 |
Q:
I examined a uveitis patient with a concerning medical history in the early weeks of the COVID-19 crisis. Is there a link, and how aggressively should I be treating him?
A:
Jeff Gerson, OD, of Grin Eyecare in Kansas City, MO, saw a similar patient. A 40-year-old Asian male called the practice’s answering service, noting irritated eyes. He complained of a red left eye and a great deal of light sensitivity. He denied a fever, a cough and recent travel, so Dr. Gerson agreed to see him. Once in the exam room, the patient revealed a history of ankylosing spondylitis and previous bouts of red eye. His medications included vitamin D, albuterol and Cimzia (certolizumab pegol, UCB).
Clues in the Medicine
While reviewing his patient’s medical history, Dr. Gerson learned that the Cimzia his patient was on is a biologic categorized as a tumor necrosis factor–blocker that can lower the immune system’s ability to fight infections. “Similar to Humira (adalimumab injection, Abbvie), Cimzia is administered twice a month via injection for ankylosing spondylitis, as well as plaque psoriasis, rheumatoid arthritis and Crohn’s disease,” Dr. Gerson says. The patient had discontinued the medication on his own because he was afraid of contracting COVID-19 due to a potentially weakened immune system.
“If you are not familiar with a particular medication that your patient is on, look it up!” Dr. Gerson recommends. “A drug that you think may have nothing to do with their presenting signs and symptoms could be the key to unlocking the diagnostic door.”
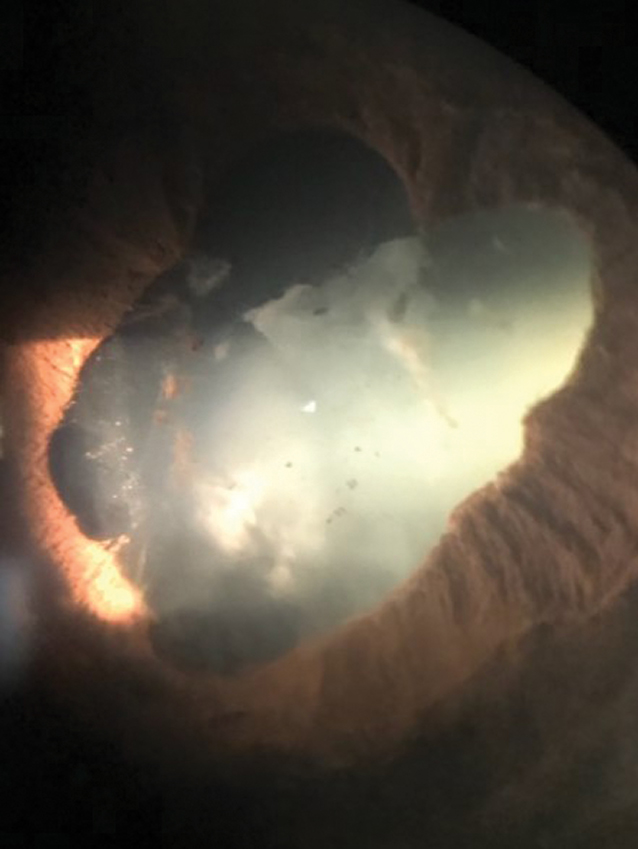 |
Fig. 1. Keep atropine and phenylephrine on hand to break synechiae aggressively in an anterior uveitis patient. Click image to enlarge. |
Another important point to take note of in this case is that ankylosing spondylitis often causes very severe anterior uveitis. Treat these types of cases extremely aggressively. It didn’t help the patient’s case that he stopped the medication that had kept the underlying systemic disease in check, even though he had experienced prior episodes on Cimzia.
Dr. Gerson says to start steroids immediately, with a preference for Durezol (difluprednate 0.05%, Novartis), when the iritis is raging. “I prescribed Durezol hourly, along with a steroid ointment at night for around-the-clock coverage,” he adds.
The synechiae were a major concern, so Dr. Gerson gave the patient a bottle of atropine 1% and phenylephrine 10% that he keeps in his “stash” for such an occasion. “Pharmacies don’t usually stock this, so keep some on hand to give to patients like this,” Dr. Gerson notes. He monitored intraocular pressure, which remained in the low teens.
Dr. Gerson saw the patient three days later and many of the synechiae had broken (Figure 1). With very slow tapering, and the patient back on Cimzia, this acute episode resolved slowly but steadily in a three- to four-week time frame. “Remember to lag your tapering way behind the improvement, so as not to risk a rebound,” advises Dr. Gerson.
Along with ocular treatment, Dr. Gerson had a discussion with the patient regarding his systemic condition. He encouraged the patient to return to the rheumatologist and ensure that he was back on the appropriate dosage of Cimzia, as well as for ongoing monitoring.
“With so many patients on biologics, and knowing that they reduce the immune response, double-checking their dosage is something worth considering in uveitis patients,” Dr. Gerson says. “Be curious about the drugs your patients are on, and treat intraocular inflammation with everything in your arsenal.”

