 |
He has maintained good follow-up over the past eight years and comes in regularly for visual field tests, intraocular pressure (IOP) checks and nerve imaging.
Diagnostic Data
When the patient initially presented in 1997, his IOPs averaged 15-16mm Hg O.U. on Xalatan and Timoptic. (His pre-treatment IOPs had been in the upper 20s O.U.)
Cup-to-disc ratios were 0.50 x 0.70 O.D. and 0.50 x 0.75 O.S. Threshold field studies demonstrated superior incomplete arcuate scotomas O.D. and O.S. Review of his past records indicated nothing out of the ordinary, and he was deemed medically stable.
Over the next few years, the only change I made to his ophthalmic medication was to decrease the Timoptic 0.5% from b.i.d. to q.a.m.
At the patients most recent visit, his systemic medications were Proscar (finasteride, Merck), Vytorin (ezetimibe/simvastatin, Merck/Schering-Plough), Plavix (clopidogrel, Bristol-Myers Squibb/Sanofi Pharmaceuticals), metoprolol and 81mg aspirin. He has no allergies to medications.
Best-corrected visual acuities at this visit were 20/25 O.D. and 20/30- O.S. through minimal hyperopic astigmatic correction. Pupils were equal, round and reactive to light and accommodation with no afferent papillary defect. A slit lamp examination of the anterior segment was unremarkable. The patient was pseudophakic, having undergone cataract surgery about 10 years earlier. Gonioscopic examination of the anterior chamber angles demonstrated wide open, grade IV pseudophakic angles with minimal trabecular pigmentation O.U.
Applanation tensions were 10mm Hg O.D. and 11mm Hg O.S. In fact, over the past three visits (approximately nine months), IOPs have averaged about 10mm Hg O.D. and O.S. All prior visits showed IOPs to average 15mm Hg in both eyes.
Through dilated pupils, the posterior chamber IOLs were centered in the capsular bags, and the posterior capsules were clear and intact. There were multiple vitreous floaters O.U. Stereoscopic examination demonstrated optic nerves of normal size, with vertical elongation of the cup-to-disc ratio to 0.50 x 0.75 O.U. The inferior rims were thinnest; therefore the ISNT rule (inferior-superior-nasal-temporal) did not apply. Visual fields demonstrated no progression in the arcuate defects. Optic nerve imaging also demonstrated no change in the optic nerve characteristics. Both maculae were characterized by dry retinal pigment epithelial mottling, O.S. > O.D., consistent with this patients best-corrected acuity and with previous visits.
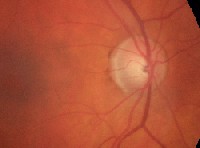 |
| Image of right optic nerve. Note the thinned neuroretinal rim inferiorly. The ISNT rule does not apply. |
Discussion
Because this patient has remained stableand even shown some improvementhe might be best served by reducing the frequency of visits to the office. Specifically, his IOPs are lower than ever before, and his optic nerves and visual fields have remained stable.
While there is nothing necessarily wrong with this reasoning, there have been some recent reports in the ophthalmic literature about the long-term effects of prosta- glandins (and topical carbonic anhydrase inhibitors) on IOP measurements.
Eye doctors now universally accept that corneal thickness plays a significant role in both IOP measurement and the risk of developing glaucoma. And, we now know that thinner pachymetry readings of central corneal thickness (CCT) cause us to read artificially low IOP (as measured by the Goldman applanation tonometer) and increase the risk of ocular hypertension converting to glaucoma.
Some recent reports in the literature suggest that long-term use of prostaglandin F2-alpha analogues may result in thinning of the cornea over time.1 This corneal thinning, in turn, may cause an underappreciation of true IOP. Researchers have proposed that long-term use of PGF2-alpha analogues may exhibit effects on the extracellular matrix of the corneal stroma via upregulation of matrix metalloproteinases (MMPs). While this mechanism has yet to be clinically proven, it does bring up the possibility that certain topical medications may play a role in thinning the cornea over time, with a concurrent underestimation of IOP levels.
As for our patient, his pachymetry readings on his last visit were 521m O.D. and 534m O.S. It would be interesting to know what his CCTs were when therapy with Xalatan was initiated, but that information is not available since pachymetry was not used at that timethe relationship between CCT and IOP was not readily considered in the mid-1990s.
In the interim, I plan on continuing to see this patient every three to four months, as I have done in the past. While he is clinically stable now, there are no guarantees that he will remain so. Does the reduced IOP give us a little breathing room? Perhaps, but constant vigilance is the standard in glaucoma patient care, no matter how good things look at the moment.
1. Viestenz A, Martus P, Schlotzer-Schrehardt U, et al. Impact of prostaglandin-F(2alpha)-analogues and carbonic anhydrase inhibitors on central corneal thicknessa cross-sectional study on 403 eyes. Klin Monatsbl Augenheilkd 2004 Sep;221(9):753-6.

