 |
A 26-year-old Caucasian male presented with a red, painful, light-sensitive left eye after accidentally being injured when a compressed air hose nozzle hit his eye. He was wearing no safety eyewear protection. His entering unaided visual acuities were 20/20 OD and 20/400 OS with no improvement to pinhole. Pupillary testing revealed a distorted, irregular “D-shaped” left pupil with the absence of an afferent pupillary defect. Applanation tonometry measured 18mm Hg OD and 19mm Hg OS.
Slit lamp examination demonstrated a mild nasal bulbar conjunctival abrasion with corresponding injection, grade 1+ traumatic iritis, moderately diffused central corneal edema, trace hyphema, and a sectoral disinsertion of the iris located inferior nasally from 8 o’clock to 10 o’clock with a corresponding transillumination defect (Figure 1).
Anterior segment findings in the right eye were unremarkable. Gonioscopy was deferred due to the presence of active inflammation and hyphema.
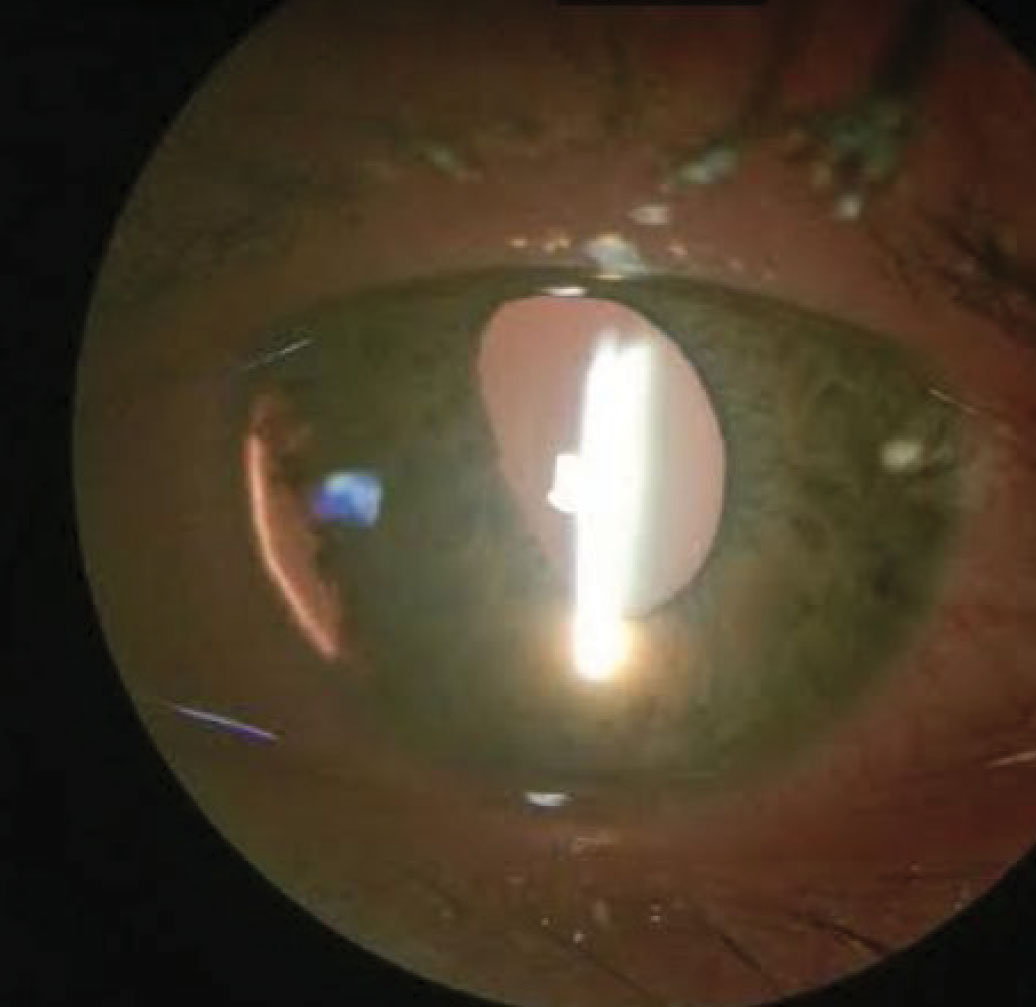 |
| Fig. 1. This photo shows our patient’s iridodialysis with accompanying inferior nasal transillumination defect. Click image to enlarge. |
Diagnosis
A fundus examination revealed mild vitreous hemorrhage, diffuse radial striae within the macular zone (Figure 2). We also noted multiple pre- and subretinal hemorrhages peripherally in the left eye. Otherwise, the retinas were flat and intact with no holes, breaks or tears. A B-scan high resolution ultrasonography was performed and revealed the presence of fluid in the left eye’s nasal suprachoroidal space (Figure 3). The test confirmed no signs of a retinal detachment.
Based on the clinical presentation and findings, the diagnosis of left large iridodialysis was made. The patient was prescribed topical cyclopentolate 1% BID, erythromycin topical ophthalmic 0.5 % ointment TID and Pred Forte (prednisolone acetate, Allergan) Q3H in the left eye until his follow-up in 24 hours. We advised he undergo a head elevation during sleep and begin topical lubricants for anterior surface irritation. The next day the patient exhibited significant improvement in ocular signs and symptoms. The conjunctival abrasion and iritis resolved, he showed improved corneal edema and a near-complete resolution of the hyphema.
Referrals were made to retina specialty for posterior segment evaluation and ophthalmology for possible surgery.
 |
| Fig. 2. This fundus image shows circular, radial striae concentrated within the macular aspect. Click image to enlarge. |
Discussion
Iridodialysis is the separation of the iris root from its ciliary body insertions, commonly sequela of blunt or penetrating ocular trauma.1-6 However, intraocular surgical procedures or congenital causes are possible.3 Occurrences are commonly unilaterally and sectoral, although complete dialysis of the iris have been reported.1 The detachment of the peripheral iris root, the thinnest attachment, results in the classic “D-shaped” pupil sign where the pupillary margin, opposite of the dissection, flattens.1
Cases of iridodialysis may present with pain, traumatic uveal inflammation and possible associated findings, such as conjunctival injection, subconjunctival hemorrhage, hyphema, corneal abrasion, decreased or increased intraocular pressure (IOP), angle recession, vitreous hemorrhage or retinal detachments.2,3 Photophobia and unilateral diplopia are possible symptoms secondary to polycoria at the corneal limbus from the abnormal anatomical pupil shape created by the iridodialysis.3,4
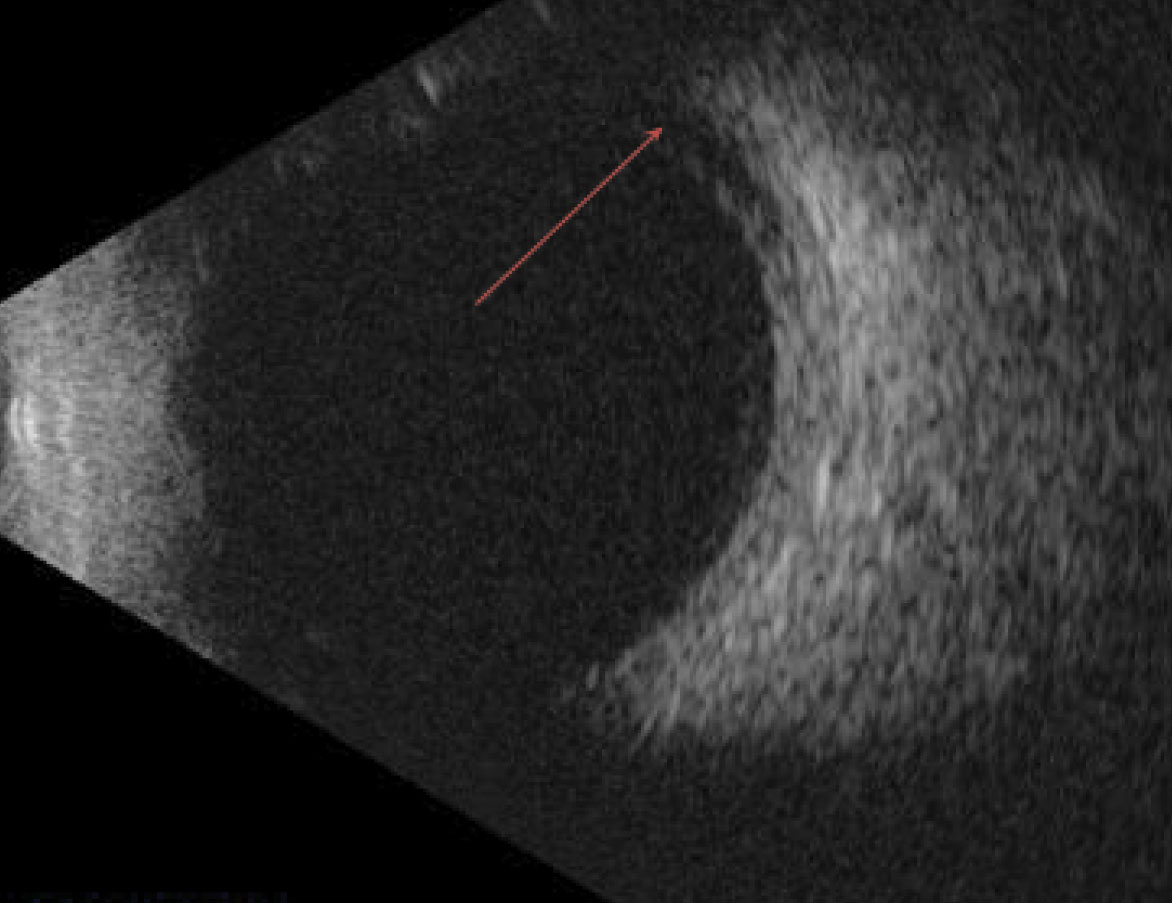 |
| Fig. 3. Fluid in the superchoroidal space was observed using B-scan imaging. Click image to enlarge. |
Treatment
Management depends on the size and location of the iridodialysis. Cosmesis is also a concern. Superior dialyses are often covered by the upper lid and may present with fewer concerns, whereas temporal or inferior iridodialyses are more symptomatic.1,2 Small, localized dialysis usually does not require treatment and may spontaneously resolve.2 Larger dialysis (less than 2 clock hours) requires a non-emergent referral for surgical intervention, commonly done by suture and sutureless techniques via limbal peritomy and multiple sclerostomies.1-6
Sutureless techniques are often reserved for simple iridodialysis repair in conjunction with other intraocular procedures.1,2 Associated collateral ocular trauma complications (e.g., corneal abrasion, elevated IOP, retinal detachment) must be addressed, treated and managed accordingly with topical ophthalmic preparations.2-7
Cycloplegics (anticholinergic drugs) are effective in alleviating pain by inhibiting ciliary body spasm, limiting the iris area to prevent the formation of a synechiae, and stabilizing the blood-aqueous barrier to reduce ocular inflammation.8 Topical corticosteroids and non-steroidal anti-inflammatory agents can reduce acute immune responses.6,7 Anti-glaucoma medications may be used to lower IOP in ocular hypertensive concurrent cases.6,7
Following the resolution of any accompanying inflammatory reactions, gonioscopy can rule out any trabecular meshwork damage or angle recession.6,7 Dialyzed angles with under 180˚ involvement have a lower risk for the development of secondary angle recession glaucoma.6,7 The prognosis of iridodialysis is good post-surgical therapy.2,6,7
The patient returned asymptomatic and was happy with the cosmetic outcomes at his three-month follow up post-surgical iris repair. Visual unaided acuities were 20/20 OD, 20/20 OS. His anterior and posterior segment findings were unremarkable with normotensive IOP in both eyes. Sequential follow ups at six months revealed stable findings with the patient remaining stable at each visit. Being stable, annual clinic visits were recommended for observation.
1. Romanazzi F, Morano A, Caccavale A. Diagnostic and therapeutic approach in a case of severe post-traumatic hyphema with subtotal iridodialysis. Case Rep Ophthalmol. 2017;8(3):496-502. 2. Loiudice P, Casini G. Post-traumatic iridodialysis, crystalline dislocation and vitreous haemorrhage: how to manage. BMJ Case Reports. 2014;2014:bcr2014205595. 3. Pandey S, Sharma V. Commentary: Modified sewing machine technique: An innovative method for the management of iridodialysis, iris coloboma, and scleral fixation of intraocular lenses. Indian J Ophthalmol. 2018;66(8):1177-8. 4. Ravi Kumar K. Modified sewing machine technique for iridodialysis repair, intraocular lens relocation, iris coloboma repair, Cionni ring fixation, and scleral-fixated intraocular lens. Indian J Ophthalmol. 2018;66(8):1169-76. 5. Richards J, Kennedy C. Sutureless technique for repair of traumatic iridodialysis. Ophthalmic Surg Lasers Imaging. 2006;37:508-10. 6. Sihota R, Kumar S, Gupta V, et al. Early predictors of traumatic glaucoma after closed globe injury: trabecular pigmentation, widened angle recess, and higher baseline intraocular pressure. Arch Ophthalmol. 2008;126(7):921-6. 7. Abri Aghdam K, Aghaei H, Shokrollahi S, et al. Comparison of the effect of cycloplegic versus NSAID eye drops on pain after photorefractive keratectomy. J Current Ophthalmol. 2015;27(3-4):87-91. 8. Ellong A, Ebana Mvogo C, Nyouma Moune E, et al. Post-traumatic glaucoma with irido-corneal angle injuries in Cameroon. Bull Soc Belge Ophtalmol. 2005;(298):21-8. |

