|
A 22-year Hispanic female was referred with concern for optic nerve edema in both eyes (OU). She was symptomatic to left-sided headache for one week with ipsilateral transient visual obscuration (TVO) and a “pressure” sensation behind her left eye (OS). She denied prior history of headaches or similar episodes, recent fluctuations in weight and pulsatile tinnitus. Her BMI was 22.1 and she and was on oral contraceptive for two years.
Best-corrected visual acuity was 20/20 OU, Ishihara color plates were full OU, there was no relative afferent pupillary defect, confrontation visual fiends were full OU and there were no extraocular motility deficits. Anterior segment examination was unremarkable OU.
Take the Retina Quiz
1. What is true of the imaging scans?
a. B-scan shows hyperechoic lesions within the optic nerve head OU.
b. The optic disc is flat with sharp margins.
c. Fundus autofluorescence (FAF) shows leakage.
d. There is obscuration of the peripapillary blood vessels.
2. What is the most likely diagnosis?
a. Central retinal vein occlusion.
b. Myelinated nerve fiber.
c. Optic disc drusen.
d. Optic disc edema.
3. Which is the gold standard for diagnosis?
a. B-scan ultrasonography.
b. Computed tomography.
c. Enhanced-depth imaging OCT.
d. FAF.
4. Which of the following is a complication?
a. Anterior ischemic optic neuropathy.
b. Cataract.
c. Cystoid macular edema.
d. Retinal detachment.
5. All of the following are typical fundus findings, except:
a. Collateral disc vessels.
b. Presence of cilioretinal artery.
c. Vascular tortuosity.
d. All of the above.
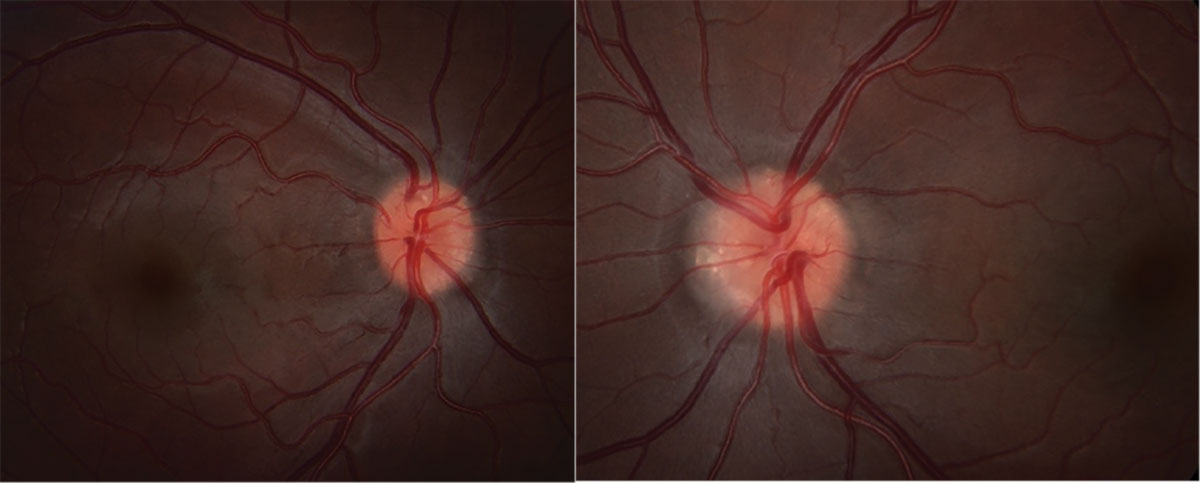 |
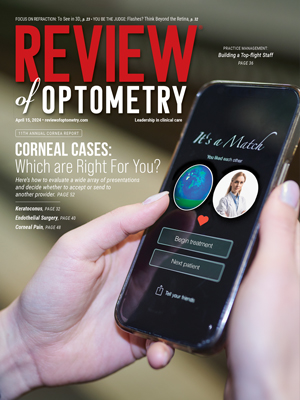
Fig. 1. Fundus photos of OD (left) and OS (right). Click image to enlarge. |
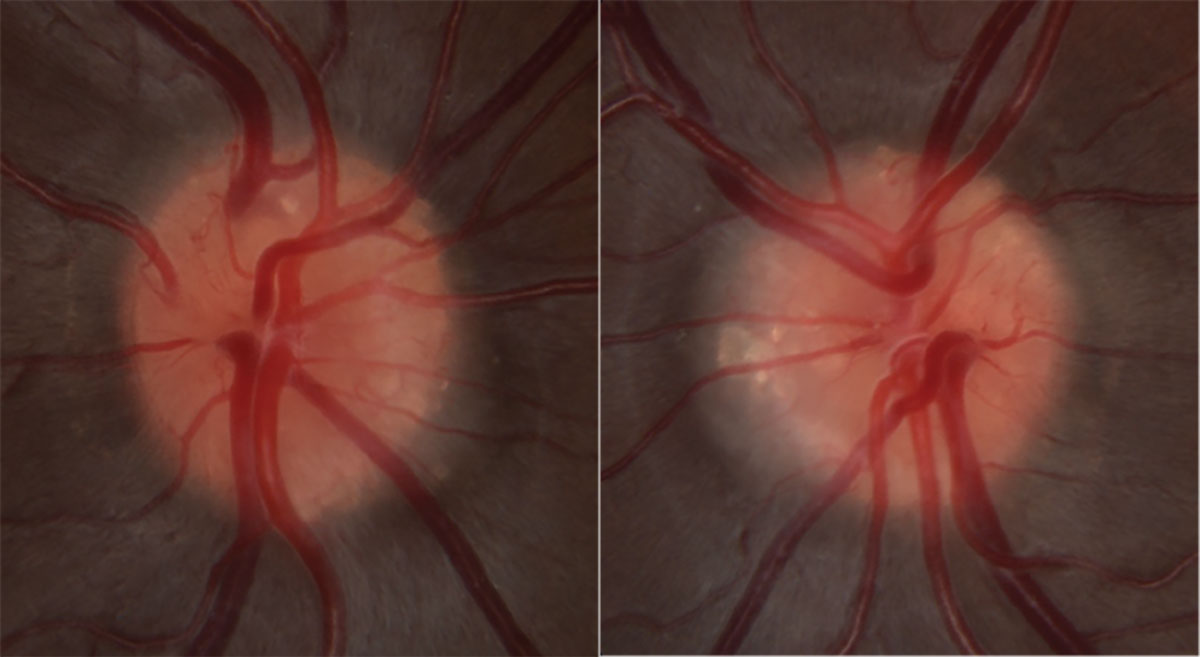 |
Fig. 2. High magnification optic nerve photos of OD (left) and OS (right). Click image to enlarge. |
Diagnosis
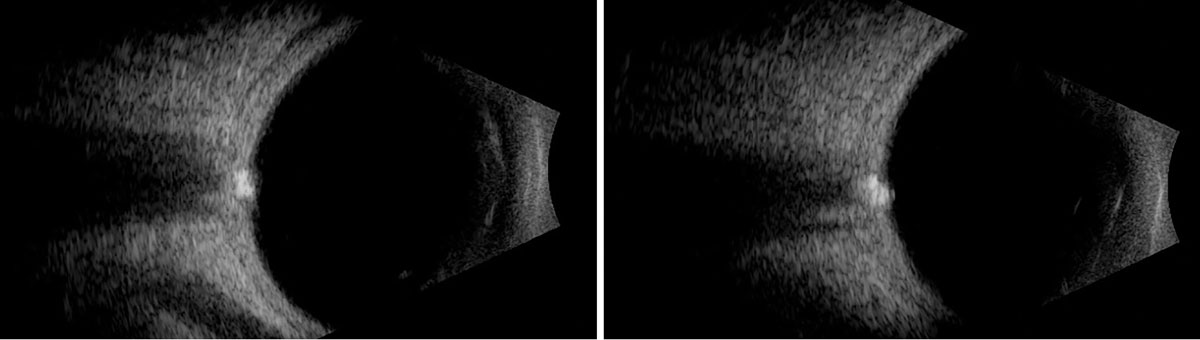
Stereoscopic fundus examination revealed bilateral optic nerve elevation with a lumpy and irregular contour (Figures 1 and 2). The disc margins appeared sharp without visible spontaneous venous pulsation present (Figures 1 and 2). FAF identified hyperAF lesions present within the optic nerve head OU (Figure 3). Further investigation with B-scan ultrasonography confirmed the presence of hyperechoic lesions buried within the optic nerve head OU (Figure 4).
While the imaging was consistent with optic disc drusen (ODD) OU, the new-onset headache with TVO raised concern for superimposed true optic nerve edema. For this reason, an MRI was obtained of the brain and orbits with and without contrast, as well as magnetic resonance venogram of the brain, to rule out intracranial mass or other etiologies of intracranial hypertension.
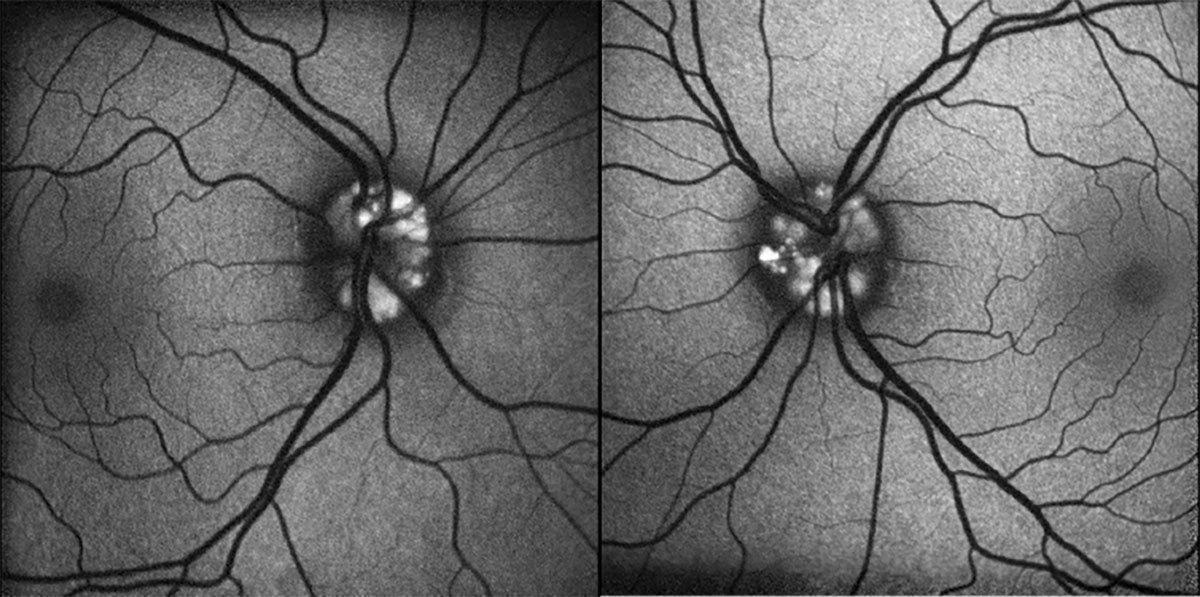 |
Fig. 3. FAF of OD (left) and OS (right). Click image to enlarge. |
ODD has a clinical prevalence of approximately one in 500 and histopathologic prevalence as high as one in 40.1 Histopathologic studies suggest a higher subclinical prevalence based on the deeper location of many clinically undiagnosed drusen due to limitations in diagnostic techniques.1-3 ODD tends to be bilateral (69% to 91%), though asymmetric, with a slight predilection toward females and Caucasians.1,2
While the exact pathophysiology is debated, the leading theory is that ODD are accumulations of metabolic byproducts due to impaired axoplasmic transport.3,4 Thus, ODD are comprised calcium phosphate, mucopolysaccharides, amino acids and nucleic acids.3-5 A small portion of ODD shows an autosomal dominant inheritance pattern with a positive family history portending a 10 times higher risk of ODD.5-7
Clinically, ODD are either classified as visible/superficial (nodular and elevated optic nerve appearance) or buried/deep (undetectable by ophthalmoscopic examination).3-5 Buried ODD tend to be more common in children due to the natural history of these lesions to acquire calcium and eventually erupt to the surface with age, often during teenage years.3-5 While ODD may obscure the optic disc margins, they rarely induce peripapillary blood vessel obscurations due to their anatomic location.1,3,8
ODD are rarely symptomatic and most commonly found incidentally on exam as the most frequent cause of pseudopapilledema.1,3 This highlights the importance of a careful review of systems and evaluating the peripapillary vasculature for slight blood vessel obscurations as pseudopapilledema may be superimposed with true papilledema.1,8 A pediatric case series of patients with idiopathic intracranial hypertension showed a high concomitant ODD prevalence of 15%, with 72% of patients affected by headache followed by 45% with TVO.8
Ophthalmoscopic examination is enhanced by ancillary testing such as B-scan ultrasonography, FAF and fluorescein angiography (FA). B-scan ultrasound is the diagnostic gold standard with the highest sensitivity at detecting calcific lesions present within the optic nerve head substance, though it is less effective at identifying buried ODD due to lack of calcification.1,3,4,6 While less sensitive than B-scan, FAF similarly shows hyperautofluorescence of superficial ODD better than with buried ODD.1,3,4,6 Combining FAF with FA is useful to assess for true optic nerve edema as FA will demonstrate leakage of the optic nerve whereas ODD will demonstrate nodular staining of the lesions.1,4
 |
|
Fig. 4. B-scan ultrasound horizontal axial scans over the nerve OD (left) and OS (right). Click image to enlarge. |
There are emerging bodies of evidence attempting to validate enhanced-depth imaging OCT, though it has not yet been shown to outperform B-scan ultrasound as the diagnostic gold standard.9 It is worth commenting that ODD appear as hyperintense foci on computed tomography due to their calcific nature, but it can be easily missed with slices 1.5mm or greater and ODD alone is not an indication for CT imaging due to radiation exposure.1,5
Nearly half of eyes with ODD have normal visual field testing, and approximately one in three eyes will show an enlarged blind spot.3 Less commonly, there may be arcuate defects or concentric narrowing of the visual field.3,5 There is a greater incidence of visual field deficits in eyes with superficial ODD as compared in eyes with buried drusen; these patients should be monitored closely with serial retinal nerve fiber layer scans as an objective measure of progression.3
Found coincidentally in patients with ODD are increased vascular tortuosity, abnormal vascular branching, collateral disc vessels and a higher incidence of cilioretinal artery presence.1, 6 The most frequent cause of visual loss in eyes with ODD is non-arteritic anterior ischemic optic neuropathy due to crowding of the optic canal similar to what occurs in patients with a physiologic “disc at risk.” Other causes of vision loss include retinal vascular occlusions (venous > arterial), progressive visual field loss and peripapillary subretinal neovascular membranes (treatment only required when foveal-threatening).1,3 Progressive visual field loss or concomitant glaucoma are managed similarly with topical ocular hypotensives to preserve as much visual function as possible; it may be difficult to subjectively detect progression by disc assessment alone, so objective metrics are often the best indicator for when to treat or escalate treatment.1,3,4 There are no recommended surgical interventions for ODD. Prognosis is generally good, and vascular events are managed as they would be in the absence of ODD.
On retrospective evaluation, one can appreciate the presence of cilioretinal artery OU and a slit defect OD without a corresponding visual field defect. Although our patient had no apparent peripapillary blood vessel obscurations, a complete neuroimaging work-up was indicated due to the new onset headache and TVO. Fortunately, there was no mass or other radiographic evidence suggestive of intracranial hypertension. This patient has been followed with stable visual fields for the last 18 months.
In summary, the presence of optic disc drusen alone does not preclude the possibility of superimposed true optic disc edema. In cases with a positive review of systems, a complete work-up is indicated to exclude concomitant disease. While the majority of eyes with ODD carry a favorable diagnosis, there are no effective therapeutic options to reverse any incurred vision loss.
Retina Quiz Answers
1: a, 2: c, 3: a, 4: b, 5: d
Dr. Aboumourad currently practices at Bascom Palmer Eye Institute in Miami. He has no financial disclosures.
1. Ryan SJ, Davis JL, Flynn HW, et al. Retina, Fifth ed. London; New York: Saunders/Elsevier, 2013. 2. Friedman AH, Beckerman B, Gold DH, et al. Drusen of the optic disc. Surv Ophthalmol. 1977;21(5):373-90. 3. Allegrini D, Pagano L, Ferrara M, et al. Optic disc drusen: a systematic review: up-to-date and future perspective. Int Ophthalmol. 2020;40(8):2119-27. 4. Auw-Haedrich C, Staubach F, Witschel H. Optic disk drusen. Surv Ophthalmol. 2002;47(6):515-32. 5. Bowling B, Kanski JJ. Kanski’s Clinical Ophthalmology: A Systematic Approach. Elsevier, 2016. 6. Chang MY, Pineles SL. Optic disk drusen in children. Surv Ophthalmol. 2016;61(6):745-58. 7. Antcliff RJ, Spalton DJ. Are optic disc drusen inherited? Ophthalmology. 1999;106(7):1278-81. 8. Genizi J, Meiselles D, Arnowitz E, et al. Optic nerve drusen is highly prevalent among children with pseudotumor cerebri syndrome. Front Neurol. 2021;12:789673. 9. Rosa N, De Bernardo M, Abbinante G, et al. Optic nerve drusen evaluation: a comparison between ultrasound and OCT. J Clin Med. 2022;11(13). |