 I feel comfortable treating most glaucoma, but when a patient’s compliance is questionable or the field defects seem to fluctuate over time, I get a bit nervous. When should I “say uncle” and send these patients for a second opinion?
I feel comfortable treating most glaucoma, but when a patient’s compliance is questionable or the field defects seem to fluctuate over time, I get a bit nervous. When should I “say uncle” and send these patients for a second opinion?
First, relax and have confidence in yourself and your care. “Remember that glaucoma is a slowly progressing disease, so there’s rarely such a thing as a glaucoma emergency,” says Robert Vandervort, OD, director of ocular disease services for Heartland Eye Consultants, in Omaha. Be sure to confirm any progression with a series of visual fields or OCT scans.
That said, it’s smart to “say uncle” when:
• You’re outside of your comfort zone. “Every optometrist and ophthalmologist has their own comfort level for treating and managing glaucoma,” Dr. Vandervort says. “If you’re at all uneasy about how your patient is doing, then absolutely get input.”
That doesn’t necessarily mean: when in doubt, refer it out. Because it usually progresses slowly, “glaucoma is a disease that really works well for collaboration,” he says. A phone call for a second opinion or advice on target IOP might be all you need.
 |
|
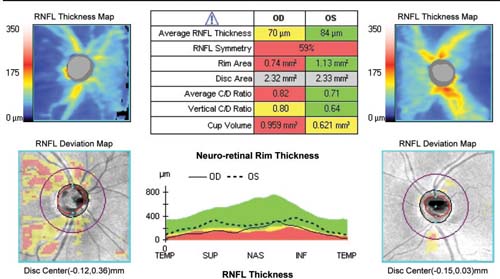
OCT may show glaucomatous damage earlier in the disease process than visual fields.
|
Signs of progression include the development of optic nerve disc hemorrhages or any noticeable changes in visual field, OCT, stereo fundus photos or optic nerve head appearance.
“Recent studies have shown that OCT is more likely than visual fields to pick up glaucomatous damage earlier in the disease process,” Dr. Vandervort says.1 “So, by the time you start picking up visual field loss, you probably have already seen significant damage of the optic nerve.” If OCT shows definite progression regardless of visual field loss, get a second opinion, he says.
Another concerning sign: high variability of IOP with or without optic nerve progression damage.2 “If a patient’s IOP is fluctuating from visit to visit by 10mm Hg—or even 6mm Hg to 8mm Hg—on medication, even without progression, I would get additional input,” he says.
• The patient is not compliant. “We know that when you add a second or a third IOP-lowering medicine, the patient’s compliance goes down,” Dr. Vandervort says. “And those second-line meds are at BID and TID dosing. So, now you’ve got not only another medicine but more drops per day. The chance that the patient is going to miss one of those drops goes up significantly.”
Instead of adding more drops, send the patient directly for selective laser trabeculoplasty. “I go to SLT very early on if there’s any question whatsoever about the control of the patient,” he says.
Last but not least, don’t let glaucoma patients get lost to follow up. “If patients fail to show up, you need to make an effort in writing to get them back in—and good documentation if they refuse to come back in,” Dr. Vandervort says.
In short, “if you’re going to manage glaucoma, you need a good recall system. If you’re not managing a tight protocol for recall, then you need to be thinking about sending these people out for opinions a lot faster,” he says.
1. Lisboa R, Leite MT, Zangwill LM, et al. Diagnosing preperimetric glaucoma with spectral domain optical coherence tomography. Ophthalmology. 2012 Nov;119(11):2261-9.
2. Rao HL, Addepalli UK, Jonnadula GB, et al. Relationship between intraocular pressure and rate of visual field progression in treated glaucoma. J Glaucoma. 2013; 22(9):719-24.

