A 63-year-old Native American male presented with severe eye pain, lacrimation, edema and erythema of the eyelids. Three days earlier, he attempted to evade police while driving under the influence of alcohol. The police sprayed him in the face with pepper spray at (less than two feet) while trying to subdue him.
The police let the patient rinse his eyes with water at the station. He continually rinsed his eyes throughout the weekend. On Monday, his symptoms did not subside, and he presented for treatment.
Ocular history was unremarkable. His medical history was positive for systemic hypertension and heart disease and gout, for which he took allopurinol, indomethacin, colchicines, benazapril and hydrochlorothiazide. Family history was positive for diabetes and hypertension. He reported no medical allergies.
Diagnostic Data
Uncorrected visual acuity was 20/200 O.D. and 20/100 O.S. The patient could not see through a pinhole with his right eye but saw 20/60+ with his left. Pupil testing was difficult, but he responded normally. I did not check IOP given his pain, blepharospasms and corneal injuries.
Anterior segment exam revealed erythema and localized irritation of the upper and lower eyelids, greater O.D. than O.S. The conjunctiva was chemotic and hyperemic.
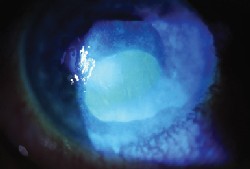
Two days after exposure to pepper spray, a large epithelial defect and dense corneal haze were present.
A large central epithelial defect with dense corneal haze was present in the right eye. The anterior chamber appeared quiet. The iris and lens were normal.
The left eye had moderate to severe diffuse corneal epithelial staining. The anterior chamber, iris and lens were normal.
Diagnosis
The patient had a large corneal epithelial defect O.D. with conjunctival and eyelid inflammation and reduced visual acuity. This was a result of the close-range exposure to pepper spray. His left eye was less involved and had moderate epithelial staining.
Treatment and Follow-up
I started the patient on ciprofloxacin qh O.U. while awake, tobramycin ointment O.U. at bedtime, and 5% homatropine bid O.U. for comfort. (I discontinued the homatropine after a week and told him to use artificial tears between instillation of antibiotics.)
I prescribed the antibiotics for prophylaxis because of the epithelial compromise and indications of poor hygiene habits, and the tobramycin ointment for nighttime protection and lubrication. The patient experienced less discomfort, and there was minimal reduction in vision with use of the ointments and artificial tears.
I had him return the next day, at which time there was less lid erythema and conjunctival hyperemia. The right cornea was re-epithelializing, but a large central area remained abraded. The left eye had moderate, diffuse epithelial staining extending from nasal to temporal limbus.
Two days after initiation of treatment, uncorrected visual acuity was 20/400 O.D. and 20/100 O.S., with pinhole acuity of 20/200 O.D. and 20/50 O.S. The patient reported less pain and burning. The lid and conjunctival inflammation were resolving, and the right corneal defect was 80% epithelialized.
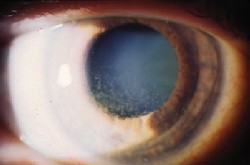
Five days after exposure to pepper spray, the right cornea was 80% epithelialized.
On day three, the patient said that he felt much better using the ointment twice a day as well as at night. Uncorrected visual acuity was 20/80+1 O.D. and 20/50-1 O.S., with pinhole acuity of 20/40-2 O.D. and 20/40+1 O.S. Slit lamp examination revealed grade 3 conjunctival injection O.D. and grade 2 O.S. There was no corneal staining in either eye. The epithelial defects resolved in both eyes, but there was persistent haze.
An associate prescribed TobraDex (tobramycin/dexamethasone, Alcon) ointment qid O.U. and artificial tears qid. He instructed the patient to discontinue the ciprofloxicin and to return in one week. We prescribed the TobraDex once the epithelial surface was healed in order to reduce the inflammatory response and resolve the haze. Again the antibiotic was included as a prophylactic measure.
The patient did not keep his appointment but returned a month later. He complied with the TobraDex regimen. Uncorrected visual acuity was now 20/30-1 O.D. and 20/40-1 O.S. IOP with non-contact tonometry measured 11mm Hg O.U. The eyelid inflammation had subsided, but there was slight stromal haze and trace fluorescein staining O.D. The mild staining appeared to be from dryness and possibly from overuse of the ointment. I instructed the patient to discontinue the TobraDex and continue using artificial tears.
Four months later, the patient returned complaining of headaches, burning, tearing and itching eyes. Corrected visual acuity was 20/30-2 O.D. and 20/20- O.S. Anterior segment exam was normal. I prescribed Patanol (olopatadine, Alcon) one drop bid in both eyes and Celluvisc in both eyes at bedtime.
The patient returned for a comprehensive eye exam six months after the incident. Best-corrected visual acuity was 20/20 O.U. Slit lamp exam was normal, and both corneas were clear, with no scarring or haze. IOP measured 12mm Hg O.U. Dilated fundus examination was normal.
Discussion
Pepper sprays are widely used by law enforcement as a form of nonlethal deterrent. Oleoresin capsicum, an extract of hot peppers, is the main ingredient, although the concentration varies by product.1,2 Capsaicin, the derivative of peppers (capsicum), causes intense pain when applied to the skin and the eyes, and neurogenic inflammation due to the release of neuropeptides contained in nerve terminals.3 It also induces an inflammation process that may be associated with endothelial cell death.
The extent of acute toxicity depends on the concentration of capsaicin and route
of administration.4 Considerable data indicates that pepper spray is safe, but little data exists on its effects on the human cornea.

Six months after exposure, both corneas were clear with no scarring or haze.
Isopropyl alcohol is often used as a carrier agent. The carrier is intended to evaporate between 1 and 2 meters, the recommended distance when using pepper spray. One study suggests that the alcohol itself is responsible for corneal injury.5
Researchers have found that the effects of pepper spray on ocular tissue include burning, redness, corneal epithelial defects and edema that last for months. One review of more than100 cases of pepper spray exposure identified seven patients with sustained corneal epithelial defects.6
Another study involving exposure to a less toxic water-based pepper spray found that the predominant symptoms were pain, reduced visual acuity, punctate epithelial erosions with no abrasions and reduced corneal sensitivity. One week later, subjects returned to normal.2
Finnish researchers sprayed pepper spray with isopropyl alcohol on 10 police officers at 1.5 to 2.5 meters. Symptoms included nasal congestion, facial hyperemia, and facial and ocular stinging. Clinical signs included reduced corneal sensitivity, focal epithelial cell damage, conjunctival hyperemia, mild chemosis, reduced visual acuity, increased tearing and temporary corneal epithelial swelling.
These researchers concluded that a single exposure to oleoresin capsicum is relatively harmless to the cornea and conjunctiva, but it may cause immediate changes that can last up to one week. Repeated exposure, however, could have long-lasting changes in corneal sensitivity.3
There have been documented cases of death due to pepper spray.7 Cough, gagging, inability to vocalize, and subjective shortness of breath have been observed in studies, suggesting risk of respiratory compromise from inhaled spray. Effects include laryngospasm, bronchoconstriction, and airway and pulmonary inflammation. Subjects sprayed by police are often agitated and may be intoxicated. They are also under constraints and under these conditions may develop respiratory distress.8
We treated five to 10 pepper spray injuries in a two-year period. Each patient had moderate to severe epithelial defects, and the complete healing process sometimes took one to two months. They were exposed to the spray at six inches to two feet, and the spray came into direct contact with corneal tissue.
These factors, plus the velocity of the spray, concentration of capsaicin and carrier chemicals may have caused the increased severity of the epithelial defects and the longer healing period. None of the patients experienced recurrent corneal erosions or lasting edema, but they did have reduced visual acuity, dryness and discomfort for weeks to months after exposure.
Patients who present with pepper spray injuries will most likely have washed their face and eyes with large amounts of water. After thorough irrigation of ocular tissues, examine the patient for epithelial defects. If corneal surfaces are compromised, prescribe a broad-spectrum antibiotic and copious amounts of lubricants.
When the corneal surface heals with no fluorescein staining, consider adding a topical steroid to resolve inflammation and corneal haze. To reduce lingering inflammation of ocular tissue, consider a topical NSAID as well. Use caution when prescribing a topical steroid because it may delay healing.
Visual acuity may not return to normal for weeks or perhaps months. There may be some loss of corneal sensitivity and potential for recurrent corneal erosion. With this in mind, the patient should be followed until the injury has completely resolved.
Dr. Greenlee formerly practiced on the Turtle Mountain Indian Reservation in Belcourt, N.D. He is now staff optometrist at the Veterans Affairs Medical Center in Lexington, Ky.
1. Reilly CA, Crouch DJ, Yost GS. Quantitative analysis of capsaicinoids in fresh peppers, oleoresin capsicum and pepper spray products. J Forensic Sci 2001 May;46(3):502-9.
2. Zollman TM, Bragg RM, Harrison DA. Clinical effects of oleoresin capsicum (pepper spray) on the human cornea and conjunctiva. Ophthalmology 2000 Dec;107(12):2186-9.
3. Vesaluoma M, Muller L, Gallar J, et al. Effects of oleoresin capsicum pepper spray on human corneal morphology and sensitivity. Invest Ophthalmol Vis Sci 2000 Jul;41(8):2138-47.
4. Richeux F, Cascante M, Ennamany R, et al. Implications of oxidative stress and inflammatory process in the cytotoxicity of capsaicin in human endothelial cells: lack of DNA strand breakage. Toxicology 2000 May 19;147(1):41-9.
5. Lee RJ, Yolton RL, Yolton DP, et al. Personal defense sprays: effects and management of exposure. J Am Optom Assoc 1996 Sep;67(9):548-60.
6. Brown L, Takeuchi D, Challoner K: Corneal abrasions associated with pepper spray exposure. Am J Emerg Med 2000 May;18(3):271-2.
7. Tsun J. Pepper spray just wont go away. N C Med J 2000 Sep-Oct;61(5):245-6.
8. Chan TC, Vilke GM, Clausen J, et al. The effect of oleoresin capsicum "pepper" spray inhalation on respiratory function. J Forensic Sci 2002 Mar;47(2):299-304.

