 |
History
A 67-year-old Black female reported to the office for a glaucoma follow-up. She explained that her eye pressure had been managed by another doctor, but—since that practice no longer took her insurance—she was referred to us by her internist.
Systemic history was remarkable for hypertension, managed with atenolol 50mg QD; ocular history was significant for open-angle glaucoma of one year’s duration, treated with latanoprost HS, OU. She denied exposure allergies of any kind.
|
|
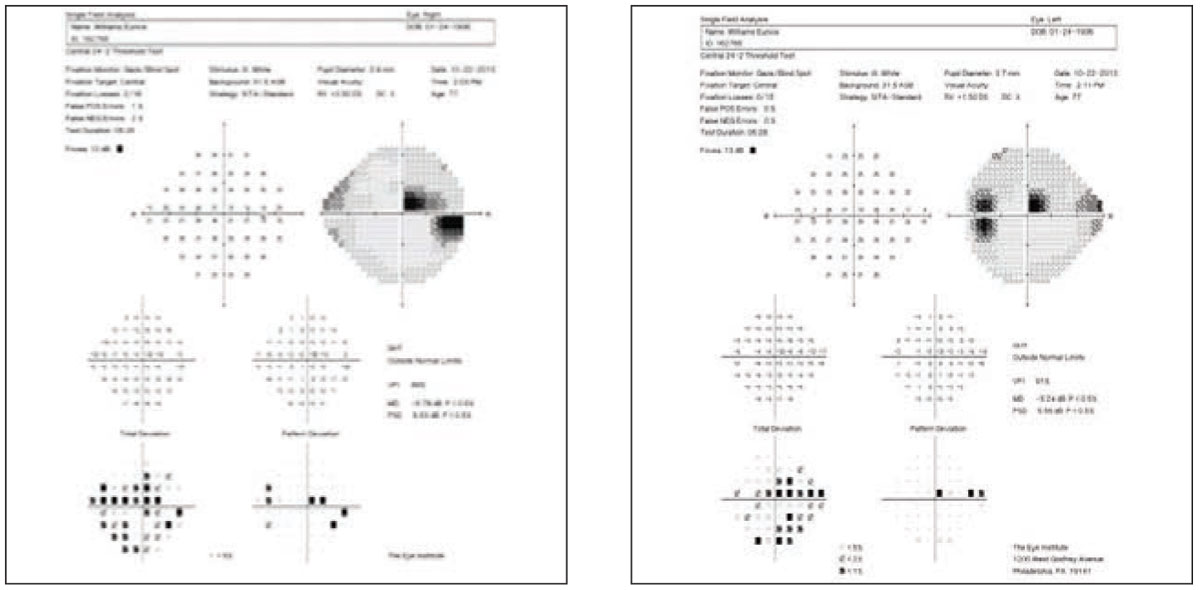
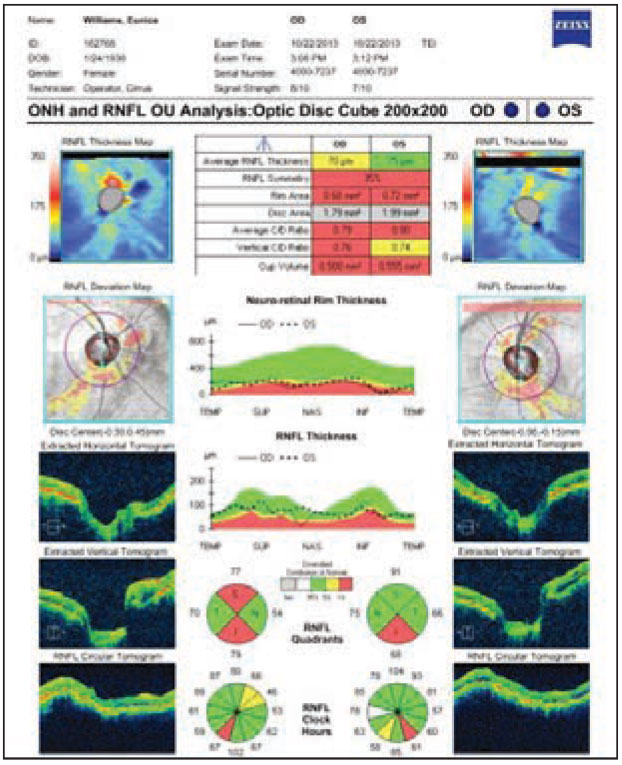
The homonymous field defect leads one to consider a differential diagnosis path that may or may not be supported by the exam findings and OCT results. Click images to enlarge. |
|
Diagnostic Data
Her best-corrected entering visual acuities were 20/20 OU at distance and near. Her external exam was normal with no evidence of afferent pupillary defect. The biomicroscopic exam of the anterior segment was normal with superficial evidence of open angles. Goldmann applanation tonometry measured 15mm Hg OU. The dilated fundus findings were normal peripherally and centrally with both nerves exhibiting moderately increased cup-to-disc ratios measuring 0.7/0.8 OU.
Additional studies included pachymetry (550µm OU), visual fields, OCT of the nerves, gonioscopy (D40r, no pigment, no exfoliation, no angle recession and no neovascularization) and a phone call to the old practice to attempt to obtain critical previous data.
Diagnosis
The diagnosis in this issue is left posterior occipital lobe infarct and glaucoma suspect, OU. Occlusion of the calcarine arteries with or without abnormalities in the branches of the middle cerebral arteries (MCA) has the potential to alter the vascular service to the occipital lobe tip.1-4 The occipital lobe tips receives neural projections from the foveomacular regions and is nourished by both the calcarine artery and a branch of MCA.1-4 Cases of central homonymous hemianopsia, respecting both the horizontal and vertical quadrantic boundaries, must be viewed with skepticism, considering the potential for cerebrovascular disease.1-4
In the case of this patient, while the potential of marginally high unmediated intraocular pressure (IOP) and increased cup-to-disc ratios suggested open-angle glaucoma triggering an appropriate structural and functional investigation, the congruous homonymous nature of the field loss mandated the need to rule out a non-glaucomatous source. In the setting of pre-existing vascular disease, fields with this specific characteristic must be approached as either being caused by cerebrovascular disease or concurrent disease (e.g., glaucoma and cerebrovascular issues). Diagnosing glaucoma exclusively must occur by exclusion.
Poor anastomosis between posterior cerebral artery (PCA) and MCA in the occipital tip is one postulated explanation for occurrence of the infarction of that area.1
Patient Status
The patient was continued on their topical drops for the purpose of maintaining pressures at the sub-18mm Hg level and the patient was referred to neuro-ophthalmology, where imaging confirmed the presence of left occipital lobe infarction. Old records were obtained to provide insight to unmedicated IOPs, disc appearance and other data, which might dictate whether topical pressure control should be continued or truncated.
Certainly, enlarged cup-to-disc ratios and nerve fiber layer dropout measured by the OCT correlating with visual field data could circumstantially suggest that the arcuate loss was produced by concurrent glaucomatous disease. At the time of publication, it was decided to maintain topical therapy with the idea that, in a patient with known vascular compromise, a lower IOP would permit less resistance to ocular perfusion, an advantage even to the healthy.
1. Kiriyama K, Yoshimura T, Furuya H, et. al. A case of central homonymous hemianopsia due to cerebral infarction of the occipital tip. Rinsho Shinkeigaku. 1996;36(7):902-5. 2. Schira MM, Tyler CW, Breakspear M, Spehar B. The foveal confluence in human visual cortex. J Neurosci. 2009;29(28):9050-8. 3. Keklikoglu HD, Yoldas TK, Coruh Y. A case report of bilateral superior altitudinal hemianopia with cerebral infarction. Neurologist. 2010;16(2):132-5. 4. Etgen T, Köhler M, Sander D. Bilateral superior altitudinal hemianopia: missing the goal, but hitting the stroke cause. J Stroke Cerebrovasc Dis. 2010;19(2):165-6. |

