Dioptin Eye Drop for Presbyopia Studies Move Forward
Distance-corrected near visual acuity gains show the potential of this new method of correction.
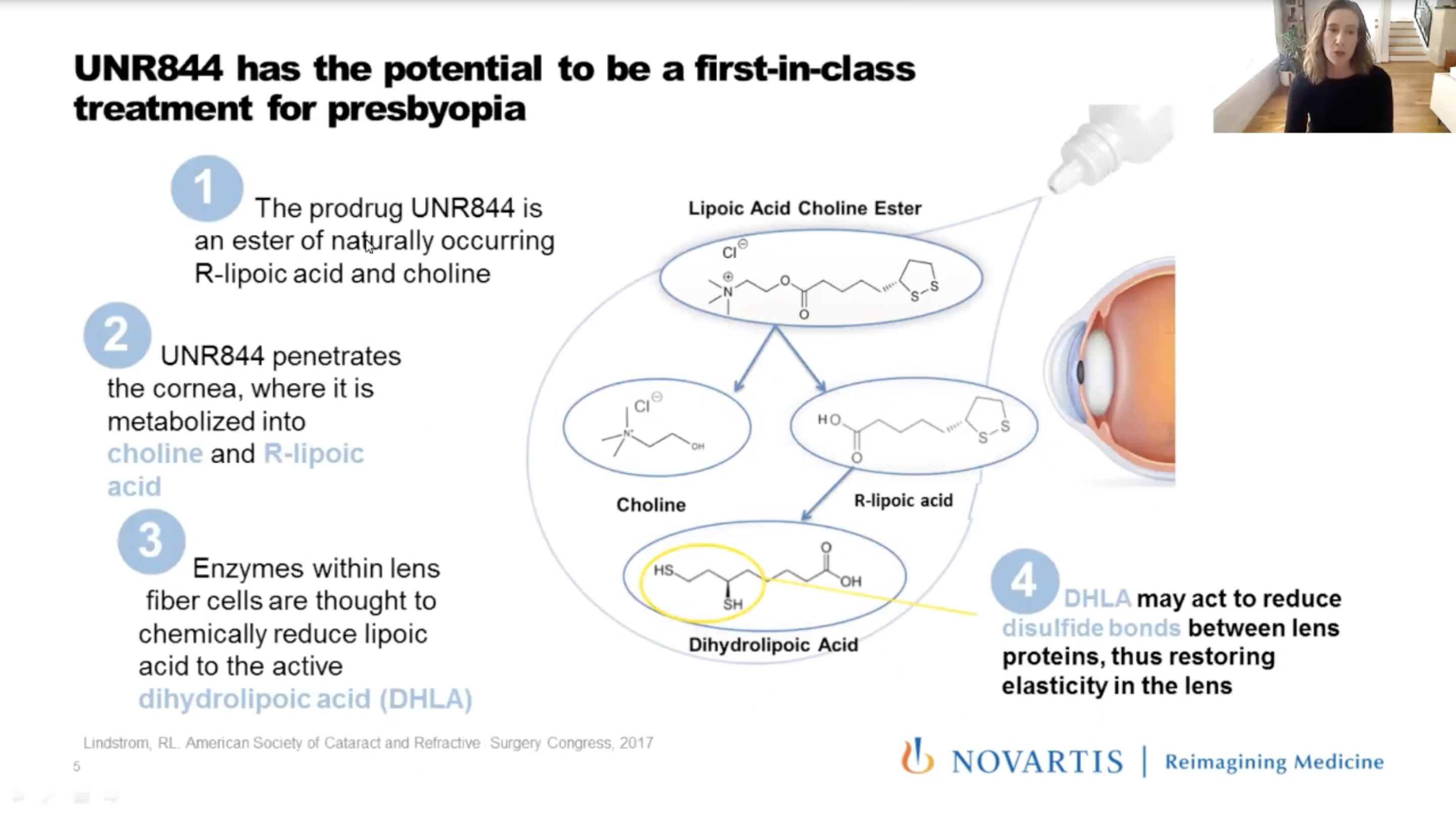
The Phase I/II results of the topical eye drop Dioptin (UNR844, Novartis) were presented by Kathryn Richdale, OD, PhD, of the University of Houston College of Optometry. The eye drop is a lipoic acid-based, topically instilled prodrug that penetrates the cornea. Enzymes metabolized by the crystalline lens help reduce disulfide bonds between proteins and restore elasticity. According to Dr. Richdale, increasing lens protein disulfide content may cause presbyopia through a loss of lens elasticity.
The ophthalmic solution showed a five-letter improvement in distance-corrected near visual acuity (DCVNA) vs. placebo, with treatment benefit observed up to seven months in observational follow-up. The prospective, randomized, double-masked, multicenter Phase IIa study analyzed male and female subjects aged 45 to 65 years old who had DCNVA in each eye and binocularly <70 ETDRS letters (20/40) at 40cm and who needed a minimum add of +1.00D or greater to achieve binocular DCNVA of at least 85 ETDRS letters (20/20.
Subjects were randomized 1:1 to receive 1.5% Dioptin (n=40) or placebo drops (n=38) in each eye, twice a day for three months. There was no significant difference in mean change in DCNVA between Dioptin and placebo, (difference of 1.6 letters), so the primary objective was not met. Due to high variability in DCNVA measures in both groups, but to a greater extent in the placebo arm, the researchers performed a post-hoc non-parametric analysis.
The median difference between Dioptin and placebo was four letters closer to the Phase I/II study results, and further clinical development is planned in a Phase IIb dose-finding study. Still, the study noted that future studies should also include mitigation strategies to minimize DCNVA variability. Research is still ongoing to better understand efficacy. Nevertheless, Dr. Richdale states that there is an unmet need for pharmacological treatments in presbyopia.
 |
The above summary was presented at the Academy press conference on October 7. Dr. Richdale will give a full presentation in this session:
P-04: Papers: Novel Pharmaceutical Treatments, Friday, October 9, 11-11:15am
COVID Fears Weigh Heavily on Eye Care Community
Outdoor activities, family time and exercise have helped practitioners, staff and students improve stress levels.
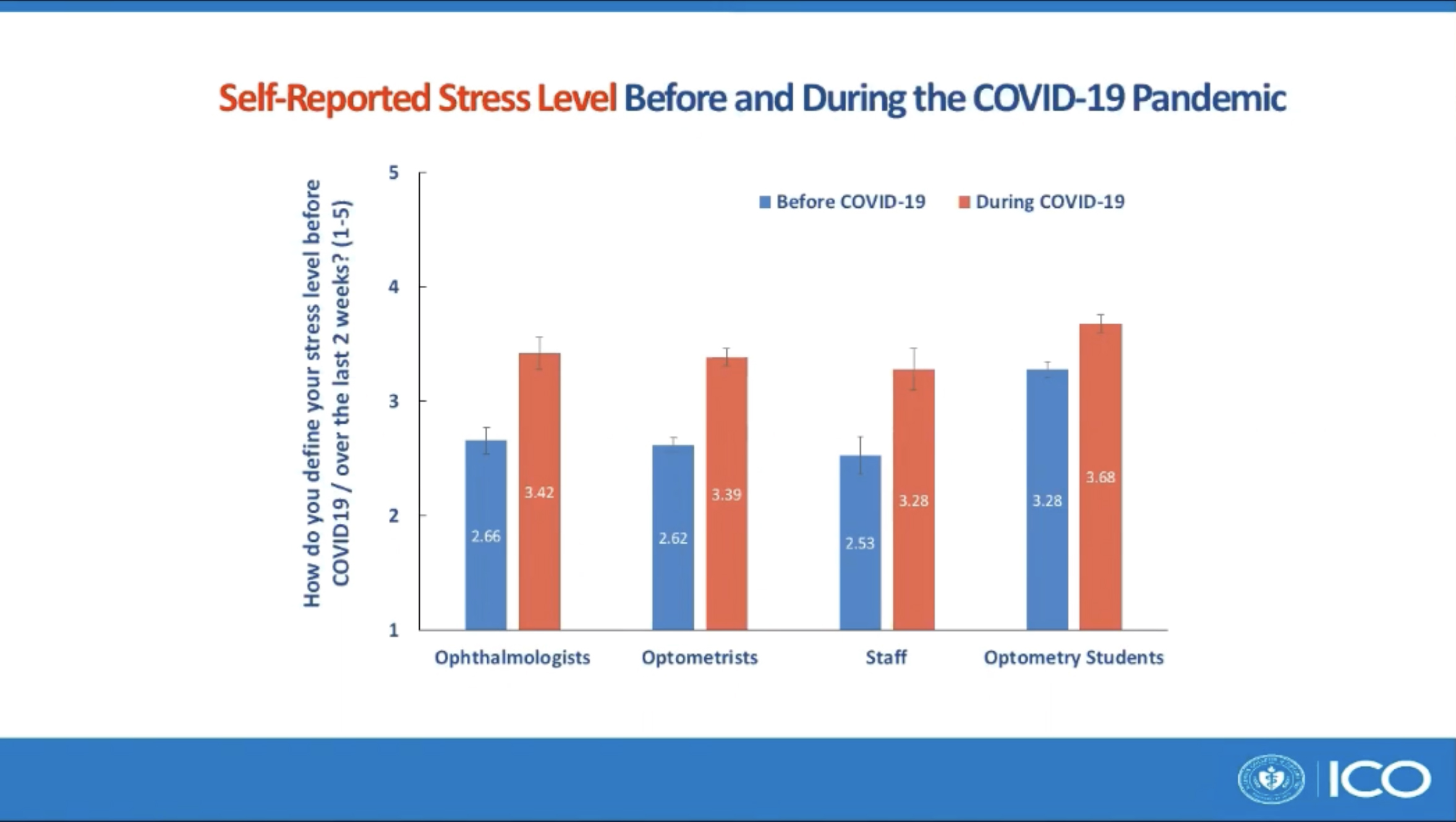
A recent survey has demonstrated the impact that COVID-19 and its consequent challenges have had on the mental health of eye care practitioners, staff and optometry students. More than 60% of professionals and students reported that their mental health was worsening during the pandemic, and almost 40% reported symptoms of anxiety, depression or both during the pandemic. Researchers identified the top three factors that have negatively impacted mental health: (1) worries about family/friends being infected with COVID-19, (2) self-worry about being infected with COVID-19 and (3) social isolation. Study authors Yi Pang, OD, PhD, FAAO, professor at the Illinois College of Optometry, and her student Connor Robbs, BS, also noted that outdoor activities, family time and exercise positively impacted mental health.
A 22-question survey was sent through social media and email to ophthalmologists, optometrists, staff and optometry students. The researchers collected data on demographics, stress level before and with COVID-19 (the last two weeks of data collected), positive and negative factors which impacted mental health by COVID-19 and screening questions for depression and anxiety. A total of 1,558 individuals (29.9% male and 69.2% female) from 49 US states (n=1,431)and Canada (n=127) responded to the survey, including 617 optometrists, 610 optometry students, 197 ophthalmologists and 134 eye care staff.
Of the participants, 61.2% stated that COVID-19 had a negative impact on their mental health vs. 25.6% stating no impact and 13.2% stating a positive impact. The mean self-reported stress level increased significantly from 2.90 out of 5 before COVID-19 to 3.50 out of 5 with COVID-19. Before COVID-19, only 6.6% of the participants scored themselves at the highest stress level, which then increased to 21.9% with COVID-19. The study also noted that 21% of participants failed the depression screening questions and 34.7% failed the anxiety screening questions. Mr. Robbs noted that optometry students self-reported the highest stress levels before and during the pandemic among all groups.
Dr. Pang identified being a student, female, younger, Asian as well as the number of new daily COVID-19 cases in the state as risk factors for mental health disorders during the pandemic. Protective factors included more frequent interactions with patients and having a greater proportion of childcare responsibilities at home. “COVID-19 has had a negative mental health impact on two-thirds of those surveyed eye care practitioners, staff and optometry students, with self-reported stress levels having increased significantly,” Dr. Pang concluded.
 |
The above summary was presented at the Academy press conference on October 7. Dr. Pang and Mr. Robbs will give a full presentation in this session:
POS-01: Posters: Public Health/Health Care Delivery, Wednesday, October 7, 3-5pm
Wireless Telemetry Reveals Pressure-based Risk Factors
While IOP is the most readily measurable variable, others demonstrate a more comprehensive view.
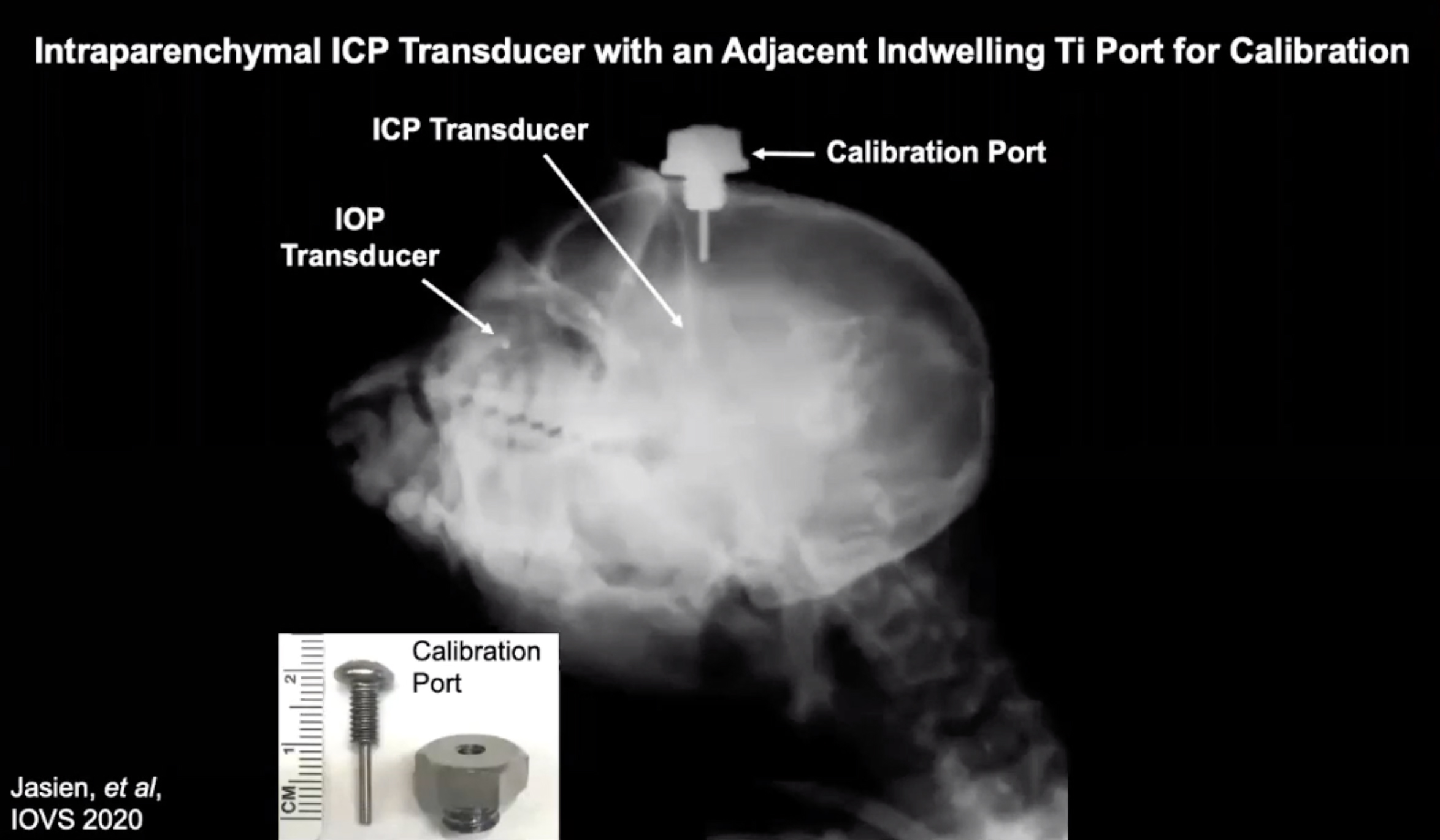
Researchers at the University of Alabama have developed an implantable wireless pressure telemetry system to help determine continuous and accurate measurements of intraocular pressure (IOP) and cerebrospinal fluid pressure (CSFP), which are important for glaucoma pathogenesis, and also assess lamina cribrosa thickness and the translaminar pressure gradient. The team measured unilateral IOP from the anterior chamber and intracranial pressure (ICP) from the brain parenchyma (as a surrogate measure of CSFP) in nonhuman primates (NHPs). Jessica Jasien, PhD, presented the team’s results yesterday.
The device measured IOP, ICP and blood pressure at 200Hz for 15s every two and a half minutes for 24 hours a day over a range of 69 to 281 days. The study collected IOP and ICP data in three male rhesus macaques on a 10% duty cycle, consisting of 200 measurements per second. While one subject had the lowest IOP and ICP in all periods, it had the highest translaminar pressure gradient in all periods due to its relatively thin lamina cribrosa. The team observed similar shifts in the rank order of possible glaucoma risk factors for the other two NHPs as well.
Dr. Jasien concluded that even though IOP is the only modifiable and readily measurable pressure-based risk factor for glaucoma, other potential risk factors exist and their rank order patterns may differ compared to IOP across subjects. Therefore, a comprehensive view of relevant risk factors is warranted.
 |
The above summary was presented at the Academy press conference on October 7. Dr. Jasien will give a full presentation in this session:
P-11: Papers: Glaucoma: New Evidence to Enhance our Understanding of the Disease, Saturday, October 10, 2-2:15pm
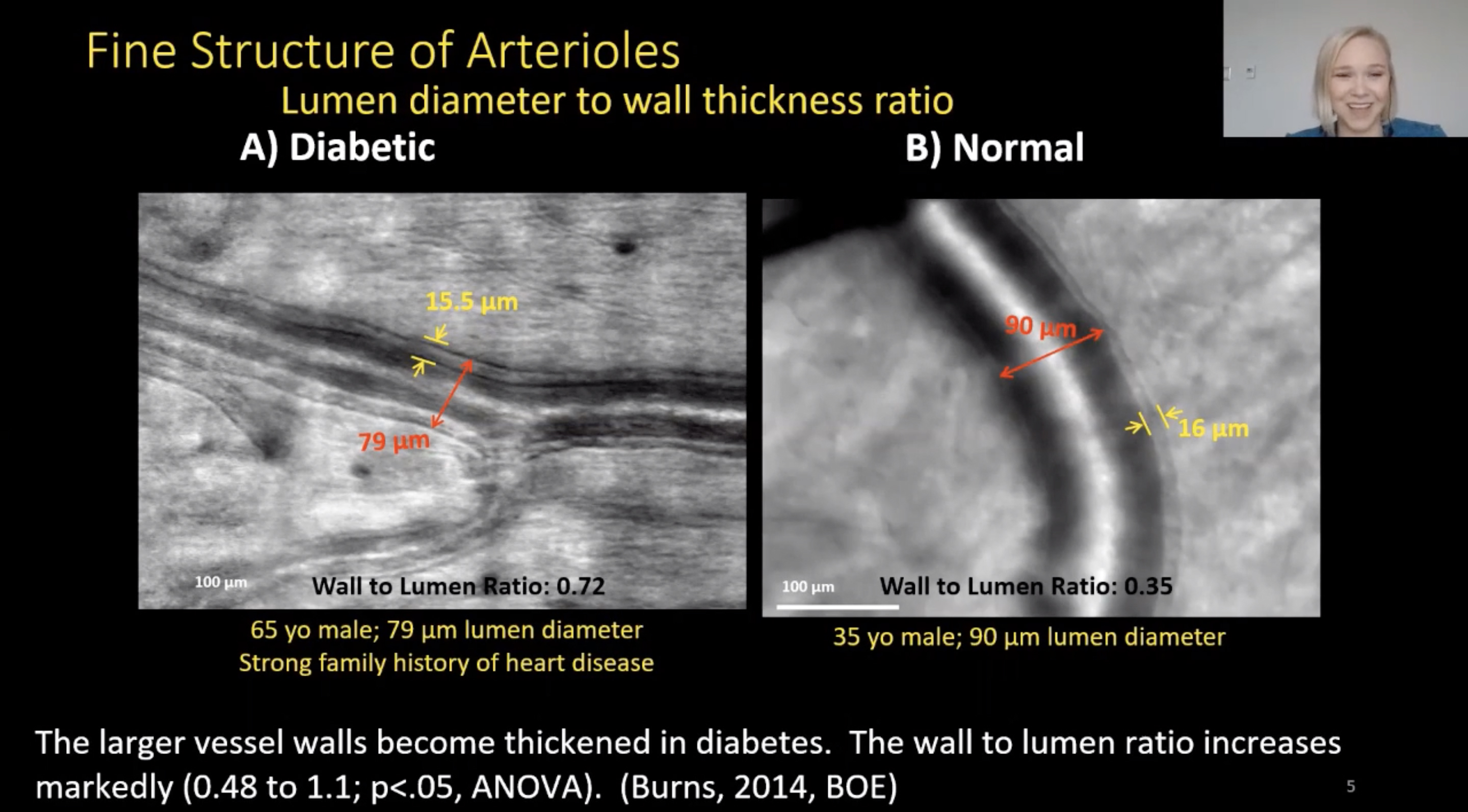
Look for Thickened Arteriole Walls in Small Vessels of DR Patients
High-res imaging finds significant alterations in retinal vasculature.
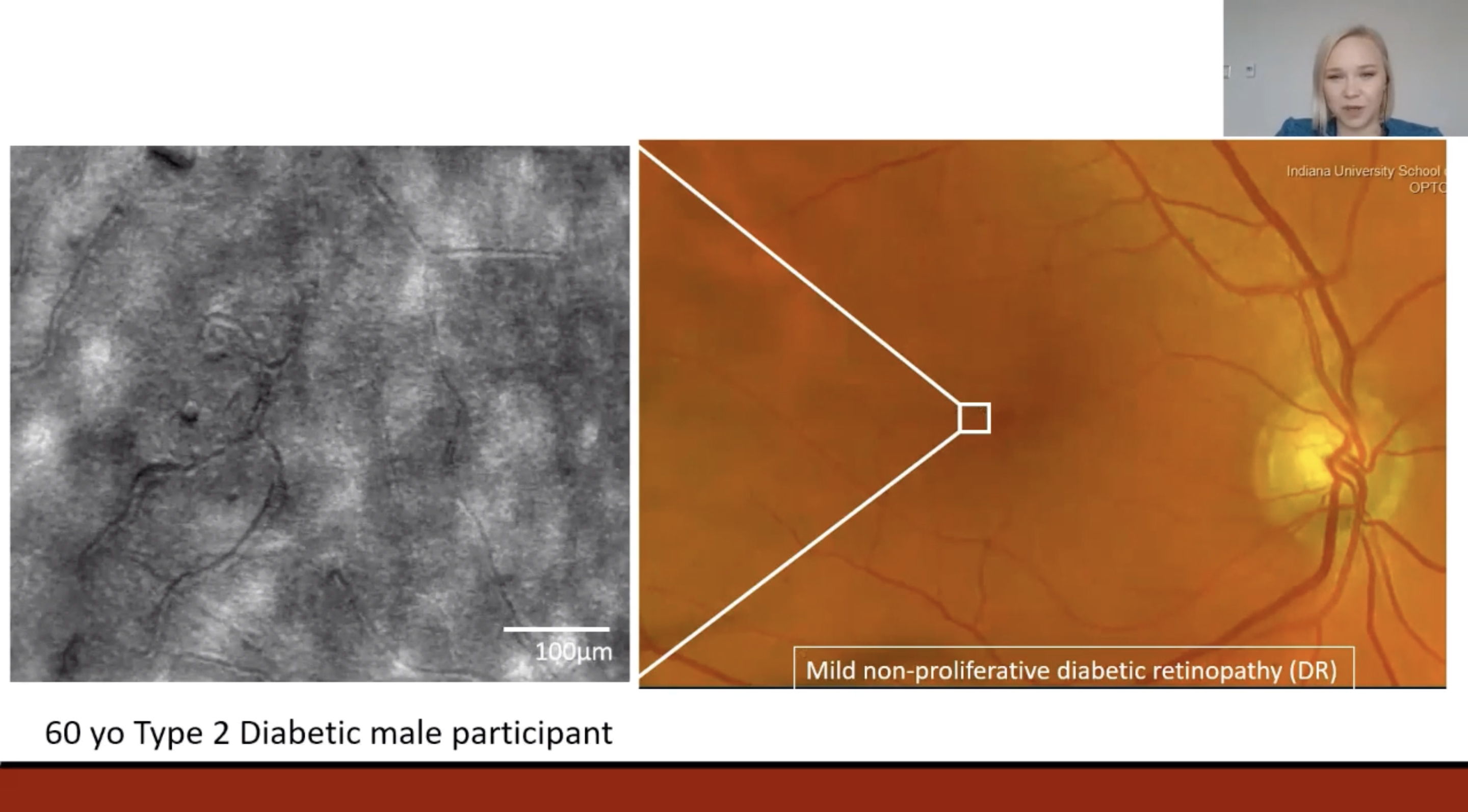
A recent study investigated the hypothesis that arteriolar structure in diabetes is altered including increases in wall thickness and wall-to-lumen ratio. It used adaptive optics scanning laser ophthalmoscope (AOSLO) imaging, which enables unique visualization of the retinal microvasculature that is compromised in diabetes, such as the structural properties of small retinal vessels. “We can get much more resolution and information on what’s actually going on to the vessel structure in these patients,” said Kaitlyn Sapoznik, OD, of the Indiana University School of Optometry as she presented the study’s results yesterday. Diabetic individuals had significant alterations in arteriole wall structure, specifically wall thickness and wall-to-lumen ratio, in arterioles of 50µm diameter or less.
The retinal microvasculature of one eye each of 45 participants (19 with diabetes mellitus, 26 controls) was imaged, and 265 arteriole segments (157 diabetes, 108 control) were selected for analysis.
Dr. Sapoznik and her team found that wall-to-lumen ratio and arteriole diameter are inversely related in both diabetic and control participants. The wall-to-lumen ratio was significantly larger in the diabetic participants compared to controls for all arteriole segments (0.7 vs. 0.5) and segments with diameters 50µm or less (0.7 vs. 0.55). There was no significant difference in wall thickness between the diabetic group and control participants (10.07µm vs. 10.27µm) for all segments, but for the smaller arteriole segments with diameters 50µm or less, the diabetic group had significantly larger total wall thicknesses (10.07µm vs. 9.3µm). The ratios of the predicted lumen diameter and the actual lumen diameter of individual subjects were significantly different between diabetic and control participants (0.93 vs. 1.00).
When comparing the ratios between controls (n=26), participants with no diabetic retinopathy (DR) (n=5), non-proliferative DR (n=12) and proliferative DR (n=2), there was a significant difference between groups as determined by one-way ANOVA. The researchers concluded that arteriole walls in small vessels, even in early DR, are thickened and arteriole structural remodeling of the walls is occurring.
 |
 |
The above summary was presented at the Academy press conference on October 7. Dr. Sapoznik will give a full presentation in this session:
P-07: Papers: Investigations into Retinal Findings in the Aging Eye and Patients with Diabetes, Friday, October 9, 7-7:15pm
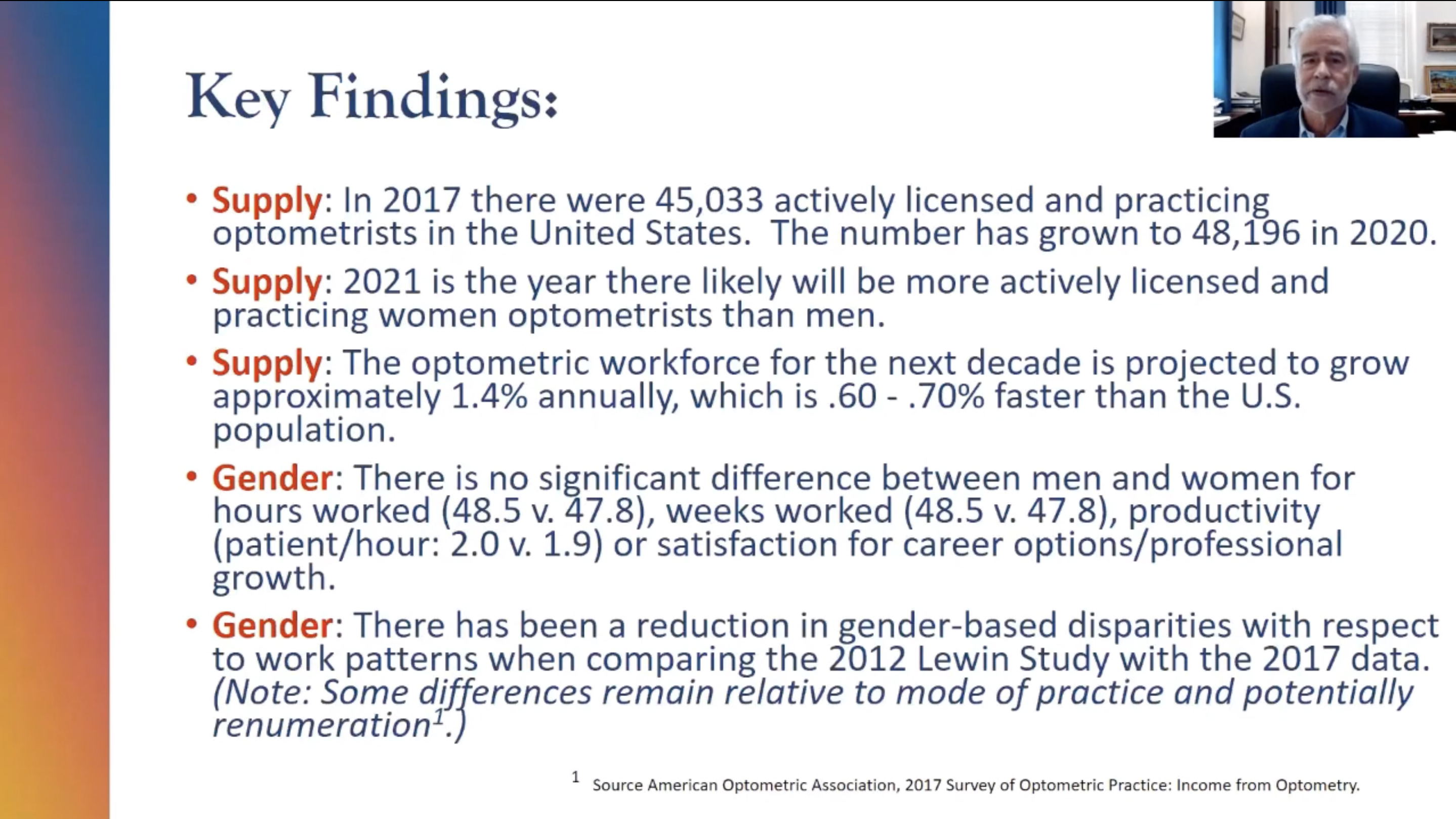
Optometry is Growing, Diversifying
Findings indicate an evolving and equitable workforce, based on productivity and satisfaction.
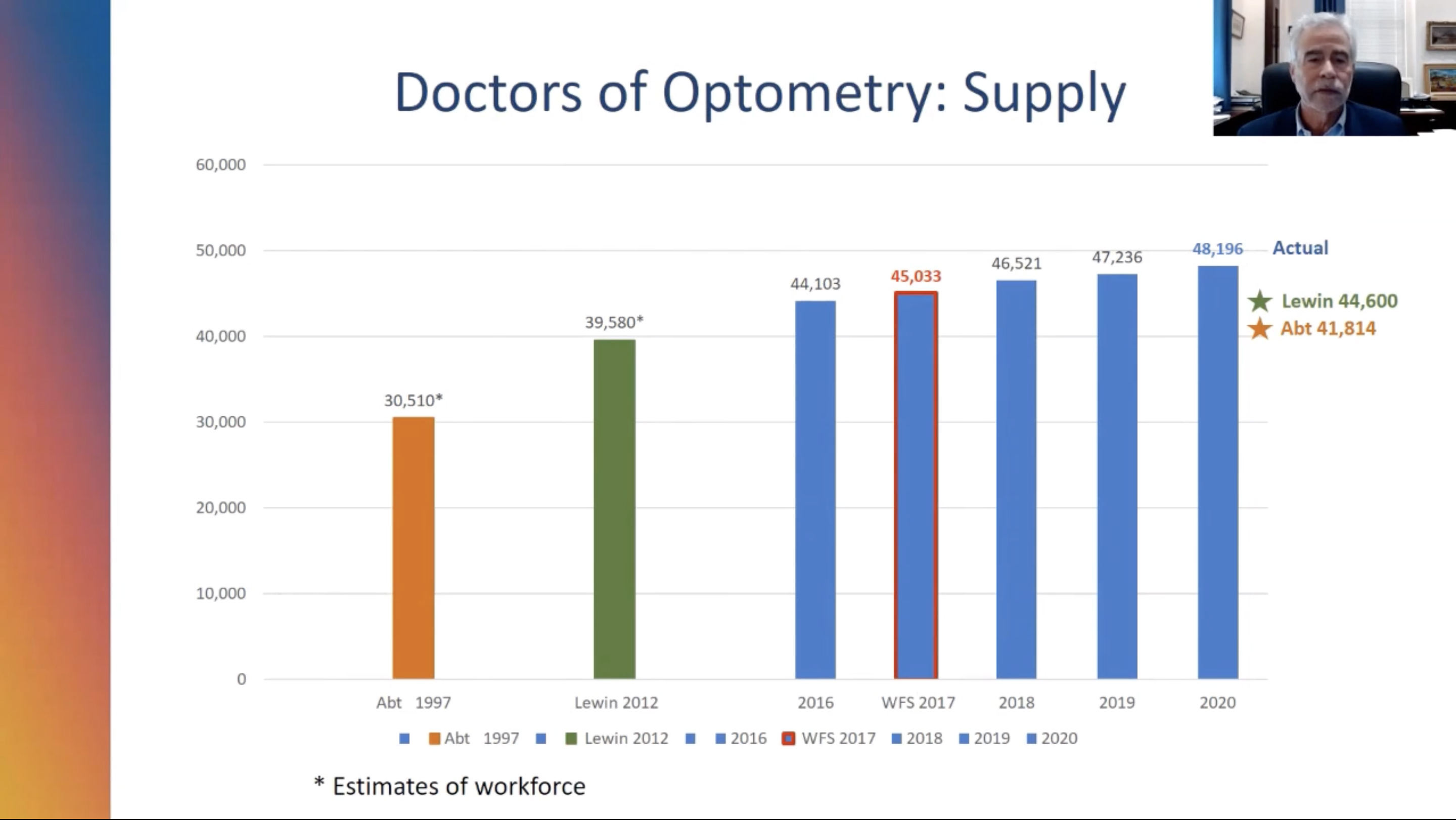
Optometry will continue to grow in the United States, according to the results of a recent study. The 2017 National Optometry Workforce Survey was fielded to 4,050 optometrists to assess the current and future supply of doctors of optometry. The survey also examined in-depth trends of demographic shifts, gender-based disparities, differences in practice behaviors between self-employed and employed ODs and potential “additional patient” capacity.
The results were presented yesterday by David Heath, OD, EdM, president of the SUNY College of Optometry. “Planning for the delivery of eye care on all levels depends upon an accurate and detailed knowledge of the optometric workforce in an understanding of demographic and behavioral trends to better meet the future needs of the public,” Dr. Heath said at the beginning of his presentation.
From 1,158 responses, the study noted no significant differences between men and women in hours (38.9 vs. 37.5, respectively), productivity (2.0 vs 1.9 patient visits/hour) or career options/professional growth satisfaction (65% for both groups). “We’re very close to parity, and we’re expecting the inversion, with more female than mal practicing optometrists in the not so distant future,” Dr. Heath noted. “By 2021, there will likely be more actively licensed practicing women optometrists than men.”
The trends toward employed vs. self-employed was marked with 44% reporting as employed, up from 29% in 2012. In 2017, there were 45,033 actively licensed and practicing optometrists in the United State; it has grown to 48,196 in 2020. Regarding “additional patient” capacity, the data indicated a potential 2.29 to 2.57 patients/week, which could mean 5.05 million to 5.65 million additional patients annually for the profession.
The study concluded that the optometric workforce for the next decade is projected to grow about 1.4% annually, 0.6% to 0.7% faster than the US population.
 |
 |
The above summary was presented at the Academy press conference on October 7. Dr. Heath will give a full presentation in this session:
P-01: Papers: Optometric Practice Patterns and Service Delivery, Wednesday, October 7, 5-5:15pm
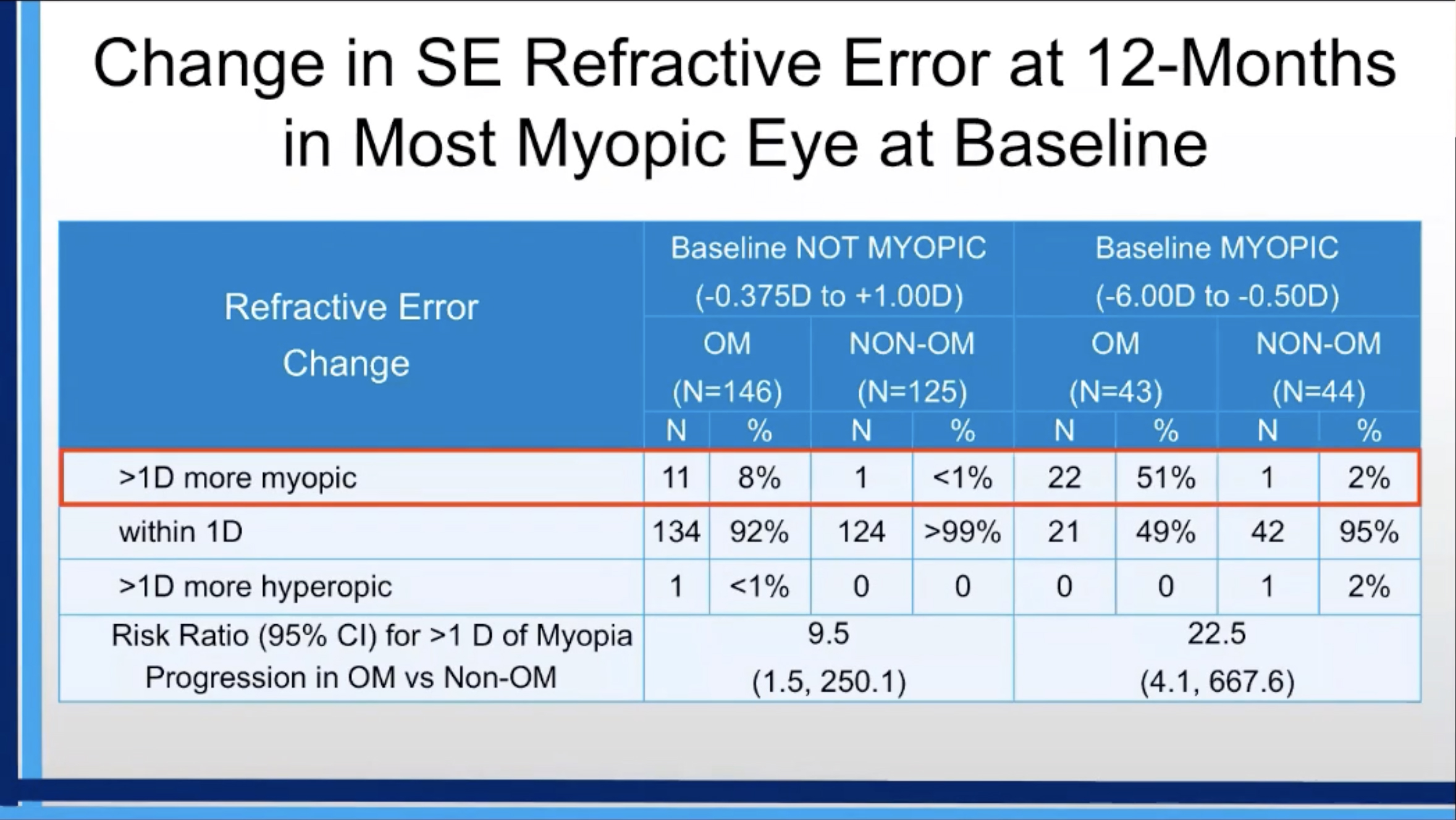
Overminus Lenses For Exotropia Associated with Myopia Progression
Study found association in 51% of children who were already myopic.
“Clinicians have expressed concern that the extra accommodative effort required with overminus spectacles might increase myopia progression,” Sergul Erzurum, MD, noted yesterday in her presentation at the Academy press conference. She and her team of researchers have determined that overminus lens treatment for childhood intermittent exotropia is associated with increased progression of myopia, especially in children who are already myopic.
The study evaluated change in refractive error in children treated with overminus compared with non-overminus spectacles for 12 months and enrolled 386 three- to 10-year-old children with intermittent exotropia with 196 who received overminus spectacles (-2.50D over cycloplegic refraction) or non-overminus spectacles (refractive error correction only, if needed, or plano spectacles for participants who did not need refractive correction). The researchers performed cycloplegic refraction within two months prior to the baseline exam and again at 12 months after randomization.
Dr. Erzurum found that the mean change in SE refractive error from baseline to 12 months was greater in the overminus group than the non-overminus group (-0.42D vs -0.04D). Also, 17% of the participants in the overminus group and 1% in the non-overminus group had more than 1.00D of myopia progression (risk ratio = 14.8). The risk ratio for having more than 1.00D of myopia progression over 12 months in the overminus vs. non-overminus group was 22.5 (51% vs. 2%) in the 87 participants who were myopic at baseline (SE -0.50D to -6.00D) and 6.4 (13% vs. 2%) in the 108 participants who were emmetropic (SE -0.375D to +0.375D) at baseline. Among the 161 participants with low hyperopia (SE +0.50D to +1.00D) at baseline, 4% of those randomized to overminus and 0% randomized to non-overminus had more than 1.00D of myopia progression at 12 months.
“Long-term effects of overminus therapy is unknown and we are now collecting refractive error and axial length data at 24 and 36 months,” Dr. Erzurum concluded. “Before considering overminus therapy, discuss the risk of myopic progression with parents.
 |
The above summary was presented at the Academy press conference on October 7. Dr. Erzurum will give a full presentation in this session:
POS-04: Posters: Pediatric & Binocular Vision II, Wednesday, October 7, 7:15-8:15pm
New Glasses Could Reduce Myopia Progression in Children
Spectacles are designed to reduce contrast signaling in the retina to slow myopia progression.
Joseph Rappon, OD, MS, FAAO, chief medical officer of SightGlass Vision, presented the results of a study on glasses designed to reduce myopia progression in yesterday’s session. “Once children are diagnosed with myopia, they are usually corrected for their myopia to see clearly,” Dr. Rappon said. “However, children are almost always left untreated in terms of preventing or reducing the progression of their myopia.”
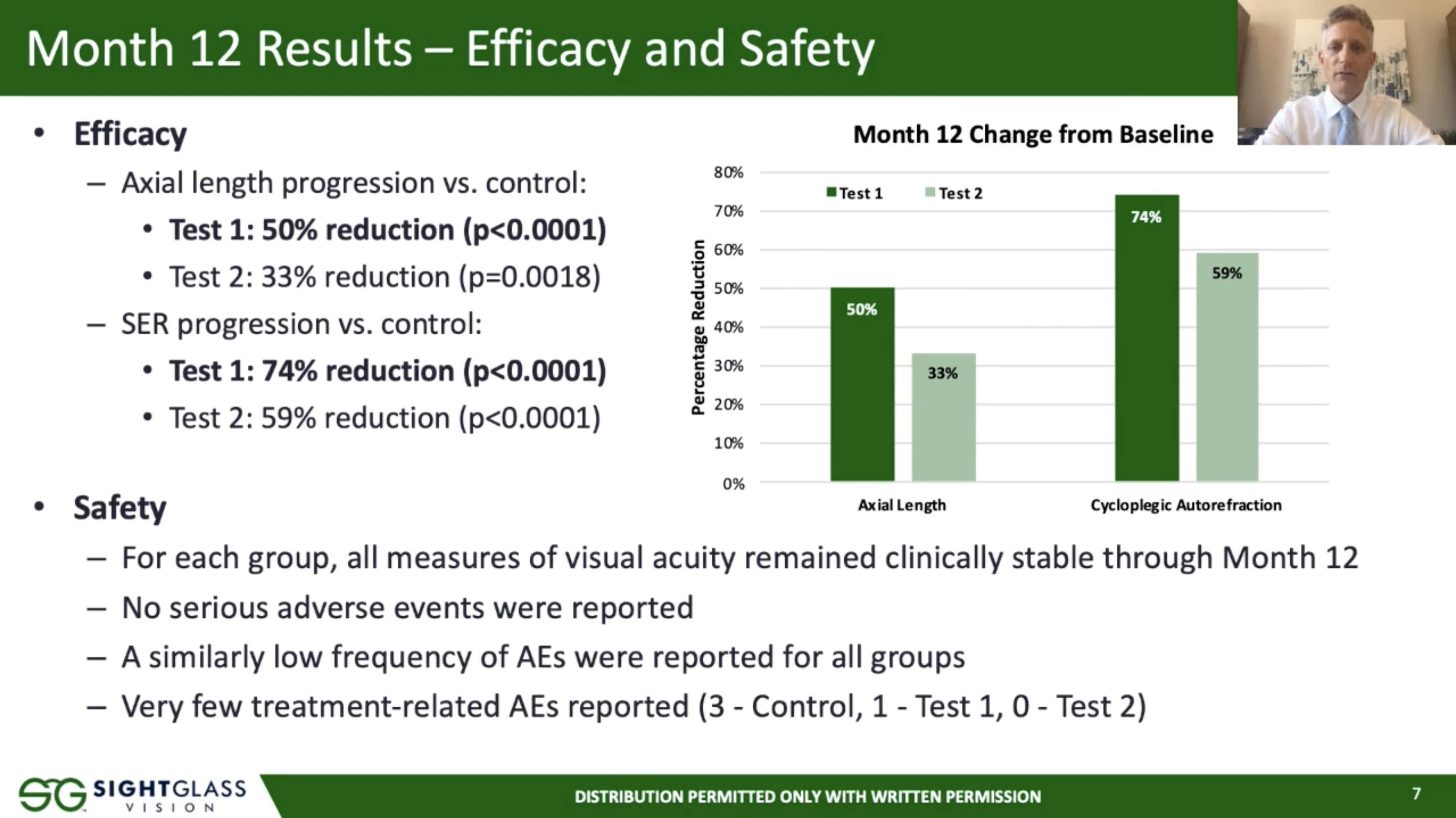
To determine the safety and efficacy of the novel lenses and support regulatory approval, researchers conducted a randomized controlled clinical trial in 256 children (mean age at screening=8.1) with myopia. The spectacles are designed, based on a hypothesis that retinal contrast causes myopia and predicted that reducing contrast signaling in the retina can slow myopia progression. The two investigational lens designs employed slightly reduce contrast in the periphery with no impact to primary gaze vision. The study followed the children for a total of 36 months, with pre-planned interim analyses at 12 and 24 months. Based on results from the subject and parent questionnaires, the investigational lenses were well-tolerated, both visually and cosmetically.
At baseline, the mean spherical equivalent refraction (SER) was -2.01D using manifest refraction, mean cycloplegic autorefraction was -1.94D and mean axial length (AL) was 24.02mm. At 12 months, the mean difference in SER progression for Test 1 vs. control was 0.40D, a 74% reduction. For Test 2 vs. control, the difference in SER progression was 0.32D, representing a 59% reduction. The difference in AL progression for Test 1 vs. control was 50% reduction, and Test 2 vs. control was a 33% reduction. All measures of visual acuity were clinically stable and there were no adverse events related to the test lenses through 12 months.
The study concluded that, based on the results at 12 months of the ongoing clinical trial, the team has demonstrated the safety and effectiveness of these spectacles for reducing myopic progression in children. “The investigational spectacles used in this study were designed to slightly reduce retinal contrast and therefore represent a new class of treatment for myopia,” Dr. Rappon emphasized.
 |
The above summary was presented at the Academy press conference on October 7. Dr. Rappon will give a full presentation in this session:
P-08: Posters: Clinical Myopia, Friday, October 9, 8:15-8:30pm
Multifocal Soft Lenses Inhibit Axial Elongation in Myopia Children
Minor differences between axial and peripheral elongation found were only on a small scale.
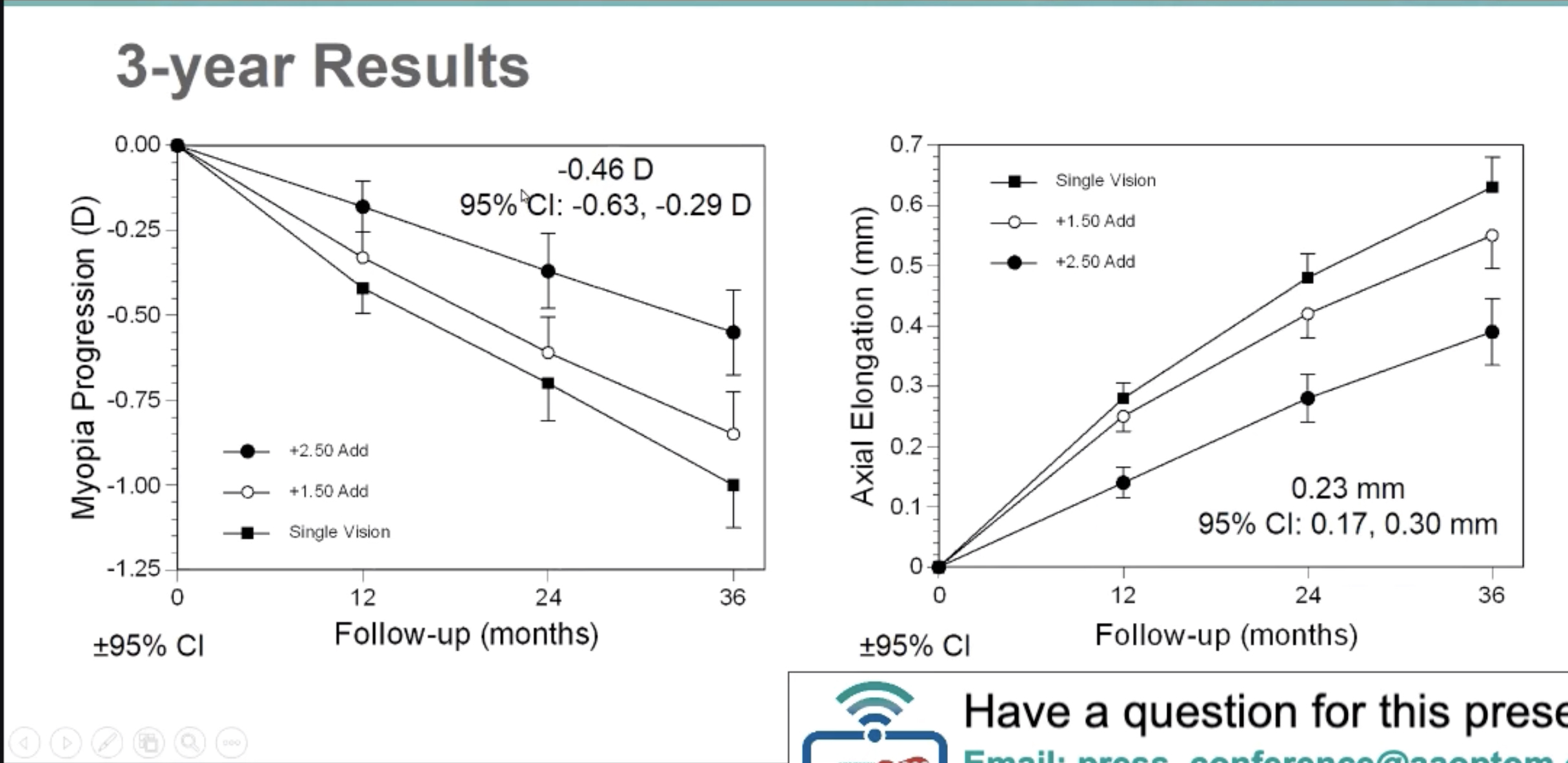
Donald Mutti, OD, PhD, FAAO, of the Ohio State University College of Optometry, presented an analysis of the Bifocal Lenses In Nearsighted Kids (BLINK) Study. This high-profile work compared axial and peripheral eye elongation to determine whether multifocal soft contact lenses affect eye growth in a regionally specific manner or more globally in a symmetric pattern between meridians. Wearing a +2.50D add multifocal soft lens appeared to inhibit axial elongation slightly more than peripheral elongation, particularly in the vertical meridian, compared to single vision contact lenses.
This study looked at 294 children from seven to 11 years old with between -0.75D to -5.00D of myopia and less than 1.00D astigmatism at baseline. The children were randomly assigned to wear Biofinity soft contact lenses for three years in one of three groups: D-design multifocal with a +2.50D add, a +1.50D add or single vision.
For children wearing +2.50D add multifocal soft lenses, axial elongation was either not significantly different than peripheral elongation (horizontal meridian), or was reversed, with less axial than peripheral elongation in the vertical meridian by 0.040mm. Axial elongation was inhibited the most and vertical periphery inhibited the least. “Elongation occurs at all retinal points but at a slower rate with a +2.50D add,” Dr. Mutti noted.
Axial elongation over three years was slightly greater than peripheral elongation in both meridians in children wearing single vision lenses. Model estimates of the axial-peripheral difference at 30° were 0.047mm and 0.067mm for the horizontal and vertical meridian, respectively.
Ocular enlargement over three years was generally symmetric across ±30° of the retina, but there were noteworthy minor differences between axial and peripheral elongation as a function of the treatment group. The researchers believe these factors potentially responsible for these minor meridional asymmetries between axial and peripheral elongation need to be explored and might include choroidal thickness changes or effects due to alteration of the accommodative response. “Multifocal soft contact lenses inhibit eye growth in a global and generally symmetric manner,” Dr. Mutti concluded. “There are asymmetries, but they’re only on a small scale.”
 |
 |
The above summary was presented at the Academy press conference on October 7. Dr. Mutti will give a full presentation in this session:
P-08: Posters: Clinical Myopia, Friday, October 9, 8:30-8:45pm
Non-surgical Blepharoptosis Treatment Looks Promising
Magnetic levator prosthesis provides similar eye opening and completeness of spontaneous blink.
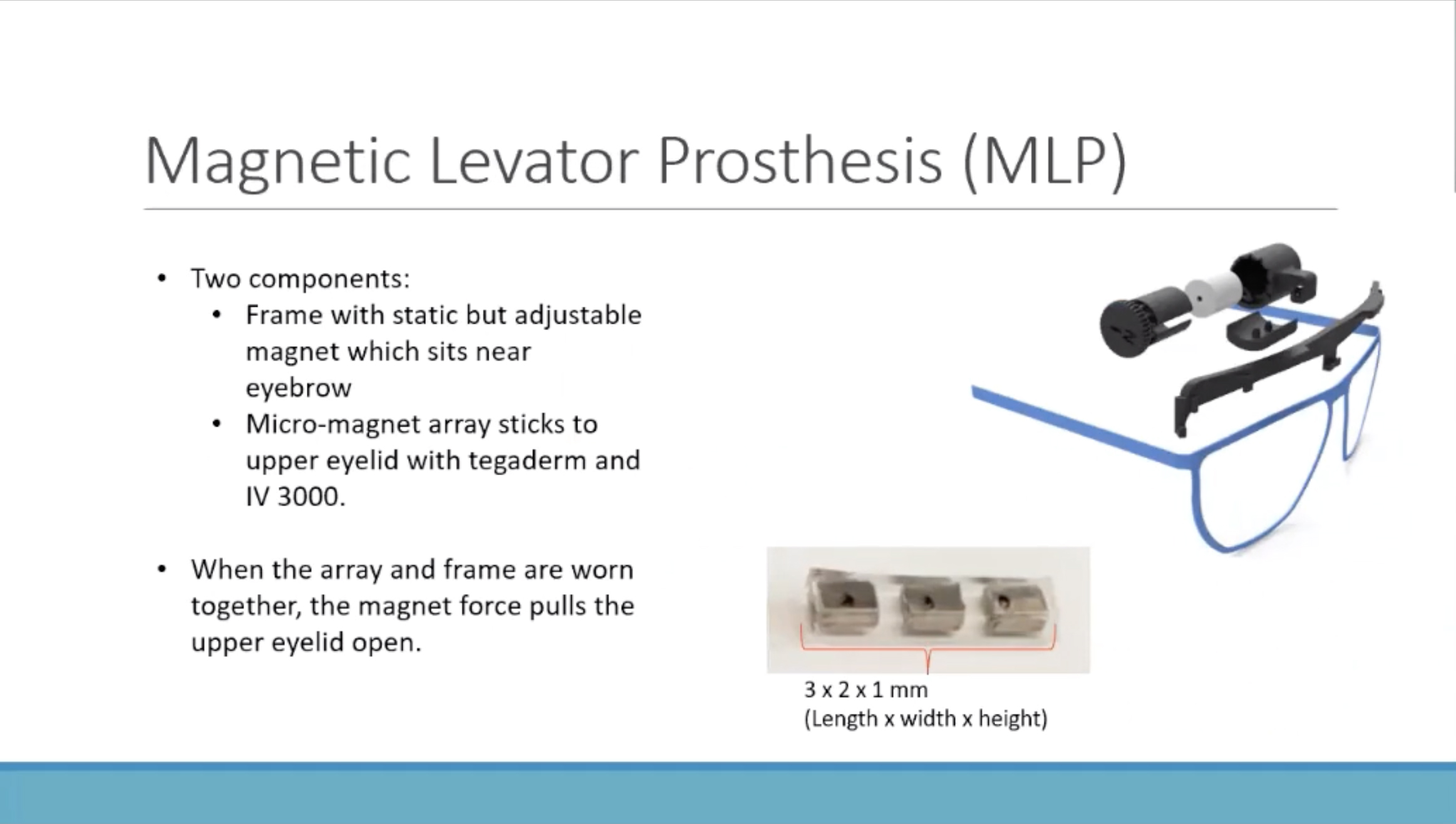
An investigational treatment for severe blepharoptosis called the magnetic levator prosthesis (MLP)—comprised of a magnetic adhesive on the eyelid and a magnet in a spectacle frame above the eye—might one day spare ptosis patients a trip to the oculoplastics surgeon. Melanie Nadeau, CLVT, MSc, of the Schepens Eye Research Institute at Harvard Medical School presented the latest research on the MLP yesterday.
When titrated correctly, the lid is suspended by the magnetic field and pulled open. The force allows a blink when desired, reanimating the lid. The recent study performed preliminary non-inferiority analysis of initial MLP response compared with the standard surgical correction of blepharoptosis: external levator advancement (ELA) and frontalis suspension (FS) surgeries.
The study included 14 patients (18 eyes) with severe ptosis occluding the visual axis, seven of whom had a prior ptosis surgery in at least one eye. Mean eye opening (the interpalpebral fissure) and volitional blinks were not significantly different between the MLP and surgery. The opening for MLP, ELA and FS were 6.82mm, 5.77mm and 4.42mm, respectively. Spontaneous blink were 3.72mm, 2.47mm and 2.95mm, respectively.
The researchers concluded that their results suggest MLP could be as effective as surgery in ptosis. “Continued investigation is warranted assessing longer-term use of the MLP and to determine if spontaneous blink can be improved in MLP-treated ptosis,” Dr. Nadeau noted.
 |
The above summary was presented at the Academy press conference on October 7. Ms. Nadeau will give a full presentation in this session:
POS-16: Posters: Neuro-eye and Orbit, Saturday, October 10, 5-7pm
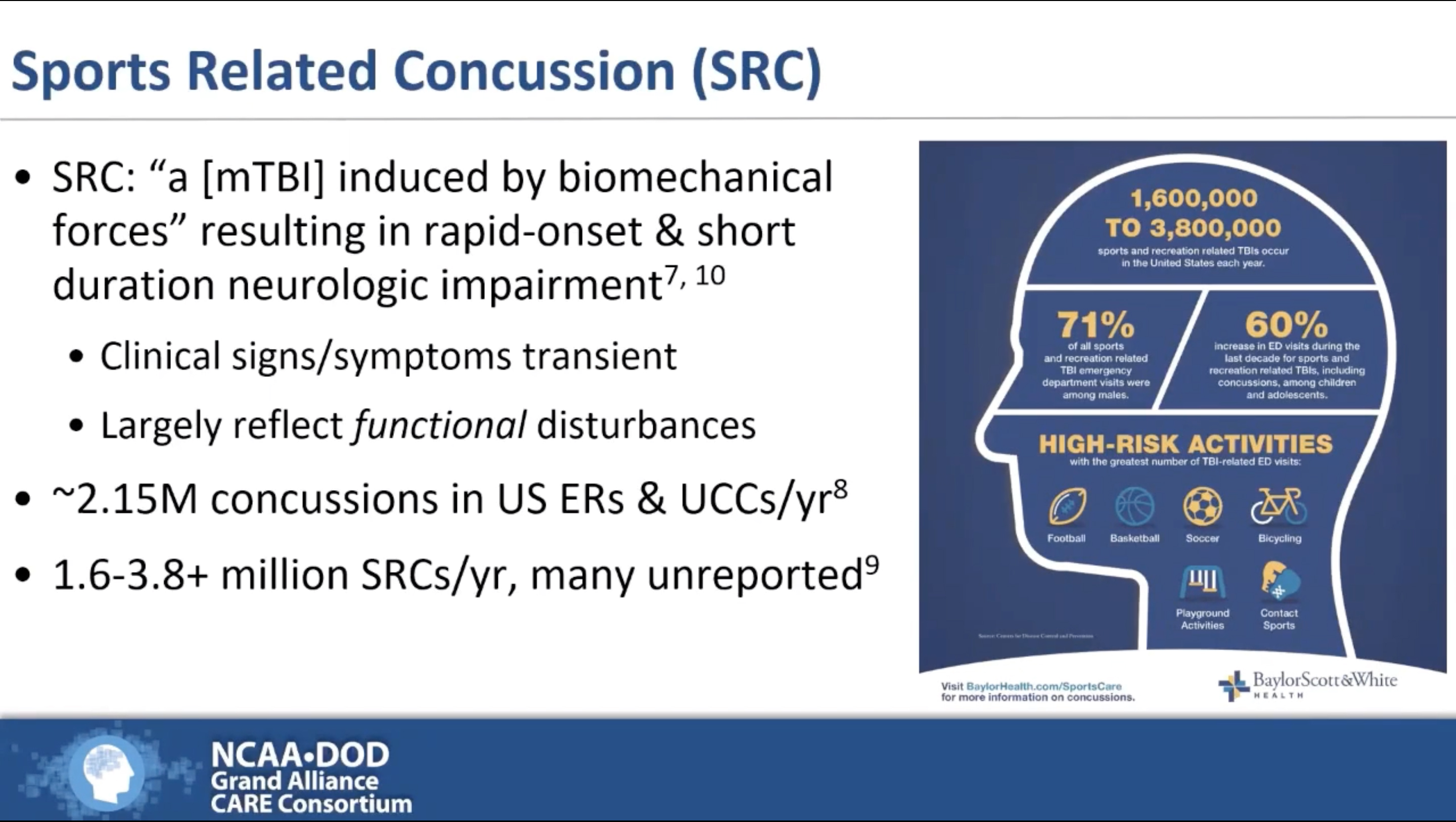
Baseline Change Scores Unnecessary for Concussion Assessments
High variance found in test-retest reliability in all commonly used tools.
Doctors who treat sports concussions need to make urgent assessments in change of status. While some proponents argue for baseline measurements at the start of a sports season, the effort may not be clinical fruitful, noted Lyndsey Ferris, OD, FAAO, from the Indiana University School of Optometry, who presented her group’s findings yesterday. Many consider baseline measurements to be expensive, time-consuming and logistically challenging.
Incorporating preseason baseline measurements for the Vestibular/Ocular-Motor Screening (VOMS) total symptom tool, VOMS mean near point convergence (NPC) or the Sport Concussion Assessment Tool (SCAT3) when identifying acute concussion within six to 48 hours of injury did not improve diagnostic accuracy.
The study analyzed preseason baseline and acute concussion VOMS and SCAT3 scores for a total of 3,430 collegiate athletes. VOMS total symptom score and SCAT symptom severity yielded the largest effect sizes between preseason and acute concussion, whereas the VOMS mean NPC and modified Balance Error Scoring System (mBESS) had medium effect sizes, with Sideline Assessment of Concussion (SAC) having a small effect size. Using preseason change scores reduced the effect sizes for all assessments.
“For each tool, we compared how accurately it predicted an athlete being concussed based on (1) post-injury only or (2) when we incorporated the athlete’s preseason performance through and individualized preseason change score,” Dr. Ferris stated.
Overall predictive value for receiver operating characteristic (ROC) analyses without incorporating preseason baselines for the five tools were area under the curve = 0.85, 0.82, 0.54, 0.56 and 0.59, respectively. ROC analyses revealed no meaningful improvement with the use of preseason change scores for any tool. “There was no meaningful difference between the two methods, Dr. Ferris noted. “For VOMS and SCAT3, using normative reference data is on par with an individualized approach.”
Dr. Ferris concluded that VOMS total symptom score, which evaluates vestibulo-oculomotor dysfunction symptoms, shows consistent utility and high accuracy for identifying acute concussion. “Therefore, preseason baseline testing may not provide a meaningful diagnostic benefit to justify the time, financial and logistical burdens they place on athletic organizations or providers,” she said.
 |
The above summary was presented at the Academy press conference on October 7. Ms. Nadeau will give a full presentation in this session:
POS-09: Papers: Traumatic Brain Injury, Saturday, October 10, 11-11:15am
