 |
An 81-year-old white male presented with acute diplopia, which he noted upon awakening. He reported it as constant, horizontal and worse when looking to the right. Pertinent medical history included hypertension and arrhythmia. Medications included Toprol (Astra Zeneca), Lasix (Sanofi Aventis), potassium and aspirin 81mg. He also had a pacemaker.
Best corrected visual acuities were 20/25 and 20/30 OD, OS. Pupils were round, equal and reactive to light. Intraocular pressures were normal at 15mm Hg in each eye. Extraocular motility testing revealed an adduction deficit in the left eye, with contralateral abducting nystagmus when the patient looked to his right. Anterior and posterior segment exams were unremarkable. There was no disc edema noted in either eye.
We diagnosed our patient with an acute left internuclear ophthalmoplegia (INO). Given his age and acute onset, the most likely etiology was ischemia. The patient was transported to the emergency room following our recommendation for neuroimaging. MRI was contraindicated because of his pacemaker. A CT was ordered, but failed to show any acute brainstem ischemia. CTA of the head and neck was also ordered, which did not show any significant stenosis.
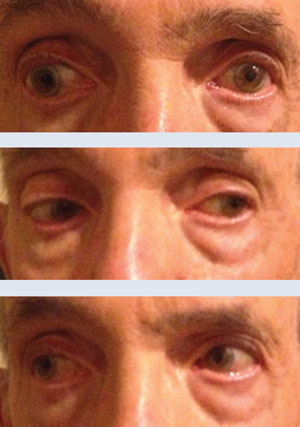 | |
| At top and center, this patient showed INO when looking to the right, normal motility when looking to the left. In the bottom photo, the patient showed an 80% improvement seven days later on follow up. |
The patient was admitted under observation for 48 hours and discharged. He returned to our clinic one week later, subsequent to evaluation by his internist and cardiologist, who increased the patient’s aspirin to 325mg and started atorvastatin. The patient reported that his diplopia had improved significantly. The adduction deficit improved about 80% subsequent to our initial examination. Although our suspicion for myasthenia was low, his normal neuroimgaing and failure to show any ischemia or stenosis prompted us to order myasthenia labs just to rule out a masquerading syndrome—results were normal. Our patient followed up one month later with complete resolution of the INO and was doing very well as of his last visit.
Discussion
Internuclear ophthalmoplegia is a localizing neuro-ophthalmic disorder caused by a disruption of the medial longitudinal fasciculus (MLF). The abducens nucleus contains two groups of neurons: (1) motoneurons that innervate the ipsilateral lateral rectus (LR) and (2) internuclear neurons that innervate the contralateral medial rectus (MR) motor neurons via the MLF.1 Lesions that disrupt the MLF will give rise to an ipsilateral adduction deficit. The deficit can range from a decrease in velocity of adduction to a complete loss. In addition to an ipsilateral adduction deficit, there is often a contralateral abduction nystagmus noted. One explanation for the nystagmus is an adaptive response to overcome the weakness of the medial rectus muscle.2
A particular variation of INO termed “one-and-a-half syndrome” occurs when a lesion disrupts the abducens nucleus or the paramedian pontine reticular formation as well as the MLF.1,3 This results in an ipsilateral gaze palsy and an INO.
Historically, patients with INO will present noting horizontal diplopia. A skew deviation can sometimes be present with INO, so there may be a vertical component as well.1,3 Convergence is spared in internuclear ophthalmoplegia unless the lesion is also close to the third nerve nucleus.3 The main causes of INO are demyelination (typically bilateral INO and seen in younger patients) and ischemia (typically unilateral and seen in older individuals).1,4,5 Less common causes of INO include trauma, tentorial herniation, infection, tumor, hemorrhage and vasculitis.4
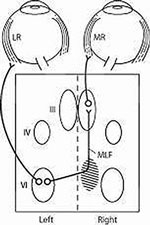 | |
| The MLF connects internuclear neurons of the sixth nerve nucleus to the contralateral medial rectus subnucleus. |
Given our patient’s age and our expectation of an acute ischemic etiology, emergent neuroimaging was warranted. The preferred imaging modality is MRI unless contraindicated, which was the case for this patient. Although CT imaging was negative, this did not exclude the diagnosis of INO. In one study, 11 patients with INO underwent MRI, which showed focal or nodular areas of high signal intensity on T2-weighted images in the region of the MLF in 10 of 11 patients.6 Nine of these 11 patients also underwent CT scan, which failed to show lesions in any patient.6
Management of internuclear ophthalmoplegia includes appropriate referrals, depending on the underlying etiology. In cases of ischemic internuclear ophthalmoplegia, patients are typically followed monthly until there is resolution of the palsy.
1. Miller, Neil R, et al. Clinical Neuro-Ophthalmology: The Essentials, 2nd edition. Lippincott Williams & Wilkins; 1999.2. Zee, DS. Internuclear ophthalmoplegia: pathophysiology and diagnosis. Bailliéres Clin Neurol. 1992 Aug;1(2):455-70.
3. Liu, GT, et al. Neuro-Ophthalmology Diagnosis and Management. W.B. Saunders Company; 2001.
4. Keane, JR. Internuclear ophthalmoplegia: unusual cases in 114 of 410 Patients. Arch Neurol. 2005;62:714-17.
5. Rizzo, JL. Pediatric internuclear ophthalmoplegia. J Neuro-Ophthalmol. 2014;33:134.
6. Atlas SW. Internuclear ophthalmoplegia: MR-anatomic correlation. AJNR Am J Neuroradiol. 1987 Mar-Apr;8(2):243.

