Trends and ControversiesCheck out the other feature articles in this month's issue:- Myopia: Should We Treat It Like a Disease? - How COVID-19 is Reshaping Optometry - Will Subspecialization Help Optometry Evolve? - Genetics in Eye Care: DNA Leads the Way - A Simpler Way to Code Office Encounters |
Technology has brought a steady stream of improvements to optometry in recent years, mostly in the form of improved diagnostic devices, but the bedrock principles of clinical care haven’t really changed. We still examine patients directly and make our assessments by synthesizing all relevant data in a mental calculus that draws upon our expertise, intellect and instincts. Two emerging tech trends—artificial intelligence (AI) and telehealth—hold the potential to revolutionize that. In fact, one already has.
The social distancing policies put in place this spring amid the COVID-19 pandemic included recommendations by the Centers for Disease Control and Prevention (CDC) to temporarily suspend all medical services other than urgent or emergent care.1 Suddenly, optometrists and their patients were isolated from each other. Telehealth solutions quickly emerged—in a sporadic, improvised way—to bridge the gap.
The CDC’s nationwide recommendation to postpone routine eye care is no longer in effect, but our continued need to maintain social distancing has introduced a challenge to the existing model of eye care. How can we protect our patients, our staff and ourselves as providers and still provide a high level of care without risking the spread of infection? Advances in telemedicine and telehealth, including the use of AI, may offer solutions.
This article reviews how some optometrists have used telehealth to evaluate patients as well as the options available to practitioners to provide remote ocular and visual health assessment, and how AI-enabled devices can shoulder some of the work of eye health assessment when doctors are inaccessible.
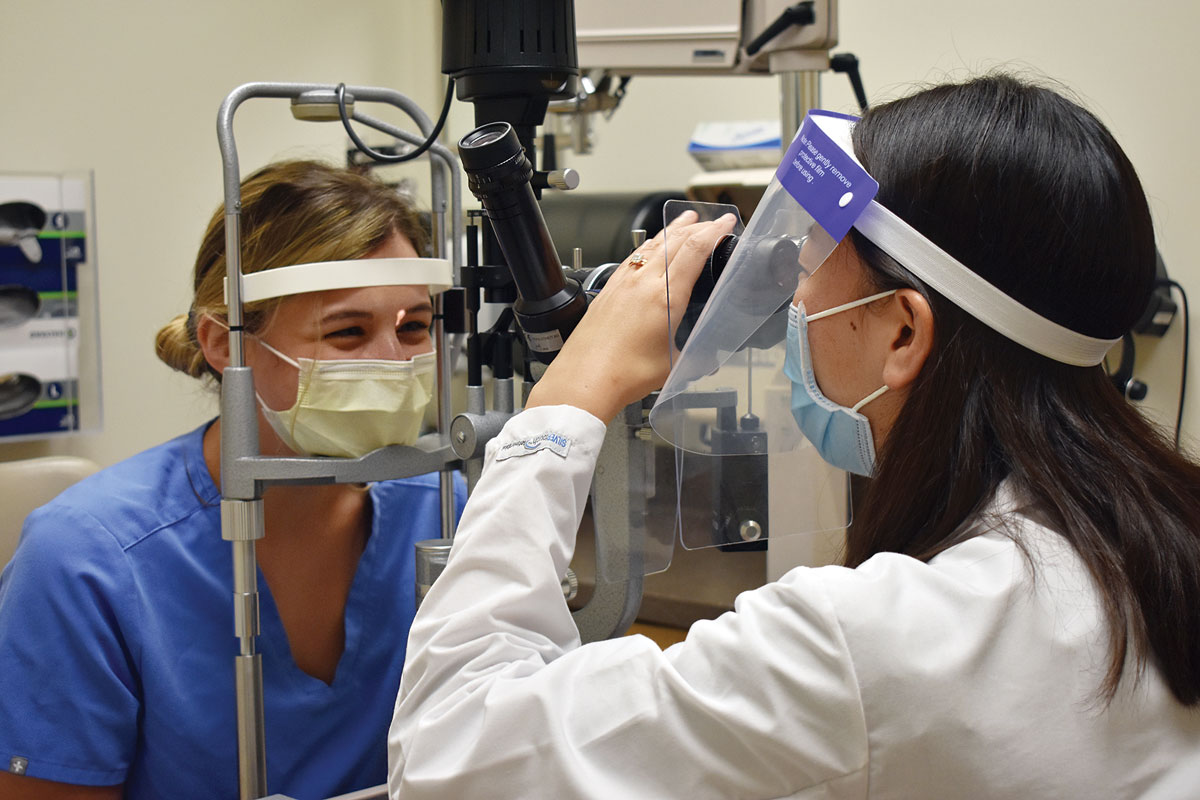 |
| Social distancing policies have affected safety protocols, motivating some doctors and patients to turn to telehealth. Click image to enlarge. |
Virtual Visits
Aspects of optometry can pair well with telemedicine. We have become increasingly reliant on imaging technology, such as optical coherence tomography (OCT) and advanced retinal imaging, to provide diagnostic capabilities above and beyond conventional slit lamp and binocular indirect ophthalmoscopy exam. Current telehealth imaging is significantly below the quality of our in-office professional tools, but it affords us an opportunity to observe the patient’s ocular anatomy in a limited way. Though it can’t replace the in-person doctor-patient relationship, telehealth is helping primary and specialty care providers find new ways to offer optometric services at home and expand the reach of care for those who may not currently be using ophthalmic services.
Current CDC recommendations advocate the use of telemedicine in place of live clinic visits, and it appears this recommendation has been well-received. Before COVID-19, less than 25% of patients were aware of telemedicine as a form of healthcare available to them. Since the pandemic, leading telehealth platforms report increases of 257% to 700% in virtual patient visits.2 Many have participated in virtual visits through video conferencing platforms during the stay-at-home quarantine period, allowing patients to access their practitioner from home, either to address new concerns or continue follow-up care. While a good number of individual practices are using platforms that are HIPAA compliant, such as doxy.me and Eyecare Live, the requirement to store communication and ensure HIPAA compliance for all patient communications is not being enforced currently, allowing doctors to even use FaceTime or Zoom to contact patients.
Larger entities in eye care have been able to bring their institutional muscle to the problem. The New England College of Optometry partnered with EyeCare Live to establish a telehealth program that allowed NECO docs to conduct urgent evaluations, vision therapy, low vision rehabilitation and other essential consultations.3 The MyEyeDr network of practices is also working on a telehealth pilot with EyeCare Live to integrate telehealth options for patients as a routine part of its services.4 And the Veterans Affairs Administration leaned into its long-established Technology-based Eye Care Service program even more this year to perform remote screenings and exams.
The current upswing in telehealth use was borne of necessity during the pandemic but some aspects may remain even after clinical care return to more conventional modes. Telehealth expands the reach of our practices and connects us with patients who cannot physically make it to the office. The added convenience allows these patients to get eye care when they need it and enhances compliance.
For example, removing barriers of scheduling time off from work, finding transportation and/ or commuting to the doctor’s office and time spent in crowded waiting rooms, will encourage more people to support and manage their ocular health.5 Many practitioners have found that their telehealth visits were faster compared with in-office visits and believe, as patients become more familiar with telehealth, efficiency will continue to improve.5
 |
| During the stay-at-home order, some optometrists have used remote refraction software from DigitalOptometrics and used Eyecare Live to video conference with patients. Click image to enlarge. |
Remote Eye Exams
A number of companies have developed or are developing diagnostic testing systems using virtual reality headsets and smart device applications for ophthalmic assessments that include visual acuity testing, refraction determination and central visual field testing.
DigitalOptometrics has developed optical software for comprehensive eye exams via telemedicine that allows the optometrist at a remote location to evaluate patients at another location via live video conference.6 The OD can remotely operate exam equipment to perform subjective refractive findings among other tests. A comprehensive exam is reported to take less than 30 minutes on average. During the pandemic, large national retail optical providers and independent practices requested installations of the remote eye exam system at their closed locations during government-required closures.7
The ESG 1200 Eye Screening Globe by GlobeChek is a kiosk equipped with diagnostic instruments capable of distance and near visual acuity, wavefront autorefraction, intraocular pressure corrected for corneal thickness, high-resolution external photography, corneal topography, anterior segment OCT, cataract grading, fundus photography and macular and optic nerve OCT. The entire no-touch/no-dilation scan is reported to take about eight minutes.8
GlobeChek is selling and leasing its unit to customers who intend to put them in hospitals, retail chain stores, even malls, airports and other public locations where they will be operated by on-site technicians.9 Currently, the GlobeChek devices are only located in eye care providers’ offices, but the company is also working on a mobile solution that uses a trailer as an office so that patients won’t need to enter a doctor’s building.7
A similar refraction device that connects to a smart phone is the EyeQue VisionCheck.10,11 A few of the concerns with this type of at-home testing involve the accuracy of results, the lack of clinical validation, and the inability to provide an assessment of the ocular health of the eye. In April, in response to COVID-19, EyeQue offered its Personal Vision Tracker vision test free to US residents and waived annual membership fees for refraction testing in an effort to help those suddenly unable to see their optometrist check their vision.7
And an optometry-led service called Telasight launched in May at the height of the shutdown. The main intent of the service is to ease more optometrists into medical eye care by providing a safety net of experts to reach out to, but the same capabilities can be applied in the telehealth sphere as well. The company says it gives optometrists the ability to conduct a professional consult with another doctor remotely and securely, including the sharing of clinical data and images such as visual fields and OCTs.
 |
| As offices continue to open in limited capacities, many optometrists wonder whether they will continue to rely on telehealth in their day-to-day. The optometric mainstay refraction remains difficult to replicate online, though advances continue. Click image to enlarge. |
Quality Control
While many optometrists vocalize approval and support for telehealth, there are also detractors who are equally doubtful the impact of telehealth will hold past the pandemic. Though patients with emergency red eyes, dry eye, contact lens follow-ups and other anterior segment conditions seem amenable to such methods, those with corneal foreign bodies, retinal detachment, angle closure and infectious keratitis, for example, are among the many conditions that require in-office consultation and expertise.12 Techniques such as viewing the fundus, or anterior segment ocular structures with staining, also requires additional equipment and skilled, in-person evaluation.
As offices continue to open in limited capacities, some optometrists doubt that they’ll continue to rely on telehealth in their day-to-day. They resolve to prioritize in-person visits with patients that will increase slowly but surely and anticipate the time-consuming schedule.5
On the other hand, many optometrists suggest that using virtual follow-up and visits could assist with the overwhelming number of patients that desire eye care. One practice noted that telehealth allowed them to resolve space issues to have multiple doctors working at the same time, as some practitioners field telehealth appointments from their home while their colleagues physically see patients in office.5 Any patient encounters that can be done remotely opens a slot for in-person care that can’t be handled efficiently otherwise.12 Some ODs envision a hybrid model moving forward, where they can conduct in-person testing and then call to discuss the results and any care and management moving forward.
Telehealth is here to stay, but its value in the core strength of optometry—refractive assessment—has some ways to go. Many optometrists formed their opinions of remote refraction a few years ago when the now-defunct Opternative service put vision screening in the hands of patients. The confluence of low quality refractive data and an existential threat to the refractive component of practices made remote refraction a non-starter for most ODs. But its proponents will continue to iterate on such services and will look to integrate them with optical shops. Optometry’s disinterest won’t deter advancement—ignore it at your own peril.
Ultimately, it is up to each optometrist to determine which elements from the expansive field of telemedicine will augment their traditional practices to help provide and expand quality patient care, especially for those with unique situations.
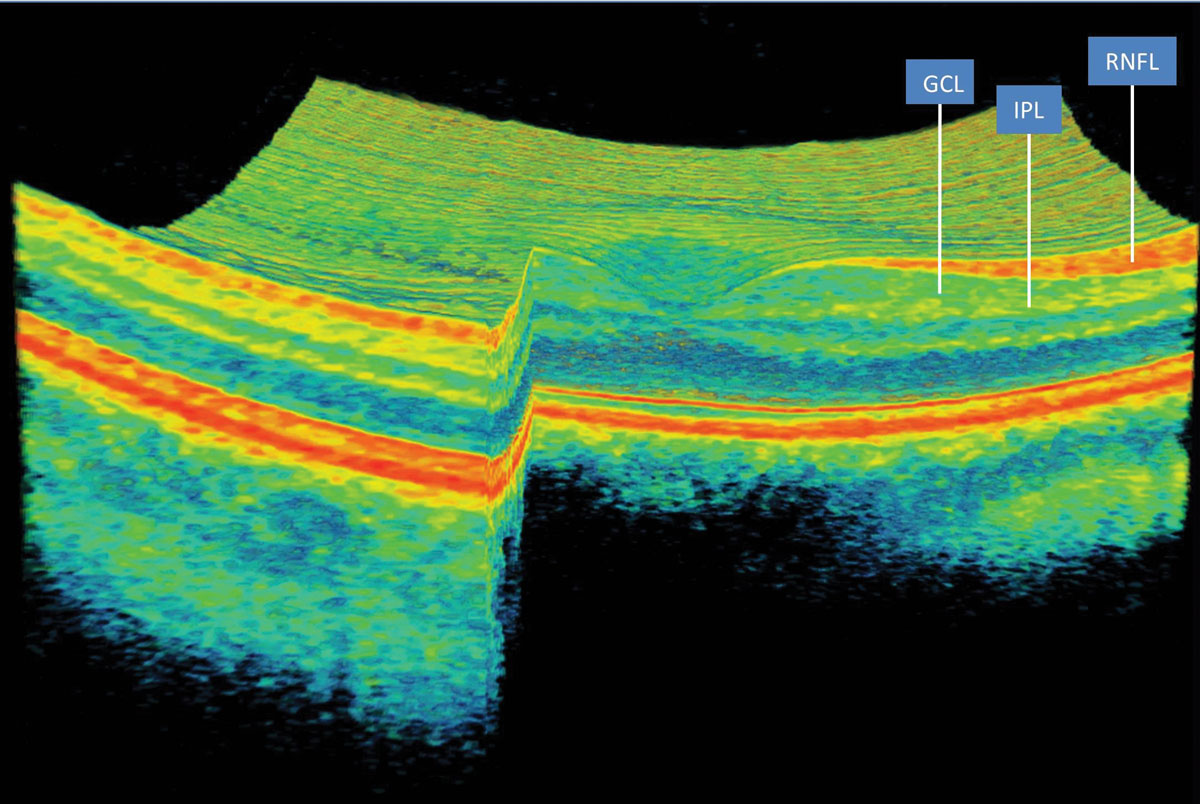 |
| The DeepMind system can convert a raw OCT scan into a 3D-tissue map to aid treatment decisions. Click image to enlarge. |
AI Gets Smarter...
The incorporation of artificial or augmented intelligence has further enhanced telemedicine capabilities, even outgrowing the provider altogether. More recently, autonomous AI systems can be trained to make clinical decisions without human oversight. AI software is developed using vast amounts of data to teach systems to diagnose conditions. In ophthalmology, autonomous AI has been studied in fundus photography, OCT and visual fields for automated detection of age-related macular degeneration (AMD), and diabetic retinopathy among other ophthalmic diseases.
AMD. One such system, DeepMind, developed by Google and the Moorfields Eye Hospital in London, demonstrated the ability to detect and classify OCT pathologies including choroidal neovascularization, macular edema, drusen, geographic atrophy, epiretinal membrane, vitreomacular traction, full- and partial-thickness macular holes, and central serous chorioretinopathy.13
In a recent study of patients diagnosed with wet AMD in one eye, the DeepMind system was able to predict progression to the second eye within a clinically actionable, six-month time window.14 By combining models based on three-dimensional OCT images and corresponding automatic tissue maps, the system predicted conversion and achieved a per-volumetric-scan sensitivity of 80% at 55% specificity, and 34% sensitivity at 90% specificity.14
Diabetic retinopathy. Screening for DR has proven to be a simple and cost-effective way to detect disease that adapts easily to telemedicine and AI, either as a first pass to reduce burden on human expert graders or as a replacement for human expert graders for even more cost-effective means.
In April 2018, the FDA approved the first autonomous software (IDx-DR) for point-of-care diagnosis of DR without physician or human interpretation. IDx has since become part of the American Diabetes Association standard of diabetes care recommendations.15,16
A recent study found the IDx-DR was a reliable screening tool when used to diagnose diabetic retinopathy in the primary care office that could reduce barriers to screening and improve gaps in diabetes treatment.16 The sensitivity of detecting “more than mild” DR was 87% and specificity was 91%.17,18 The camera used in the system was easy to learn, and staff were taught to reliably obtain images without direct physician supervision. Examination with the IDx-DR system was not invasive and did not require dilation.17
A second device, EyeArt (Eyenuk), has recently been cleared by the FDA to automatically detect “more than mild” DR and vision-threatening DR in eyes of adults diagnosed with diabetes.19 Similar to the IDx, novice operators can be trained to obtain medical grade retinal images. EyeArt provided disease detection results for 97% of eyes, and a vast majority of participant eyes (90%) received disease detection results without needing dilation.19
“Eyenuk is on a mission to screen every eye in the world to ensure timely diagnosis of life- and vision-threatening diseases,” said its founder and CEO, Kaushal Solanki, PhD, in a press release announcing its partnership with Devlyn Optical, a chain that operates in the US and Mexico, to put devices in their stores.20
 |
| In practices using the IDx-DR system, staff were taught to reliably obtain images without direct physician supervision. Click image to enlarge. |
...But More Troublesome
While these diagnostic telemedicine and AI systems hold great promise, they are not without challenge and concern. Most development has been occurring in private industry, so there is limited research, scrutiny and transparency that would be needed for incorporation into the medical industry. Rigorous validation is needed to ensure safety and limit any unexpected problems during real world implementation.15
There are also ethical and legal concerns. Autonomous AI is a very new concept, there are no generated rules to follow for ethical human-computer interaction. Liability is a concern, as, legally, the creators of the autonomous AI assumes liability for harm caused by the diagnostic output of the device, but who owns the patient data generated and who defines appropriate use of patient data? Most state medical boards do not consider an autonomous AI output to have the same medicolegal status as physician.
And finally, the successful clinical implementation of AI requires provider trust that the system improves patient outcomes, works equally well on the vast majority of patients and doesn’t threaten physicians. The IDx-DR system has been met with professional concern, where some ophthalmologists disagree, resent or even fear autonomous AI for the diabetic eye exam for disease.21
In an effort to protect the many forms of AI in healthcare, the American Medical Association adopted the term “augmented intelligence” to portray AI as broad, with autonomous AI as just one subtype. Many other forms of AI exist that rely on human physician interpretation.22
Advanced technology like AI can help improve access to care with increased accuracy and decreased cost. Deployed in retail or health settings outside the eye care’s office, it can identify more patients that need our expertise in-office. Though AI can be trained to be consistently detail-oriented and resistant to fatigue, it will not replace the eye care provider. Our human ability to use higher levels of metacognition and intuition allows us to recognize and manage out of the box abnormalities, something that is yet transferable to an algorithm.
Whether or not there’s another shutdown that forces change in our practice, optometrists should be prepared for the future of expanded eye care. Many have now seen the value and the opportunity of technology to care for patients remotely. We need not worry that we are going to be replaced by telehealth or AI—clinical decision-making has always been and will continue to be required for optimal patient care Advances in both of these spheres will increase accessibility to healthcare, increase awareness of ocular disease and identify more patients whose outcomes can be improved by the unique skill set that optometrists can provide.
Dr. Shahid is a clinical assistant professor in the Department of Ophthalmology and Visual Sciences at the University of Iowa’s Carver College of Medicine, where she provides primary eye care and vision rehabilitation.
Dr. Wilkinson is a clinical professor in the Department of Ophthalmology and Visual Sciences at the University of Iowa’s Carver College of Medicine. He is the director of the institution’s Vision Rehabilitation Service and a faculty member of the University of Iowa Institute for Vision Research and the National Advanced Driving Simulator.
1. Parke DW. Ophthalmology after coronavirus disease 2019 (COVID-19): transition back to patient care.JAMA Ophthalmol. 2020;138(6):599-600. 2. Saleem SM, Pasquale LR, Sidoti PA, Tsai JC. Virtual ophthalmology: telemedicine in a COVID-19 era. Am J Ophthalmol. 2020;216:237-42. 3. NECO Magazine. NECO eye clinics launch telehealth for specialty services and urgent eyecare. New England College of Optometry. www.neco.edu/news/entry/neco-eye-clinics-launch-telehealth-for-specialty-and-urgent-eyecare-visits. April 9, 2020. Accessed September 9, 2020. 4. Karp A, Tosh M. Retailers find telehealth options improve the patient experience. Vision Monday. www.visionmonday.com/eyecare/article/retailers-find-telehealth-options-improve-the-patient-experience. June 22, 2020. Accessed September 9, 2020. 5. Karp A, Tosh M. Making the leap into telehealth. Vision Monday. www.visionmonday.com/eyecare/article/making-the-leap-into-telehealth. June 22, 2020. Accessed September 9, 2020. 6. DigitalOptometrics. www.digitaloptometrics.com. Accessed September 9, 2020. 7. Karp A, Tosh M. Adjusting to the new normal: how ocular telehealth can help. Vision Monday. www.visionmonday.com/eyecare/article/adjusting-to-the-new-normal-how-ocular-telehealth-can-help. June 22, 2020. Accessed September 9, 2020. 8. GlobeCheck. www.globechek.com. Accessed September 9, 2020. 9. VM Staff. COVID-19 crisis response tactics: GlobeChek, Maui Jim, Transitions Optical. Vision Monday. www.visionmonday.com/eyecare/coronavirus-briefing/crisis-response-tactics/article/covid19-crisis-response-tactics-globechek-maui-jim-transitions-optical. May 15, 2020. Accessed September 9, 2020. 10. EyeQue. www.eyeque.com. Accessed September 9, 2020. 11. Karp A, Tosh M. Vision care grows up. Vision Monday. www.visionmonday.com/eyecare/article/virtual-vision-care-grows-up. June 22, 2020. Accessed September 9, 2020. 12. Karp A, Tosh M. Envisioning the future of ocular telehealth. Vision Monday. www.visionmonday.com/eyecare/article/envisioning-the-future-of-ocular-telehealth. June 22, 2020. Accessed September 9, 2020. 13. Ting DSW, Pasquale LR, Peng L, et al. Artificial intelligence and deep learning in ophthalmology. Br J Ophthalmol. 2019;103(2):167-75. 14. Yim J, Chopra R, Spitz T, et al. Predicting conversion to wet age-related macular degeneration using deep learning. Nat Med. 2020;26(6):892-9. 15. Abramoff A. The autonomous point of care diabetic retinopathy examination. In: 15. Klonoff DC, Kerr D, Mulvaney SA, eds. Diabetes Digital Health. Elsevier; 2020:159-78. 16. Mudie LI, Wang X, Friedman DS, Brady CJ. Crowdsourcing and automated retinal image analysis for diabetic retinopathy. Curr Diab Rep. 2017; 17(11):106. 17. Savoy M. IDx-DR for diabetic retinopathy screening. Am Fam Physician. 2020;101(5):307-8. 18. Bellemo V, Lim G, Rim TH, et al. Artificial intelligence screening for diabetic retinopathy: the real-world emerging application. Curr Diab Rep. 2019;19(9):72. 19. Eyenuk. Eyenuk announces FDA clearance for EyeArt autonomous AI system for diabetic retinopathy system. BusinessWire. www.businesswire.com/news/home/20200805005495/en/Eyenuk-Announces-FDA-Clearance-EyeArt-Autonomous-AI. August 5, 2020. Accessed September 9, 2020. 20. Multinational optical retailer piloting AI and telemedicine technology to protect community eye health during the COVID-19 pandemic. Business Wire. financialpost.com/pmn/press-releases-pmn/business-wire-news-releases-pmn/multinational-optical-retailer-piloting-ai-and-telemedicine-technology-to-protect-community-eye-health-during-the-covid-19-pandemic. June 8, 2020. Accessed September 23, 2020. 21. McDonnell PJ. ‘The Retinator’: revenge of the machines. Ophthalmol Times 2010;35(13):4. 22. American Medical Association (AMA). Augmented intelligence in healthcare; 2019. |

