 |
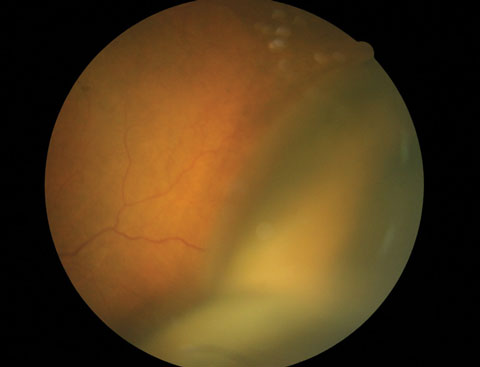
Systemic steroids treatment after suprachoroidal hemorrhage were associated with better change in vision, final vision and anatomic success. Photo: Andrew S. Gurwood, OD. Click image to enlarge. |
Despite systemic steroids being a commonly discussed treatment option for suprachoroidal hemorrhage (SCH), their use has not been directly studied. In new research determining factors associated with visual and anatomic outcomes of SCH, a team from the University of Penn and Cairo University found that steroids improve visual acuity, final acuity and odds of anatomic success.
A total of 413 eyes from 49 studies published between 1990 and 2022 were included, with a mean age of 60.8 years and follow-up of 13.8 months. Among 145 eyes with at least six months of follow-up, the mean gain in visual acuity was -0.98 (0.89) logMAR.
“We found some evidence that eyes with more severe SCH (e.g., those precipitated by corneal surgery or presenting with expulsive SCH) were more likely to receive systemic steroids, a difference that would be expected to weaken the observed benefit of systemic steroids,” the authors explained. “However, we still observed significantly better change in vision, final vision and anatomic success among patients receiving systemic steroids.”
In contrast, surgical technique and timing of surgery, were not clearly associated with better change in visual acuity.
The mechanism for a potential benefit of systemic steroids for SCH is unclear, the authors noted, but pathophysiologic studies suggest that steroids may help restore the normal balance of fluid flow in the suprachoroidal space.
“Under physiologic conditions, the suprachoroidal space is kept empty in part due to osmotic forces, as there are more colloids in the choroidal veins compared to the suprachoroidal space,” the authors explained in their paper for Retina. “Inflammation reduces osmotic forces by accelerating breakdown of hemoglobin and increasing vascular leakage, allowing albumin and other proteins to enter the suprachoroidal space, where there is no lymphatic system or enzymatic breakdown to facilitate clearance. By reducing inflammation, steroids may help restore these osmotic forces to facilitate resolution of SCH.”
Systemic steroids have been shown to restore photoreceptor volume in the setting of inflammatory chorioretinopathies, and reducing inflammation may help preserve retinal integrity in SCH, the authors added.
They also found that SCH precipitated by corneal surgeries was associated with worse change in logMAR VA than SCH precipitated by other types of surgeries, although they note this finding should be interpreted in light of the small number of eyes with corneal surgery-associated SCH. “In a review of SCH occurring during penetrating keratoplasty, Bandivadekar et al. noted that visual outcomes tended to be poor and attributed this to the open-sky nature of penetrating keratoplasty, leading to a higher risk of SCH progressing to expulsive hemorrhage,” the authors noted.
Liu T, Elnahry AG, Tauqeer Z, et al. Factors associated with outcomes of suprachoroidal hemorrhage: an individual participant data systemic review. Retina. March 6, 2024. [Epub ahead of print]. |


