Confused about dry eye? Youre in good company. In late April, optometrist Carolyn Begley sat at the Symptoms table among other international researchers at a dry eye symposium. Other dry eye experts at the symposium, held at the Association for Research in Vision and Ophthalmology (ARVO) meeting, filled two additional tables; one table represented Surface Staining and another Tear Film. The discussion focused on how each area impacted diagnosis and treatment of dry eye.
It was interesting, says Dr. Begley, a professor at Indiana University School of Optometry. At the symptoms table, we all agreed that symptoms needed to be taken into account [for diagnosis and treatment]. But at the other tables, they couldnt agree on the clinical signs that were the most important.
Signs of dry eye dont necessarily match the symptoms. One recent study found that about one in three patients with moderate/severe symptoms had no surface staining.
The debate is both an emblematic and a literal example that even the experts dont understand dry eye. This complicates treatment. We dont really understand where the symptoms come from, Dr. Begley says. She points to the disconnect between the symptoms that patients report and the clinical signs that patients demonstrate. They dont necessarily match up.
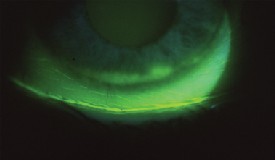
Surface staining is one example. You would think that if you put in a stain, that tells you where the dead cells are. Wherever there are dead cells, you would expect a person to have symptoms. That should tell you the answer.
But instead of an answer, it raises more questions. Thats because surface staining doesnt always correlate with symptoms. Not only does staining not correlate, but you dont have to have it to have symptoms, Dr. Begley says.
In one study, she found that nearly one in three patients with moderate to severe symptoms had no surface staining.1 What that study did find, though, is that clinicians use both signs and symptoms of dry eye to gauge the severity of the condition. Moreover, clinicians likely give greater weight to patient symptoms in making a diagnosis.
Dry Eye on Trial
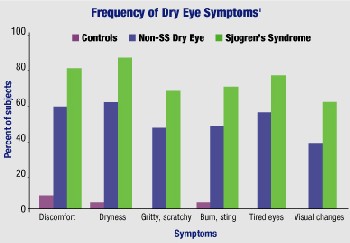
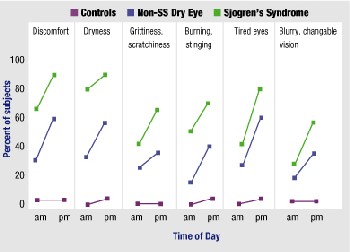
Symptoms worsen as the day goes on.1 The top chart shows the percentage of patients who report moderate to extreme symptoms. The bottom chart shows the diurnal change in the proportion of subjects who report moderate to severe symptoms.
Put another way, clinicians view dry eye as a symptom-based disease, and they determine it through a diagnosis of exclusion, says optometrist and researcher Kelly K. Nichols, assistant professor of clinical optometry at the Ohio State University College of Optometry.
This isnt exactly news to many clinicians. But what you may not know is that this does have a serious impact on treatment. Thats because clinical trials for drugs developed to treat dry eye do not look at the condition as only a symptom-based disease, Dr. Nichols says. Rather, pharmaceutical studies must rely not only on symptoms but on clinical tests for dry eye in order to demonstrate a measurable change in improvement.
To be included in most studies, patients must have clinically significant symptoms and results on standard diagnostic tests, and they must demonstrate those results again on follow-up. Essentially, patients must re-qualify for the study each time they are examined, Dr. Nichols says.
As an example, very often, only the patients who have grade 2 and above conjunctival staining and Schirmer tests below 5mm are entered into the studies, says optometrist and researcher Robin Chalmers, a clinical trial consultant in Atlanta.
Thats appropriate for patients with severe symptoms, Dr. Chalmers says, but such studies leave out patients who make up the majority of dry eye sufferers: those with mild to moderate symptoms. These are the patients who are more likely to find their way into your chair.
Those drugs [in clinical trials] end up being indicated for people with a severe problem and may not be necessarily appropriate for the other people with milder signs, Dr. Chalmers says. My point is that this market could expand tremendously if you accept that having symptoms and few signs is a type of patient to study and treat. If you can then show improvement in the symptoms, youve proven something about whether the drug or the treatment works.
Headaches Dont Need Tests Practical Pearls for Dry Eye Patients One patient may describe dry eye as gritty. Another might say burning. Dont worry about pinning down the terminology, says Kelly K. Nichols, O.D., Ph.D. Instead of sorting through a thesaurus of sandy, dry, and stinging, ask the patient to describe his or her single worst symptom. Record that in the chart, and monitor for improvement by asking about the severity of that particular symptom (say, on a scale of 1-10) at each visit. Dry eye symptoms appear more strongly and/or more often at the end of the day, say Dr. Nichols, Carolyn Begley, O.D., and Robin Chalmers, O.D. This is especially true for contact lens wearers.6 Ask patients specifically about end-of-day symptoms. Better yet, schedule these patients toward the end of the day for a better opportunity to observe signs and query for symptoms. Be sure to ask elderly patients about dry eye. The severity of dry eye in the elderly, both men and women, is underestimated, Dr. Chalmers found.4 Elderly patients often take medications (or combinations of medications) that have a drying effect. Also, their lifestyles are such that they tend to read a lot or do other tasks in which dry eye interferes with function. If the patient presents with signs of bacterial over-colonization and/or significant lid inflammation, its OK to prescribe a short-term antibiotic or antibiotic-steroid combination at bedtime after lid hygiene. But skip the messy, gooey ointment and use drops, says Arthur Epstein, O.D. Diagnosing and counseling a patient can take up a lot of chair time, Dr. Nichols says. Dont shortchange the patient on diagnosis by sending her home with a few hurried words and a random sample bottle of drops. (A study Dr. Nichols conducted found that many clinicians diagnose dry eye with only two diagnostic criteria, one of which is a symptom assessment.7 One in five clinicians uses only one criterion.) At the same time, you need not give away your clinical expertise if you can bill for it. To that end, have patients come back for a full dry eye evaluation thats separate from a routine examination, Dr. Nichols says. Brush up on your medical billing codes and charge appropriately.
A major hurdle is that current diagnostic tests for dry eye are not always repeatable for mild to moderate dry eye patients, Dr. Nichols says. In a recently published study, she and her co-authors found lackluster repeatability in most dry eye measurements.2 In particular, inferior corneal staining (fluorescein and rose bengal) and grading of meibomian gland disease both had poor repeatability.
Schirmer testing, as found in previous studies, also showed variable results from visit to visit. However, with wetting scores of less than 10mm (i.e., in patients with more advanced disease), repeatability was improved. Repeatability of tear break-up time, however, was substantial.
Heres how: Tell the patient to shake the bottle, look up directly at the dropper, close the eye and drop one drop directly on their lid margin. Rub it in with the pinky. Air dry by fanning the eye. As the patient sleeps, the eye will weep a little. This reconstitutes the antibiotic or combination to provide a kind of slow-release therapeutic effect. In the morning, a quick wash of the face will remove any residue.
Its great for contact lens wearers, Dr. Epstein says, because theres no gunk left, and its actually easier to apply than ointment.
If we test on visit one and then do the same tests two weeks later, we often find that we dont get the same results, Dr. Nichols says. Now, is that because their disease changes within that same period of time, or is it because the test is just not repeatable between those two visits due to the nature of the test? We dont know the answer.
But one thing Dr. Nichols has found is that patients subjective reporting of symptoms is repeatablemoderate to highly so in this study. Similarly, Drs. Chalmers and Begley presented a paper at this years ARVO meeting that found that patients reported a very high repeatability of symptoms (more than 90%) over a two-week period.3
So, between patient-reported symptoms and diagnostic tests, most optometrists can rely much more on symptoms to diagnoseand then treatdry eye.
In the same way that the three most important keys to success in starting a restaurant are location! location! location!, the three most important keys to dry eye diagnosis have been history! history! history!, says Arthur Epstein, O.D., president of the Optometric Dry Eye and Ocular Surface Disease Society.
If thats true, and symptoms are reliable, why are there still so many people with undiagnosed dry eye? For one reason or another, clinicians do not diagnoseor they underdiagnosethese patients. Drs. Chalmers and Begley conducted a study that compared doctor and patient perceptions of dry eye.4 They found that patients typically perceive their dry eye to be worse than what the doctor perceives it to be. Specifically, patients in the study were four times as likely to describe their condition as more severe compared with what the doctor judged as the severity. Similarly, more than one in three patients reported moderate symptoms, yet doctors identified only one in five patients with moderate symptoms.
Dr. Begley uses the analogy of a headache, which is usually diagnosed entirely on patient symptoms. A neurologist would be negligent if he had to see signs of a headache before treating the patients discomfort or pain. Cant eye doctors do the same for dry eye patients?
Out of the Pigeonhole Dry Eye Drugs in the Pipeline Secretagogues Immunomodulator Androgen Therapy
In other words, what if everything looks okay, but the patient is still complaining? Dr. Epstein asks. The average doctor would simply say the patient is nuts.
However, the psychological elements of dry eye shouldnt be dismissed, he says. At least one study has found that dry eye patients do have more psychological problems and disturbances, such as emotional instability and depression.5
But its so easy to pigeonhole these patients and say that they are attention-
15(S)-HETE. Alcons secretagogue 15(S)-HETE appears to stimulate secretion of MUC-1, a mucin that anchors the tear film to the epithelium. Clinical trials are ongoing.
INS365. Insp
ire Pharmaceuticals entry, also known as diquafosol, is an agonist of the P2Y2 receptor and is designed to promote secretion of aqueous, mucin and lipid components. Last year, Inspire submitted a new drug application to the FDA, based on phase II and phase III data, for a 2% preservative-free solution.

ASM981. Novartis is in phase II trials with a topical dry eye drop based on its Elidel (pimecrolimus) prescription skin cream for eczema. Pimecrolimus is a cell-selective inhibitor of inflammatory cytokines.
Topical drop. Postmenopausal women (particularly those with Sjgrens syndrome) and the elderly of either sex may be hormone deficient. This deficiency may lead to meibomian gland dysfunction, altered lipid profiles in meibomian gland secretions, tear film instability and evaporative dry eye. Allergan is in phase II trials with a topical androgen (testosterone) drop. Topical application of the hormone appears to alleviate dry eye signs and symptoms, and stimulate tear flow.
Transdermal cream. Charles Connor, O.D., Ph.D., director of research at Southern College of Optometry, has received a patent for a transdermal androgen cream (testosterone 3%) which is applied to the eyelid. Hes currently seeking a drug company to assume production. The vanishing cream, used bid, works best among aqueous-deficient women ages 40 to 60, Dr. Connor says, but it has almost no success in males. Patients with Sjgrens syndrome may need to apply it four times a day. One beneficial side effect that patients have noticed: It reduces wrinkles around the eye, he says.
seekers or have mental issues or whatever, Dr. Epstein says. I think thats a real serious mistake. Instead, it should get you thinking: What is causing the patients symptoms. Could this patient have no clinical signs yet have dry eye?
And that kind of thinking is upending the long-held view that dry eye is simply an aqueous or lipid deficiency, or a surfacing problem. Dr. Epstein says that researchers are changing their view of the three-layer tear filma concept thats from the middle of the last century. The tear film is no longer believed to be three discrete layers on top of one another like a sandwich; rather, parts of the layers overlap or interact. And, it may be that when combinations of certain elements from different layers are out of proportion, the imbalance can lead to different types of dry eye.
New thinking has also led to the notion of a neural feedback loop that controls tear and mucin production and incites inflammation. This inflammation not only damages the surface of the eye and lacrimal gland but also suppresses by any number of possible mechanismsthe production of tears.
Still, what does this mean to the average clinician or to the suffering patient? This kind of new thinking hasnt improved diagnosis of dry eye, and it has done very little to improve current management.
But Dr. Epstein thinks corneal sensitivity may eventually prove to be of some help. Some patients have significant corneal staining but report no discomfort, while other patients have far less staining but are more uncomfortable. He suspects that some patients experience more hypoesthesia from corneal surface damage than do others.
We dont do corneal sensitivity as part of the dry eye evaluation, and perhaps we should.
What else can asking the questionWhat about the patient who doesnt have any signs but yet has dry eye?tell us? In terms of management, very little.
Unfortunately, clinicians must revert to thinking of treatment in terms of the discrete three-layer tear film, Dr. Epstein says, because therapies havent yet caught up to the current level of thinking.
New therapies, such as immunomodulators that squelch the inflammatory processRestasis (cyclosporin, Allergan) is the first Rx dry eye medication in this classare on the horizon. (See Dry Eye Drugs in the Pipeline, above.) Meanwhile, careful and complete evaluationespecially with an ear to symptomatologymay be your most accurate and helpful instrument.
1. Begley CG, Chalmers RL, Abetz L, et al. The relationship between habitual patient-reported symptoms and clinical signs among patients with dry eye of varying severity. Invest Ophthalmol Vis Sci 2003 Nov;44(11):4753-61.
2. Nichols KK, Mitchell GL, Zadnik K. The repeatability of clinical measurements of dry eye. Cornea 2004 Apr;23(3):272-85.
3. Chalmers RL, Begley CG. Repeatability of habitual symptoms as measured by the dry eye questionnaire (DEQ). ARVO Abstract #3455, 2004.
4. Chalmers RL, Begley CG, Venkataraman K, et al. Grading dry eye severity: a comparison of clinician and self-assessment. ARVO Abstract #2463, 2003.
5. Erb C, Horn A, Gunthner A, et al. [Psychosomatic aspects of patients with primary keratoconjunctivitis sicca.] Klin Monatsbl Augenheilkd 1996 Feb;208(2):96-9.
6. Begley CG, Caffery B, Nichols KK, Chalmers R. Responses of contact lens wearers to a dry eye survey. Optom Vis Sci 2000 Jan;77(1):40-6.
7. Nichols KK, Nichols JJ, Zadnik K. Frequency of dry eye diagnostic test procedures used in various modes of ophthalmic practice. Cornea 2000 Jul;19(4):477-82.

