 |
Optometrist A.M. Skeffington once postulated that, “The near-work demands imposed upon our culture are incompatible with our physiology and provoke a stress response.”1 Over time, the human body set up a system to reduce the impact of visual stress: buffers. Buffers allow us to resist stress and come away unharmed by those same stressors.2 Without the presence of buffers, we would experience symptoms almost as soon as stressors are encountered, and if their duration or intensity continues for too long, changes in structure would occur.
Low hyperopia and exophoria are the body’s ocular buffers and should be encouraged, not viewed as detriments. As Leo Manas, OD, put it, “The presence of orthophoria is undesirable, and remedial measures should be instituted to regain the buffer of exophoria as soon as possible.”3 The cases below demonstrate how to keep your patients on the desired exophoria path during the prescribing process.
Case 1
|
|
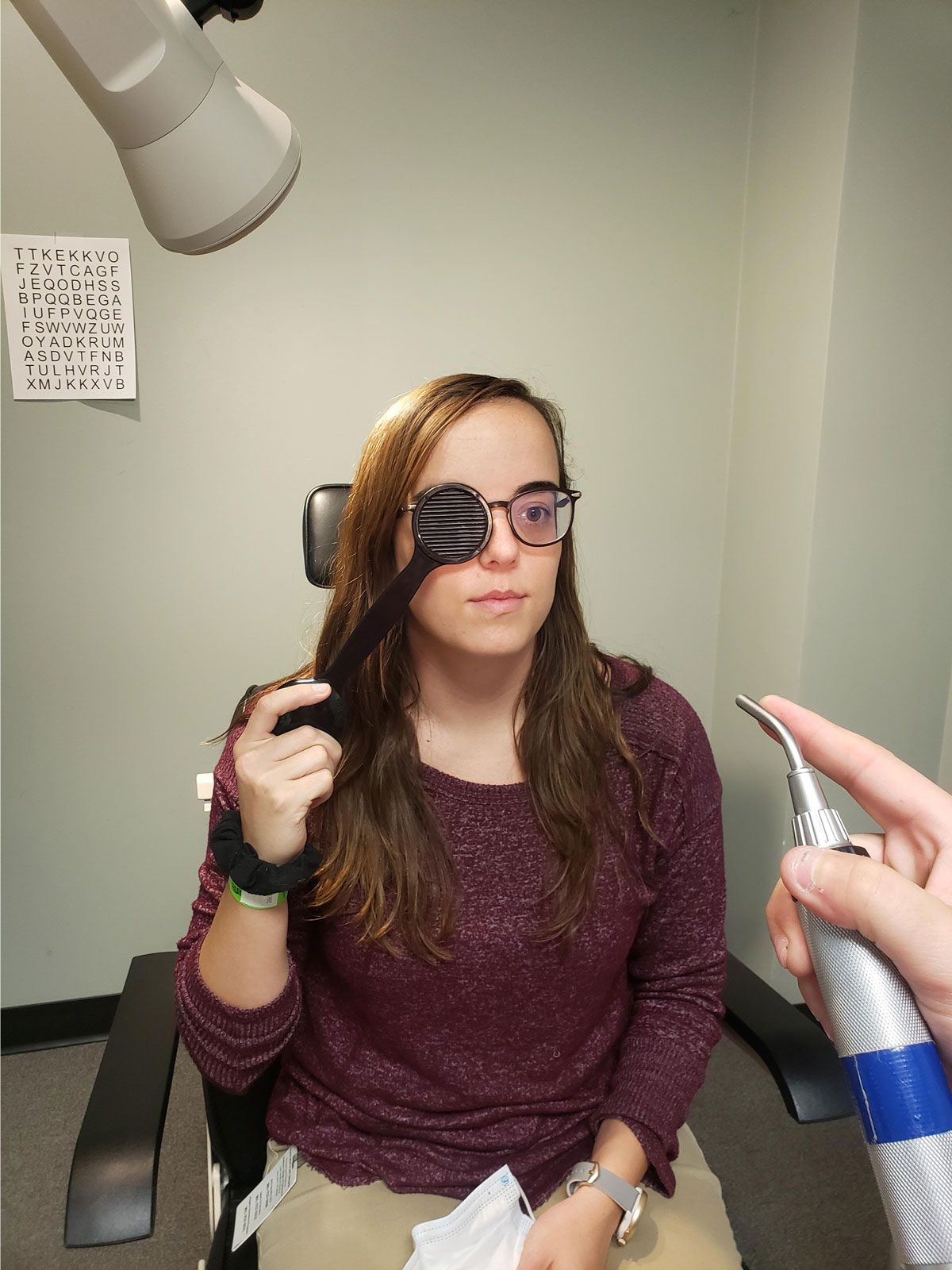
Use a Maddox rod to determine a patient’s phoria. Click image to enlarge. |
A 10-year-old female patient presented complaining of distance blur with her glasses, which were -1.50-0.50x180 OD and -1.50 OS. Her acuities were 20/25- OD, 20/30 OS and 20/25 OU at distance and 20/20 OD, OS and OU at near.
Stereopsis yielded 20 seconds of arc using the Randot Stereo Test. Near point data, including the near point of convergence and accommodative amplitude, fell within expected values. However, the cover test stood out, showing orthophoria at distance and four esophoria at near with glasses.
A new prescription of -2.00 OU improved the patient’s acuities to 20/20 OD, OS and OU. Negative and positive relative accommodations were balanced at +2.50/-2.50, and the fused cross-cylinder test showed +1.00 (higher than the expected +0.50). The vergence ranges showed an imbalance at near (base-in x/16/8, base-out x/32/20). The cover test remained four esophoria at near.
While the patient’s numbers did not line up with its textbook definition, convergence excess was deemed the appropriate diagnosis.
The patient’s degree of esophoria indicated that we needed to help her reestablish exophoria. The first step was plus lenses in the form of a bifocal. Given that the expected average accommodative convergence/accommodation ratio is four to one and that convergence excess is associated with a higher-than-average ratio, we trial-framed +1.00 over the new distance prescription. We were pleased to find the near cover test at two exophoria.
The final prescription was -2.00 OU with a +1.00 bifocal. While some practitioners set the segment height higher to ensure the patient takes advantage of the add, we decided, based on the patient’s maturity, that a traditional height would suffice. A progressive, or stress-relieving, lens design was not discussed but is not out of the question for those who prefer a no-line option.
We will evaluate the patient again after six to eight weeks of new lens wear and consider vision therapy.
Case 2
|
|
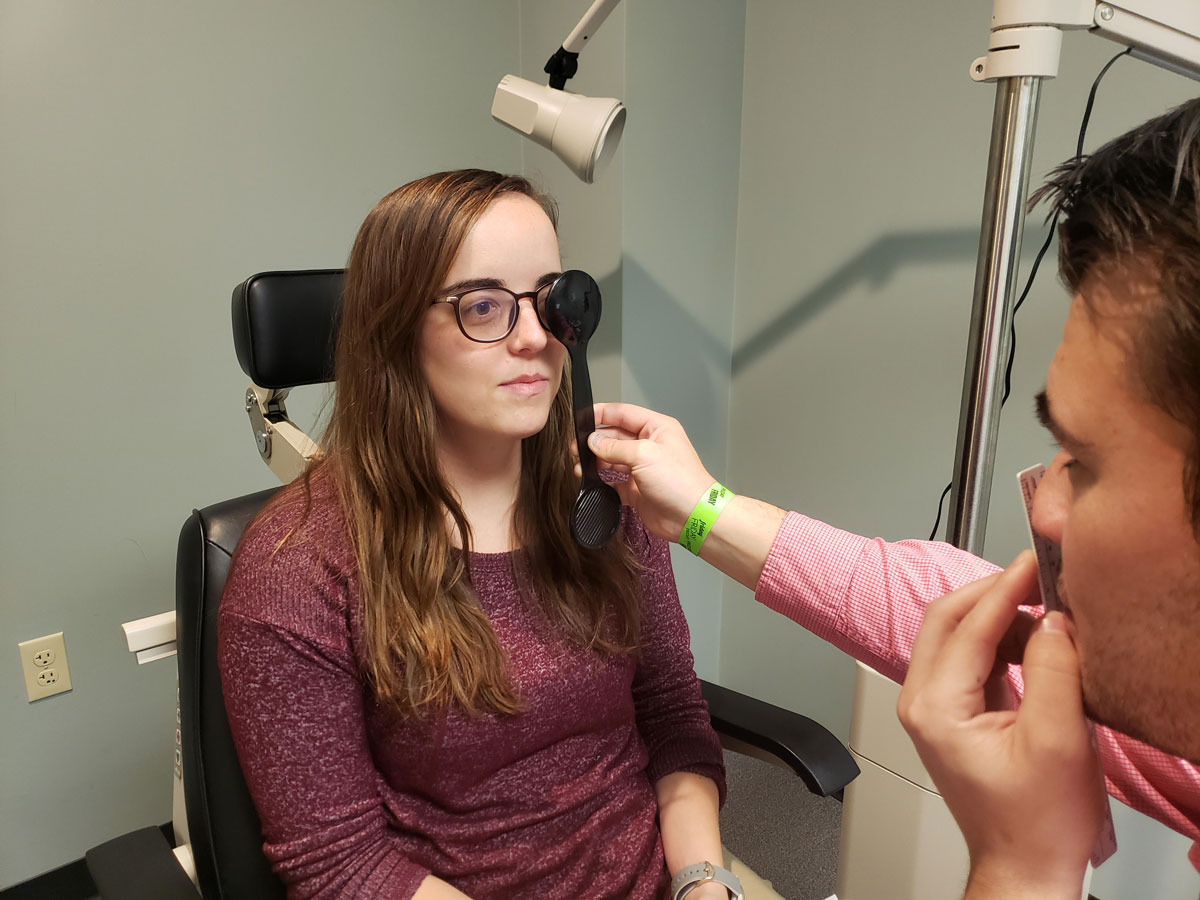
This patient is undergoing near cover testing. Click image to enlarge. |
A 13-year-old female patient presented complaining of asthenopia at near, especially with increased computer work during virtual schooling. Her uncorrected visual acuities were 20/20 OD, 20/25 OS and 20/25 OU at distance and 20/25 OU at near. She had been prescribed glasses with a prescription of -0.75-0.75x180 OD and -1.00 OS at an eye exam four weeks prior but did not see a difference in clarity and stopped using them.
She demonstrated a stereopsis of 50 seconds of arc. Cover testing showed six esophoria at distance and near. Her retinoscopy showed +2.00 OU, which reduced her acuities to 20/50 OD and OS. Her refraction was +1.00 OU, which resulted in visual acuities of 20/20 OD, OS and OU.
With a trial frame, cover testing was two esophoria at distance and near. With the goal of reducing the eye turn as much as possible to support the natural buffer, we trialed extra plus at near and determined +1.00 OU to be the “best bang for the buck.” With the new prescription, cover testing showed two exophoria at near.
|
|
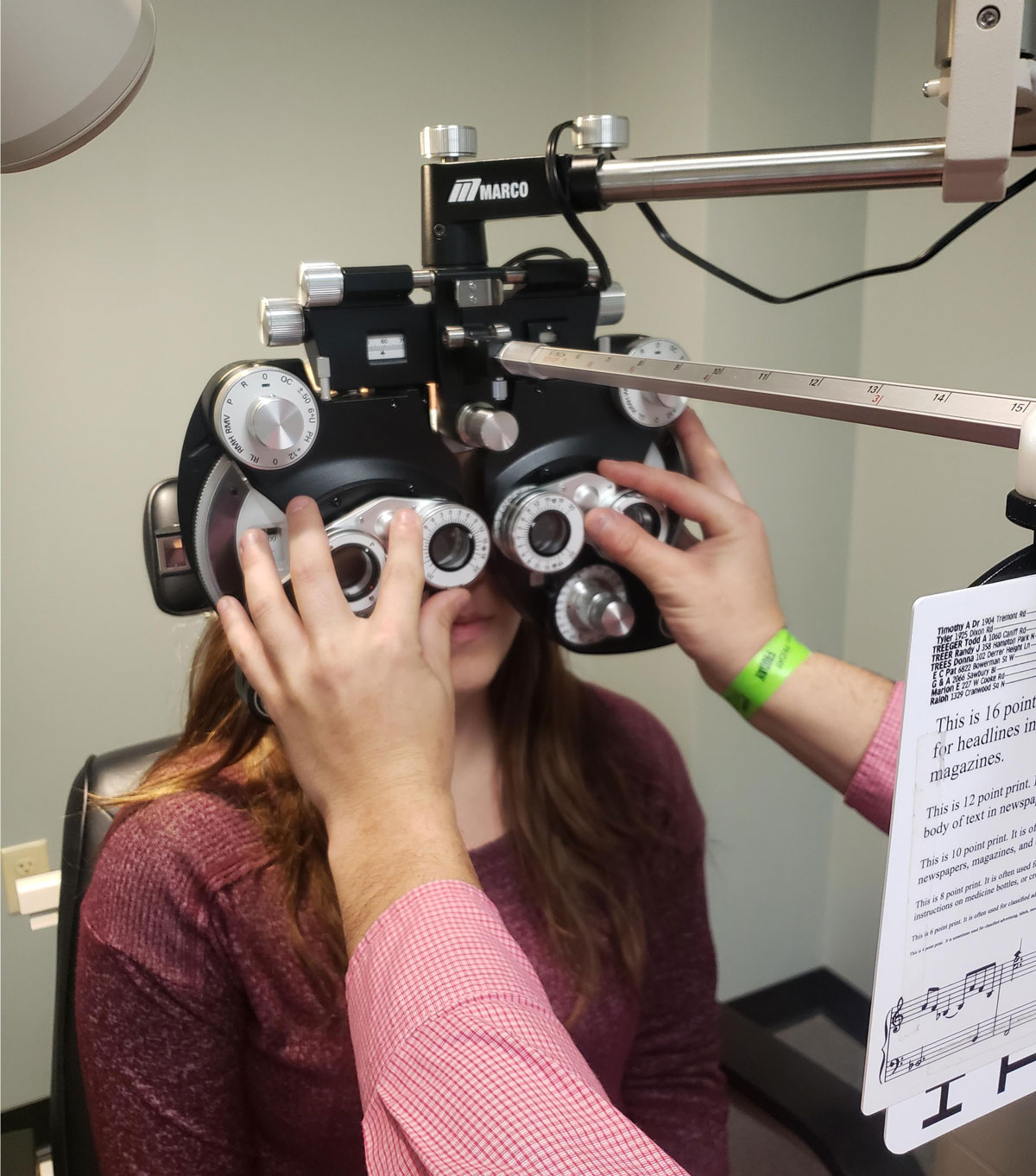
A phoropter is also helpful in measuring the phoria. Click image to enlarge. |
The patient was prescribed +1.00 OU with a +1.00 bifocal for full-time use and was scheduled to come back in four to six weeks for a complete accommodative and binocular vision workup. At that point, we will consider vision therapy to further encourage the patient to actively solidify her buffer for long-term success.
While the two patients described here are very different, we were able to use plus to help each of them restore their exophoric buffer in each case.
Prescribing lenses is a passive treatment. In some cases, it is sufficient enough to nudge the patient in the right direction. In many cases, though, vision therapy can build on the lenses and complete the process of preventing the visual system from building a higher exophoria at near (convergence insufficiency) and halting the buffer from reducing even further into orthophoria or esophoria (convergence excess).
1. Birnbaum MH. Optometric Management of Nearpoint Vision Disorders. Boston: Butterworth-Heinemann, 1993:33. 2. Selye H. The Stress of Life. New York: McGraw-Hill, 1976. 3. Manas L. Visual Analysis. Santa Ana, CA: Optometric Extension Program Foundation, 2009:14. |

