Idiopathic juxtafoveal retinal telangiectasis (IJRT) is a rare disorder. The condition is discernible by clinical presentation along with the use of fluorescein angiography and ocular coherence tomography.
IJRT is subdivided into different types, and further subdivided into subtypes and stages. The treatment of the disease is controversial and mostly depends on the patient’s level of symptoms and clinical signs.
|
|
|
|
|
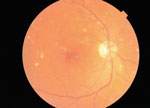
Fundus photographs show dot and scattered hemorrhages OD (left) and pigment mottling OS (right). Both eyes have a pseudohole appearance.
|
History
A 55-year-old white male presented with an emergent complaint of increased black spots in the vision of his right eye. He had noticed that the black spots had been increasing in size and number, along with increased blurry vision over the past six to eight months. His past ocular history was unremarkable. He had not had an eye exam in over three years.
His systemic history was positive for poorly controlled Type 1 diabetes; his last A1c reading was 9.8. He also reported hyperlipidemia and hypertension. His blood pressure was 132/78 the morning of the exam. Systemic medications included temazepam, atenolol, glipizide, insulin, metformin, omeprazole, multivitamins and aspirin (325mg).
Diagnostic Data
Visual acuity at presentation was 20/60 OD with pinhole to 20/40 and 20/30 OS with pinhole to 20/25. Following refraction, the patient’s best-corrected visual acuity was 20/40 OD and 20/25 OS. The refraction yielded -1.00 DS in the right eye and -0.50 DS in the left eye. The patient had no deficiencies on extraocular motility or confrontation visual field testing. He had equal, round, reactive pupils with no afferent defect. Amsler grid revealed metamorphopsia nasally in both eyes.

|
|
|
Arrow points to telangiectatic vessel, OD.
|
|
Biomicroscopy uncovered trace seasonal allergic conjunctivitis with mild papillae and punctate keratitis. He had mild nuclear sclerosis in the lenses of both eyes. Goldmann applanation tonometry pressures measured 18mm Hg OU.
Dilated fundus exam revealed two small dot hemorrhages inferior to the central macula with a few scattered hemorrhages temporally, along with a pseudohole appearance in the macula of the right eye. The macula of left eye had a slightly elevated appearance with pigment mottling and a few small hemorrhages surrounding it. The left eye also had a pseudohole appearance. Both eyes had a negative Watske-Allen sign.
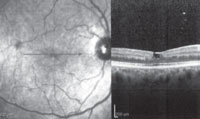
Optical coherence tomography (OCT) showed a subfoveal macular cyst-like appearance secondary to atrophy that affected the foveal contour in both eyes.
Diagnosis
Based on the OCT results, we tentatively diagnosed the patient with idiopathic juxtafoveal retinal telangiectasis. We referred the patient to a retina specialist, who confirmed the diagnosis of type 2 IJRT using fluorescein angiography.
|
|
|
|
|
OCT scans, both OD (left) and OS (right), show subfoveal macular cyst-like appearance due to atrophy affecting the foveal contour.
|
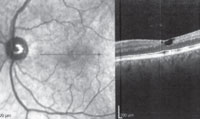
Flourescein angiography is the diagnostic tool of choice for IJRT. The irregular dilation of capillaries is easily seen on the arteriovenous phase, along with leakage of dye from the affected capillaries into the intracellular spaces of the retina.1 In our patient, both eyes showed punctate hyperfluorescent spots within the central macula in the early phases, along with leakage seen in the late phases.
OCT is another important diagnostic tool used in this disease. Features of IJRT seen on OCT are most commonly loss and disruption of the photoreceptor layer, cyst-like structures in the fovea and within intra-retinal layers, possible neovascularization, and intra-retinal deposits and plaques. The discontinuity of the photoreceptors is correlated with loss of visual acuity. If the photoreceptor layer is intact, the visual acuity is usually preserved.2 Gass concluded the loss of central vision is due to photoreceptor atrophy in the absence of macular edema.3
|
|
|
|
|
Fluorescein angiography (FA) in the patient’s right eye: early arteriovenous phase (left) and late arteriovenous phase (right).
|
|
|
|
|
|
FA in the left eye: early arteriovenous phase (left) and late arteriovenous phase (right). Both eyes show punctate hyperfluorescent spots within the central macula in the early phases, and leakage in the late phases.
|
Another unique feature seen on OCT is the internal limiting membrane (ILM) drape, as seen in our patient. The draping of the ILM over the fovea is due to underlying loss of tissue, causing a cystoid space. This draping shows the loss of the outer plexiform layer due to a cystoid space underneath the fovea that allows the retina to have a normal foveal contour and foveal thickness.2 Foveolar atrophy is easily seen on OCT and may mimic a lamellar macular hole. This atrophy is the main cause of slow progressive vision loss over time, whereas rapid and severe vision loss occurs with the development of a neovascular membrane.3
Treatment and Follow-up
The patient did not receive any treatment for this condition. He will be monitored by the retina specialist closely on a monthly basis initially, with the goal of every other month for the balance of the year.
He was dispensed an Amsler grid and educated on the signs and symptoms of decompensation. After his initial visit, the patient missed his two follow-up appointments and returned for a three-month follow-up and then again two months later. The patient’s visual acuity had slightly decreased in subsequent follow-up visits.
Discussion
Idiopathic juxtafoveolar retinal telangiectasias are a group of rare retinal vascular disorders characterized by alterations of the juxtafoveolar capillary network in one or both eyes that is detectable even in asymptomatic patients.4
This disease is more specific to the parafoveal region of the retina. Therefore, it becomes easily distinguishable from other generalized retinal telangiectasias such as Coats’ disease or a secondary telangiectasis found in retinal vein occlusions, carotid artery disease or diabetes.3
|
Classification of IJRT by Type
|
||||
| Type | 1A | 1B | 2 | 3 |
| Frequency |
2nd most common
|
Rare | Most common | Very rare |
| Gender |
Male (90%)
|
Male | Male = Female | Male = Female |
| Age | 15-54 | 40-50 | 35-65 | 40-60 |
|
Congenital/acquired
|
Congenital
|
Congenital
|
Acquired
|
Acquired
|
|
Laterality
|
Unilateral | Unilateral | Bilateral | Bilateral |
|
Visual acuity at presentation
|
Around 20/40
|
≥20/25
|
20/20 to 20/300
|
20/25 to 20/50
|
| Classic signs |
Exudates and macular edema
|
Exudates and macular edema
|
Foveolar atrophy or CNV (stage 5)
|
Capillary obliteration
|
|
Systemic associations
|
None | None |
Possible diabetes
|
CNS involvement
|
IJRT was first identified by Gass and Oyakawa in 1982.5 They classified the disease into four groups based on clinical features and results from fluorescein angiography. Gass and Blodi updated this classification system in 1993.3 They divided IJRT into three groups with smaller subgroups within the first group. (See “Classification of IJRT by Type,” above.) This most recent classification system is widely accepted and described as follows:3
• Type 1. The hallmark characteristic of type 1 is variable sized aneurysmal dilations and easily visible telangiectasis of the retinal capillaries.3
Type 1 is subdivided into types 1A and 1B.5 Each are unilateral and congenital, typically affecting men in their 30s and 40s.6 The vision loss in type 1A is more significant than in type 1B.3
|
|

|
|
|
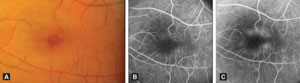
Type 2, stage 1 IJRT: fundus photo (A) with images of early phase FA that shows punctate staining (B) and late phase shows mild leakage (C). Images: Nowilaty S, Al-Shamsi H, Al-Khars W. Idiopathic juxtafoveal retinal telangiectasis: a current review. Middle East Afr J Ophthalmol. 2010 Jul;17(3):224-41.
|
|
|
|
|
|
Type 2, stage 2 IJRT: fundus photo (A) with early phase (B) and late phase showing leakage (C).
Images: Nowilaty S, Al-Shamsi H, Al-Khars W. Idiopathic juxtafoveal retinal telangiectasis: a current review. Middle East Afr J Ophthalmol. 2010 Jul;17(3):224-41.
|
|
|
|
|
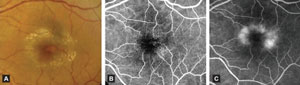
|
Type 2, stage 3 IJRT: fundus photo (A) shows grayish ring with crystals surrounding the macula. Early phase of FA shows visible telangiectasis (B) and late phase shows late leakage (C). Images: Nowilaty S, Al-Shamsi H, Al-Khars W. Idiopathic juxtafoveal retinal telangiectasis: a current review. Middle East Afr J Ophthalmol. 2010 Jul;17(3):224-41.
|
Subgroup 1A is the second most common of all types and can be found in males ranging in age from 15 to 54.1 The telangiectasis of the capillaries is typically found in the temporal half of the macula involving an area of two disc diameters or greater.7 In these patients, the decreased vision ranges from 20/25 to 20/40.
Subgroup 1B is rare and affects mostly middle-aged men between the ages of 40 and 54.6 The difference between subgroup 1B and 1A differs primarily in the size of the area of telangiectases. These telangiectases occupy small focal areas less than one disc diameter adjacent to the foveal avascular zone.7,8 The amount of vision loss in this subgroup is much less where the men are either asymptomatic or have vision better than 20/25.6
In both subtypes, cystoid macular edema may develop and will show classic petalloid leakage on fluorescein angiography.6 Macular edema and lipid exudation are the main cause of vision loss in type 1.3
• Type 2. Type 2 is bilateral, acquired and has no gender predilection. This is the most common type of IJRT and is significantly different from type 1.3 Although type 2 is considered the most common, its prevalence was found to be very low—0.1%—by the Beaver Dam Eye Study and even lower—0.004% to 0.022%—in the Melbourne Collaborative Cohort Study.9 Age of onset is typically in the 40s or 50s.
The most common clinical sign in type 2 is foveolar atrophy. The characteristics are usually symmetric, but vision loss may be asymmetric. Vision loss ranges from asymptomatic to mild blurring of central vision to slow progressive loss of central vision. The vision loss can occur slowly, but may become rapid with the development of intra-retinal neovascularization.10 Some research suggests that diabetes may be an underlying cause for this group.11
IJRT type 2 is further subdivided into five stages (see “Stages of Type 2 IJRT,” below) by characteristics of the different signs and symptoms:
Stage 1. Patients are typically asymptomatic in stage 1. The retina typically looks slightly grayish and there could be a loss of retinal trans-parency.3 Stage 1 signs may be difficult to identify by biomicroscopy alone. Fluorescein angiography will show juxtafoveolar telangiectasis in stage 1 even if there are no abnormalities seen during clinical examination.10
Stage 2. In stage 2, evidence of the disease starts to be slightly more obvious with biomicroscopy. There is graying of the parafoveolar region that is usually confined to the temporal side or forming a horizontal oval around the fovea while sparing the foveal center. Although the fovea is spared, it may look slightly thinner than the surrounding retina. Minimal telangiectatic changes usually occur at this stage, giving it a subtler appearance than type 1 IJRT.3
|
Stages of Type 2 IJRT
|
| ||
|
|
Signs |
Symptoms
|
|
| Stage 1 |
Retina appears grayish; telangiectasis visible by IVFA only
|
Typically asymptomatic
|
|
| Stage 2 |
Graying of parafoveal region on temporal aspect of macula; thinning of foveal region seen
|
Typically asymptomatic
|
|
| Stage 3 |
Right-angle venules mostly temporal to fovea; blunted foveal reflex
|
Mild vision loss (usually when patient presents to clinic)
|
|
| Stage 4 |
Clumps of RPE hyperplasia seen around right angle venules; pseudovitelliform lesion sometimes seen
|
Vision loss worsens
|
|
| Stage 5 |
Development of a neovascular membrane; superficial crystalline deposits may develop |
Most detrimental vision loss
|
|
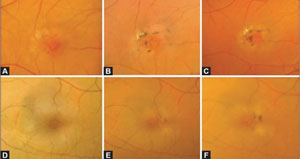
Stage 3. Stage 3 exhibits right-angle venules, mostly found temporal to the fovea, but they can also surround the fovea with a blunting of the foveal reflex.6 Most patients present to clinic during stage 3 due to the complaint of mild vision loss. This vision loss appears to be due to progressive foveolar atrophy.10 The foveolar depression may mimic a macular hole in this stage when viewed by biomicroscopy, but is easily distinguishable by fluorescein angiography.3
Stage 4. Stage 4 is characterized by clumps of retinal pigmented epithelial hyperplasia seen around the right-angled vessels in the parafoveal region that are associated with chorioretinal anastomosis.3,10 A stellate pattern of retinal pigmented epithelial hyperplasia may envelop the macula during this stage, and some patients may develop a pseudovitelliform lesion.3,6
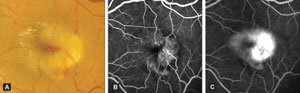
Stage 5. Stage 5 is the final stage of type 2 IJRT. This is the stage that is most detrimental to vision due to the development of an intra-retinal neovascular membrane (NVM). The NVM may occur as a result of retinal capillary remodeling, proliferation and invasion of the outer retina that has progressively atrophied from the disease.3 In 40% to 45% of eyes in stage 5, superficial retinal crystalline deposits of unknown etiology have been reported. The significance of these refractile deposits is currently unknown, and they may occur at any time between stages 2 and 5.10
Refractile crystals may be present in other retinal disorders, but these crystals have distinguishing characteristics, such as showing specular reflection and being distributed in an annular pattern around the fovea, sparing it centrally.12
• Type 3. The final group is type 3, which is bilateral perifoveal telangiectasis with capillary obliteration. This type is extremely rare and usually occurs in a patient’s 40s with no gender predilection. Aneurysmal dilation occurs, along with the capillary obliteration without leakage. This causes slow, progressive vision loss in patients. This type is associated with other sequelae such as optic nerve head pallor, hyperactive deep tendon reflexes and central nervous system (CNS) symptoms.6
Type 3 is suspected to be autosomal dominant in inheritance pattern and is known to be associated with cerebroretinal vasculopathy.8 Researchers have shown evidence of CNS pseudotumor characterized by unusual vasculopathy with fibrinoid necrosis and necrosis of white matter.8 If you suspect CNS symptoms, refer patients to a neurologist.6
|
|
|
|
|
Type 2, stage 4 IJRT: Serial fundus photos of a patient’s right eye (A-C) and left eye (D-F) shows RPE hyperplasia. Images: Nowilaty S, Al-Shamsi H, Al-Khars W. Idiopathic juxtafoveal retinal telangiectasis: a current review. Middle East Afr J Ophthalmol. 2010 Jul;17(3):224-41.
|
|
|
|
|
|
Type 2, stage 5 IJRT: Fundus photo of subretinal neovascularization shows refractile crystals (A) with corresponding early phase (B) and late phase (C) FA images. Images: Nowilaty S, Al-Shamsi H, Al-Khars W. Idiopathic juxtafoveal retinal telangiectasis: a current review. Middle East Afr J Ophthalmol. 2010 Jul;17(3):224-41.
|
Overall, the most common symptoms reported by patients are blurred vision, metamorphopsia and possible scotomas when checked with Amsler grid.1 This contrasts with the many asymptomatic patients with type 1 or the early stages of type 2. (See Classification of IJRT by Type.”)
Pathogenesis
The pathogenesis and etiology of IJRT are unknown at this time. One study by Sallo et al. suggested looking into the physical and chemical properties of the retinal crystals to find information on the metabolic pathways involved in the pathogenesis of the disease.12
Other researchers have suggested that the histopathology of IJRT may be linked to dysfunction of the Muller cells.3 The crystalline deposits have been thought to be remnants of degenerated Muller cells due to the location near the ILM.
Management
Although a number of studies have attempted to determine the best treatment of IJRT, no treatment modality has been able to show consistent efficacy.7,13,14
Some of these studies are contradicting, but the current treatments include intravitreal bevacizumab injections, focal grid laser photocoagulation or photodynamic therapy (PDT).7,13,14
If patients are asymptomatic or have minimal vision loss, usually no treatment is recommended.6
If a pronounced macular edema is seen in type 1, patients may benefit from intravitreal bevacizumab injections.13 One study of type 1 patients used laser photocoagulation to prevent the accumulation of lipids in the fovea, especially if no prior accumulation of exudates existed.11
The treatment of type 2 IJRT is more controversial. A study concluded that if minimal cystic changes are seen on OCT, repeated injections will not produce functional improvement.13 Another study found intravitreal bevacizumab provided short-term improvement in vision due to decrease in retinal thickness and a reduction of angiographic leakage.14 The use of focal laser photocoagulation is performed only if neovascularization is present outside the foveal area.6
Again, this treatment is controversial because some studies have shown no significant improvement of visual outcome with focal/grid photocoagulation. Reports show an increased risk of the development of subsequent neovascularization after treatment.
Recently, PDT has been used to resolve leakage of a neovascular membrane, but there is no effect on edema associated with telangiectasis.10
Currently there are no treatments available for the ocular manifestations of type three IJRT.
Unfortunately, the rarity of this disease makes the treatment difficult to assess in a controlled but random manner. Gass and Blodi did not recommend laser photocoagulation in type 2 if it is non-proliferative due the long-term prognosis already being poor. If type 2 is proliferative, anti-VEGF treatment such as bevacizumab may be efficacious.3
Comanage the treatment of these patients with a retinal specialist, as a fluorescein angiography is necessary to confirm the diagnosis and staging of IJRT.
IJRT is not a common disease entity. It is often misdiagnosed as retinopathy secondary to other diseases such as diabetes or sequelae of an old venous occlusion. Fluorescein angiography and ocular coherence tomography are tools that aid in the definitive diagnosis of this retinal disease. The different groupings and stages assist the clinician in determining an accurate prognosis and the best course of treatment.
Dr. Cooper is a fee-basis optometrist at the C.W. Bill Young VA Medical Center in Bay Pines, Florida. Dr. Gruosso is a staff optometrist also at the C.W. Bill Young VA Medical Center, where he is the director of the low vision clinic and student externship program. Dr. Miller is a staff optometrist and residency program coordinator at the C.W. Bill Young VA Medical Center.
1. Gass JD, Oyakawa RT. Idiopathic juxtafoveolar retinal telangiectasis. Arch Ophthalmol. 1982 May;100(5):769-80.2. Paunescu L, Ko T, Duker JS, et al. Idiopathic juxtafoveal retinal telangiectasia: new findings by ultrahigh-resolution optical coherence tomography. Ophthalmology. 2006 Jan;113(1):48-57.
3. Nowilaty S, Al-Shamsi H, Al-Khars W. Idiopathic juxtafoveal retinal telangiectasis: a current review. Middle East Afr J Ophthalmol. 2010 Jul;17(3):224-41.
4. Wu. J, Ferrucci S. Idiopathic juxtafoveal retinal telangiectasia. Optometry. 2008 Nov;79(11):653-62.
5. Chhablani J, Kozak I. Multimodal imaging in idiopathic juxtafoveal retinal telangiectasia. Retinal Physician. 2013 Jan;10:62-64.
6. Friedman N, Kaiser P, Pineda R. The Massachusetts Eye and Ear Infirmary Illustrated Manual of Ophthalmology. 3rd ed. Philadelphia: Saunders Elsevier; 2009: 352-3.
7. Lee S, Kim S, Kim Y, Kang SW. Clinical features of idiopathic juxtafoveal telangiectasis in Koreans. Korean J Ophthalmol. 2011 Aug;25(4):225-30.
8. Pauleikhoff D, Padge B. Vascular Abnormalities: Idiopathic Juxtafoveolar Retinal Telangiectasis. In: Joussen AM, Gardner TW, Kirchhof B, Ryan SJ. Retinal Vascular Disease. Berlin/Heidelberg: Springer; 2007: 528-534.
9. Klein R, Blodi B, Meuer S, et al. The prevalence of macular telangiectasis type 2 in the Beaver Dam Eye Study. Am J Ophthalmol. 2010 Jul;150(1):55-62.
10. Engelbrecht NE, Aaberg TM Jr, Sung J, Lewis ML. Neovascular membranes associated with idiopathic juxtafoveolar telangiectasis. Arch Ophthalmol. 2002 Mar;120(3):320-4.
11. Bonyadi M, Moradian S. Large juxtafoveal telangiectasia. J Ophthalmic Vis Res. 2010 Jul;5(3):202-4.
12. Sallo FB, Leung I, Chung M, et al; MacTel Study Group. Retinal crystals in type 2 idiopathic macular telangiectasia. Ophthalmology. 2011 Dec;118(12):2461-7.
13. Gamulescu MA, Walter A, Sachs H, Helbig H. Bevacizumab in the treatment of idiopathic macular telangiectasia. Graefes Arch Clin Exp Ophthalmol. 2008 Aug;246(8):1189-93.
14. Charbel Issa P, Holz FG, Scholl HP. Findings in fluorescein angiography and optical coherence tomography after intravitreal bevacizumab in type 2 idiopathic macular telangiectasia. Ophthalmology. 2007 Sep;114(9):1736-42.

