A 54-year-old black male presented with a history as a glaucoma suspect. His previous eye-care provider had monitored him as a suspect every six to nine months for five years. His family history is positive for open-angle glaucoma in his mother and a maternal aunt.

The patient said he had never used any glaucoma medications, but added that his previous doctor cautioned that he might require them in the future. On further questioning, he said that the other doctor was concerned about the appearance of his optic nerves, but felt there was not enough evidence to warrant medical intervention.
His only current medication is Betapace (sotalol, Berlex) for atrial fibrillation. He reported no known allergies to medications.
Diagnostic Data
On initial presentation, best-corrected visual acuity was 20/20 O.D. and 20/25- O.S. Manifest refraction of -2.25 -1.75 x 100 O.D. and -4.74 -3.00 x 065 O.S. did not improve acuity. Pupils were equal, round, and reactive to light and accommodation with no afferent pupillary defect. Extraocular motilities were full in all diagnostic positions of gaze.
IOP measured 18mm Hg O.D. and 19mm Hg O.S. Central corneal thickness (CCT) measured 519m O.D. and 507m O.S. A slit lamp examination of the anterior segments was unremarkable. Gonioscopy demonstrated grade IV open angles to the ciliary body, with a moderate amount of trabecular pigmentation that was symmetric between the eyes. Threshold visual fields were normal O.U.
Through dilated pupils, the crystalline lenses were clear. There was a posterior vitreous separation in the left eye. Close examination of the optic nerves showed cup-to-disc ratios of 0.60 x 0.70 O.D. and 0.70 x 0.80 O.S. The nerve heads were normal in size. The cups appeared vertically elongated, and the neuroretinal rims were thinnest at 6 and 12 oclock in both nerves. Analysis of the nerve fibers demonstrated no discernable NFL thinning in either eye. Both maculae were healthy, although foveal reflex was absent in the left eye. Examination of the peripheral retina demonstrated scattered areas of pigmented cystoid O.U. I did not intervene medically at this point.
We obtained his records, which showed normal visual fields during the period the previous doctor evaluated him. IOP averaged 17mm Hg O.D. and 19mm Hg O.S., although there were some instances when IOP went as high as 23mm Hg O.D. and 24mm Hg O.S. Cup-to-disc ratios were previously judged to be 0.70 O.D. and O.S.
The patient returned to me eight weeks after the initial presentation for repeat tensions and field studies. At this visit, IOP measured 19mm Hg O.U. Repeat threshold fields were normal, and reliability indices were high.
Discussion
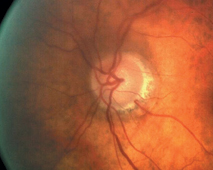
Although the patient is normotensive and does not have any field defects, his left eye shows classic glaucomatous optic neuropathy with neuroretinal rim loss and compromise.
At this point, we traditionally would consider two options: medicate the patient or continue to monitor him without intervention. Now, in light of recent literature, and given his risk factors and the appearance of his optic nerves, I chose to medicate this patient with Travatan (travoprost, Alcon) 1 drop O.U. hs (at bedtime).
Since the Ocular Hypertension Treatment Study, or OHTS, highlighted the role of CCT in ocular hypertensives, we have expanded our list of risk factors beyond race and IOP. However, two recently published studies speak to the heart of the clinical decision-making process in this particular case.
Researchers recently looked at the essential question this case posed: Is CCT a risk factor for visual field loss in normotensive patients who have glaucomatous optic neuropathy but normal visual fields?1 These researchers concluded that thinner central corneas, higher baseline IOPs and larger vertical cup-to-disc ratios could predict the development of visual field defects in these patients.
In their analysis, the mean CCT of patients who developed visual field loss during the term of the study (approximately 4.5 years) was 543m, while the mean CCT of those who did not develop field loss was 565m. These researchers also studied other risk factorsthese included refraction, age, gender family history of glaucoma, hypertension, cardiovascular disease and migraineand found that they were not predictive of field loss.
Also bearing on this case is another study that confirms that blacks generally tend to have thinner corneas than whites, Asians and Hispanics.2 Mean CCT in the black patients studied was 535m, while mean CCT in Asians, Hispanics and whites was 550m, with no significant intra-group difference among these three races. Also of interest: This study found a correlation between corneal curvature and CCT.
It is well documented that thinner corneas often lead Goldmann applanation tonometers to underestimate actual IOP. Experts have presented various formulas to correct IOP based on CCT readings, but because blacks tend to have thinner corneas, the potential exists for delayed diagnosis of glaucoma in this population, and increased severity of glaucomatous optic nerve disease at the time of diagnosis.
In this case, our patients preperimetric glaucomatous optic neuropathy, his thinner CCT readings, his family history and race warranted prompt intervention. As always, though, one must make a careful and methodical analysis of the entire glaucomatous landscape before rendering appropriate therapy.
1. Medeiros FA, Sample PA, Zangwill LM, et al. Corneal thickness as a risk factor for visual field loss in patients with preperimetric glaucomatous optic neuropathy. Am J Ophthalmol 2003 Nov;136(5):805-13.
2. Shimmyo M, Ross AJ, Moy A, Mostafavi R. Intraocular pressure, Goldmann applanation tension, corneal thickness, and corneal curvature in Caucasians, Asians, Hispanics, and African Americans. Am J Ophthalmol 2003 Oct;136(4):603-13.

