Swarbrick HA. Microbial keratitis in overnight orthokeratology: review of the first 50 cases. Eye Contact Lens. 2005;31(5):201-8. 33. Bullimore MA. The safety of soft contact lenses in children. Optom Vis Sci. 2017;94(6):638-46. 34. Ladage PM, Yamamoto N, Robertson DM, et al. Pseudomonas aeruginosa corneal binding after 24-hour orthokeratology lens wear. Eye Contact Lens. 2004;30(3):173-8. 35. Lipson MJ. Initial fitting. In: Lipson MJ, ed. Contemporary Orthokeratology. Vol First. Rochester: Bausch Health; 2019:25-38. 36. Kumar M, Shetty R, Jayadev C, et al. Repeatability and agreement of five imaging systems for measuring anterior segment parameters in healthy eyes. Indian J Ophthalmol. 2017;65(4):288-94. 37. Penna RR, de Sanctis U, Catalano M, et al. Placido disk-based topography versus high-resolution rotating Scheimpflug camera for corneal power measurements in keratoconic and post-LASIK eyes: reliability and agreement. Int J Ophthalmol. 2017;10(3):453-60. 38. Mejía-Barbosa Y, Malacara-Hernández D. A review of methods for measuring. Optom Vis Sci. 2001;78:240-53. 39. Kojima R. Topography. In: Lipson M, ed. Comtemporary Orthokeratology. Vol First. Rochester: Bausch Health; 2019:39-53. 40. Lipson MJ, Brooks MM, Koffler BH. The role of orthokeratology in myopia control: a review. Eye Contact Lens. 2018;44(4):224-30. 41. Charm J, Cho P. High myopia-partial reduction orthokeratology (HM-PRO): study design. Cont Lens Anterior Eye. 2013;36(4):164-70. 42. Lu F, Sorbara L, Simpson T, Fonn D. Corneal shape and optical performance after one night of corneal refractive therapy for hyperopia. Optom Vis Sci. 2007;84:357-364. 43. Swarbrick HA, Hiew R, Key AI, Peterson S, Tahhan N. Apical clearance rigid contact lenses induce corneal steepening. Optom Vis Sci. 2004;81:427-35. 1. |

