History
A 9-year-old black female presented for an eye examination complaining of itchy, irritated eyes. These symptoms had been bothering her for seven months.
Her ocular and systemic history was noncontributory.
Diagnostic Data
Her best uncorrected acuity was 20/20 O.U. at distance and near. External examination findings were normal with no evidence of afferent pupillary defect. The pertinent anterior segment findings are illustrated in the photograph.
Goldmann intraocular pressure measured 18mm Hg in both eyes. Dilated funduscopy of the periphery was within normal limits in both eyes. Both optic nerves had cup-to-disc ratios of 0.35 x 0.35.
Next Month in the Mag Feedback
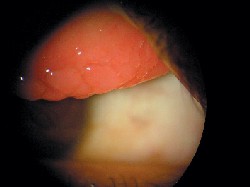
The patient presented with this clinical appearance.
Your Diagnosis
How would you approach this case? Does this patient require any additional tests?
What is your diagnosis? How would you manage this patient? What is the likely prognosis?
Diagnosis
The diagnosis in this issue is giant papillary vernal conjunctivitis. Additional testing might include checking the cornea for sodium fluorescein staining and ruling out the presence of lymphadenopathy (to rule out viral etiology).
The clinical presentation of vernal conjunctivitis is chronic bilateral inflammation of the superior and limbal palpebral conjunctiva. Its prevalence is higher in warmer climates, with an onset between the ages of 3 and 25 years. Males are typically more affected than females.1-5 Patient symptomatology often includes itching with thick ropy discharge. In most cases a history of allergies (seasonal or other) or infantile eczema can be elicited.1-6
The important observable clinical signs include large conjunctival papillae on the back of the superior tarsus; raised, gelatinous, white clumps of degenerated eosinophils at the superior limbus (called Horner-Trantas dots); areas of superficial punctate keratitis (SPK); and in severe cases, well demarcated, sterile, superior, corneal shield ulcers.1-5
VKC can be differentiated from atopic keratoconjunctivitis (AKC) based upon age, location, dermatitis and lack of seasonal variability.6Allergic responses are classically considered an over-reaction of the bodys immune system to immunogens or allergens.1-3 The response can be innate or acquired. The key component of the vernal ocular allergic response is the eosinophil.
Vernal conjunctivitis is IgE-mediated and the only ocular disease to involve solely Type I hypersensativity.5 Involvement of secondary inflammatory cells, particularly eosinophils (in addition to mast cells) resident to the substantia propria of the superior tarsus can produce vision threatening sequelae. Under high magnification, papillae with epithelial downgrowth form crypts, at the base of which lie mucous-producing goblet cells. Plasma cells and lymphocytes collect inside papillae stroma. Vernal shield ulcers develop in the upper regions of the cornea. The base of the ulcer is composed of abnormal mucous, fibrin and serum, deposited as a gray plaque.3 Friction, secondary to the roughened superior conjunctiva, erodes the corneal epithelium.
Vernal conjunctivitis management is primarily aimed at reducing symptomatology and preventing serious vision threatening sequelae. Perhaps the most effective treatment is the elimination or avoidance of the allergen. Cold compresses and artificial tears and ointments soothe and lubricate on an as needed basis. Topical decongestants (naphazoline, phenylephrine, etc.) produce vasoconstriction, reducing hyperemia, chemosis and other symptoms by retarding the release of the chemical mediators into the tissues from the blood stream.
The following are better therapies than topical decongestants, and all can be used before the disease flares up or to keep it under control following acute treatment
Topical antihistamines such as Emadine (emedastine, Alcon) and Livostin (levocabastine, Novartis).
Topical antihistamine/mast cell stabilizer combinations such as Elestat (epinastine, Allergan), Optivar (azelastine, Bausch & Lomb), Patanol (olopatadine, Alcon), Zaditor (ketotifen, Novartis) b.i.d.-q.i.d.7.
Mast cell stabilizers such as Alamast (pemirolast, Vistakon), Alocril (nedocromil, Allergan), Alomide (lodoxamide, Alcon), Crolom (cromolyn sodium, Bausch & Lomb) and Opticrom (cromolyn sodium, Allergan)
Oral antihistamines such as Benadryl (diphenhydramine Pfizer] 25mgs, t.i.d. p.o.)
The non-steroidal anti-inflammatory drugs (NSAIDs) such as Acular LS (ketorolac, Allergan) and Voltaren (diclofenac, Novartis) b.i.d.-q.i.d., and the topical steroids Alrex (loteprednol 0.2%, Bausch & Lomb), Lotomax (loteprednol 0.4%, Bausch & Lomb) and Pred Mild (prednisolone acetate 0.12 %, Allergan ) may offer relief in moderate cases.
Reserve stronger topical steroidal preparations such as Pred Forte (prednisolone acetate, Allergan), Inflamase Forte (prednisolone sodium, Novartis), Lotemax (loteprednol 0.5%, Bausch & Lomb), Vexol (rimexolone, Alcon), FML (fluorometholone alcohol, Allergan), and Fluor-Op (fluorometholone alcohol, Novartis) b.i.d.-q.i.d. for the more severe presentations.
Patients who present with shield ulcers should be additionally managed with aggressive cycloplegia (atropine 1%, homatropine 5%, scopalomine 0.25 %, b.i.d.), topical antibiotic drops (tobramycin, ciprofloxacin, ofloxacin, trimethoprim/polymyxin) to cover, and topical steroids (even though the etiology is mechanical) to reduce the underlying superior palpebral conjunctival papillary cause. Also consider prescribing the mucolytic acetylcysteine (Mucomyst 10% or 20%, Geneva) q4-6h. In any case where foreign body sensation produces symptoms or signs, whether there is an ulceration or not, a low water content, hydrogel lens may be used to reduce the interaction between the lid and cornea.
Educate patients with a history of seasonal allergic conjunctivitis to avoid the deleterious substances that precipitate symptoms. In chronically occurring cases, patients may be treated in advance with loading doses of topical mast cell stabilizers or combination preparations, b.i.d. to q.i.d. to attempt to retard the degranulation process and momentum of beginning symptoms. If effective, this therapy should be maintained for the duration of the season and repeated before each period.
Patients placed on supportive therapies (tears, cold compress) may be followed on an as needed basis. Patients placed on topical medications should be followed at 1 week, with close monitoring thereafter. Patients placed on topical steroids should undergo periodic IOP measurement. Patients treated for shield ulceration should be followed every 1-3 days.1
1. Cullom RD, Chang B. Conjunctiva/Sclera/External Disease: Allergic Conjunctivitis. In: Cullom RD, Chang B. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. Philadelphia: J.B. Lippincott Co. 1994;112-13.
2. Cetinkaya A, Akova YA, Dursun D, Pelit A. Topical cyclosporine in the management of shield ulcers. Cornea 2004 Mar;23(2):194-200.
3. Hunter PA, Watson PG. Allergic Eye Diseases: Episcleritis and Scleritis. In: Spalton DJ, Hitchings RA, Hunter PA. Atlas of Clinical Ophthalmology. Philadelphia: Lippincott 1984:5.1-5.22.
4. Hunt L. Allergic conjunctivitis disorders. Insight 1995;20(2):25-26.
5. Foster CS. The pathophysiology of ocular allergy: Current thinking. Allergy 1995;50(21 suppl.):6-9, 34-38.
6. Marren SE. Allergy. In: Blaustein BH. Ocular Manifestations of Systemic Disease. New York: Churchill Livingstone 1994:243-55.
7. Goes F, Blockhuys S, Janssens M. Levocabastine eye drops in the treatment of vernal conjunctivitis. Doctrine of Ophthalmology 1994 ; 87 ( 3 ) : 271 - 81.
Thanks to Charlene Maloney, O.D., for contributing this case.
5th Annual Presbyopia Report. As the presbyopic population is expanding, so is the range of options available for these patients. Optometrist Paul M. Karpecki looks at the latest research into surgical treatments for presbyopia, including conductive keratoplasty and accommodating IOLs. Also included: contact lenses and progressive lens options for presbyopic patients.
New Drugs in the Pipeline. Learn about the most recently approved and soon-to-be-released ophthalmic drugs, such as the latest glaucoma combination drugs, the forthcoming Rx dry eye meds and potential neuroprotectors. Plus, well take a peek at some astounding preliminary research of drugs a long way out.
Make the Most of Internal Communication. This article offers practical tips you can use to maximize in-office communication and to promote organization. These include using an internal Internet system, a practice post office, and multi-colored light fixtures to indicate which exams rooms are in use.
Ocular Warnings of Systemic Disease. Sometimes the so-called routine eye exam is anything but routine when you are the first to discover signs of a serious systemic illness. Optometrist Evan Canellos conducts grand rounds, including cases of leukemia diagnosed through an eye exam, a post-op corneal melt in a patient with rheumatoid arthritis, and an asymptomatic pituitary adenoma diagnosed from an eye exam.
Review of Optometry welcomes questions and comments. Contact Amy Black, editor-in-chief, ablack@jobson.com with Letter to the Editor as the subject line. Or, write to Review of Optometry, 11 Campus Blvd., Suite 100, Newtown Square, PA 19073.

