|
Trichiasis is a condition characterized by misdirected eyelashes toward the globe. It may result in corneal or conjunctival abrasion, chronic ocular surface disease and ulceration in more severe cases.1 Patient symptoms may include pain, irritation, epiphora and foreign body sensation.2 It can be classified as primary trichiasis or secondary trichiasis.
In primary trichiasis, the eyelid margin is normally positioned but the eyelash follicles are misaligned. Primary trichiasis may occur due to severe blepharitis, recurrent chalazia, tumors, herpes zoster ophthalmicus, eyelid trauma or previous surgery.3
In secondary trichiasis, the eyelash follicles are aligned normally, but the eyelid margin is rotated inward, causing lashes to contact the globe.1 Secondary trichiasis is caused by entropion associated with eyelid laxity, retractor disinsertion or posterior lamellar contraction, as seen in conditions such as cicatricial ocular pemphigoid, Stevens-Johnson syndrome, trachoma and chemical burns.1,2 When associated with entropion, efforts should be made to correct the underlying condition before performing eyelash ablation. If entropion surgery cannot be performed or trichiasis remains after surgery, perform radiofrequency ablation.
 |
|
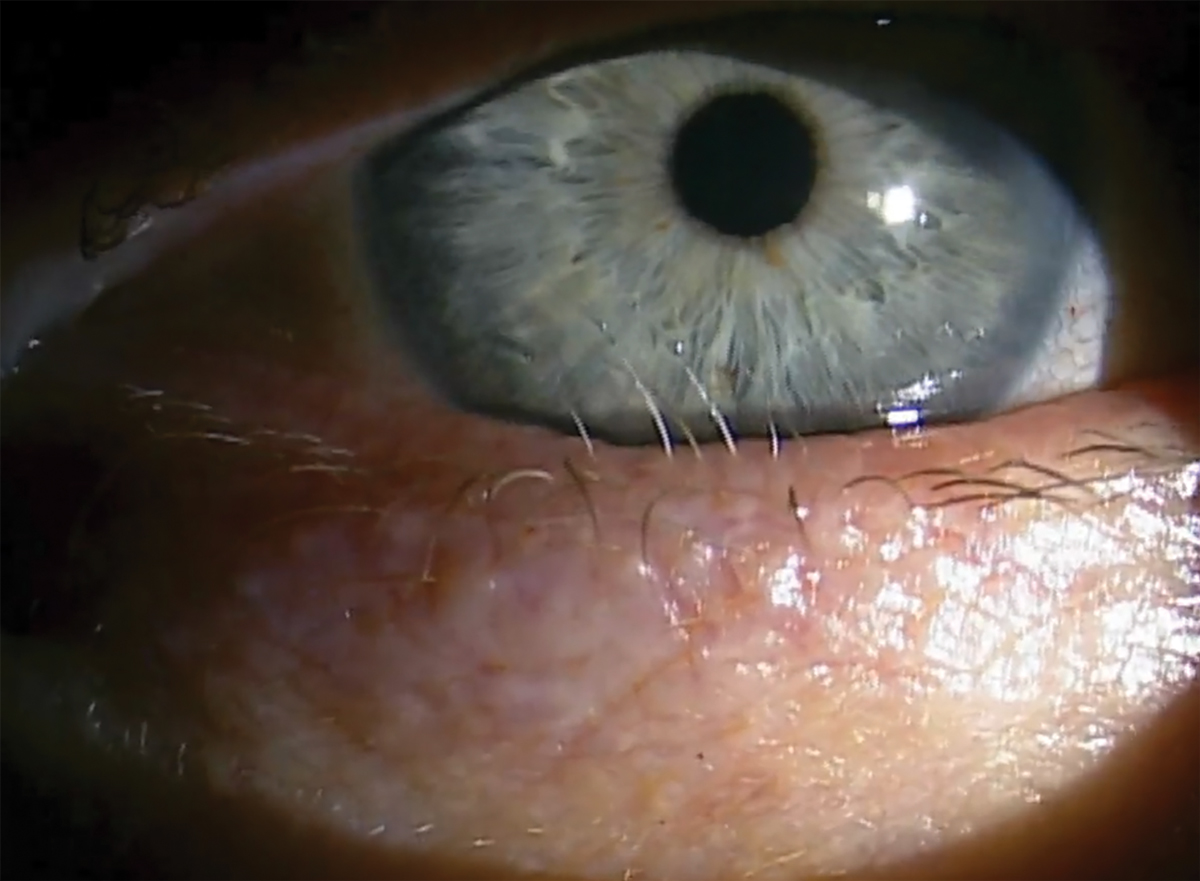
Distichiasis with six offending lashes rubbing on the globe. Click image to enlarge. |
Distichiasis is characterized by one or more extra rows of eyelashes located within the tarsus and growing behind the normal row of eyelashes at the meibomian gland orifices.1,4 This condition may be congenital or acquired. The cilia, although aligned normally, commonly result in globe touch due to their more posterior origination.
A permanent treatment method for trichiasis and distichiasis involves the use of electrosurgery to cause follicular destruction, termed trichiasis ablation. Radiofrequency is used to selectively ablate the root of eyelash follicles without side effects caused by electrocautery on the eyelid.
Contraindications
These involve the cautionary approach exercised when using radiofrequency devices. Patients with cardiac pacemakers or defibrillators and use of flammable fumes such as oxygen are contraindicated with radiofrequency. If alternative treatments are not an option, the grounding plate can be placed away from the heart and the lowest power setting can be used. Trichiasis ablation can be a timely procedure depending on the number of eyelashes that need to be removed, thus patients should be comfortable lying on their back for at least 15 to 30 minutes. Any active herpetic infection should be treated prior to surgery.
 |
|
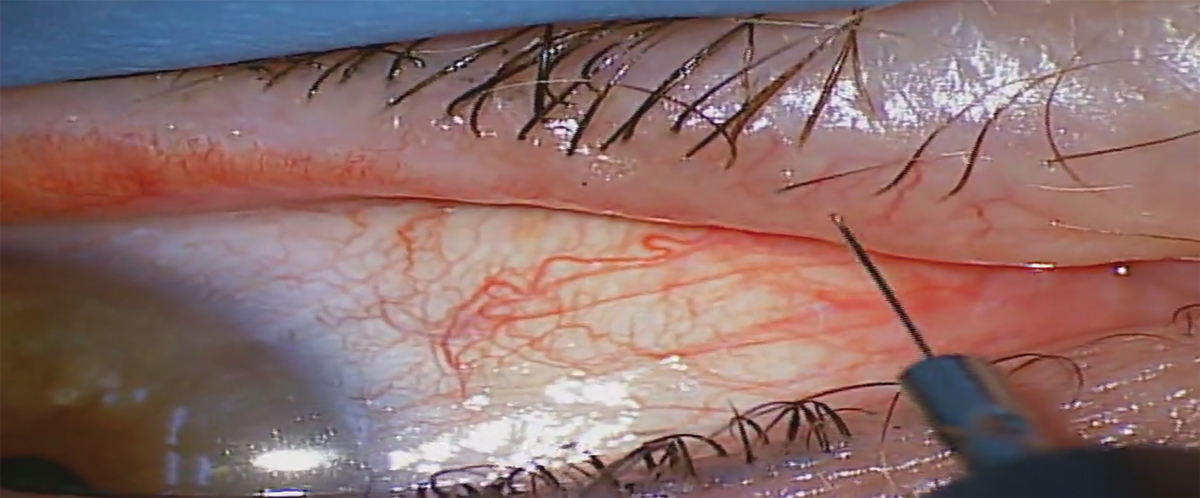
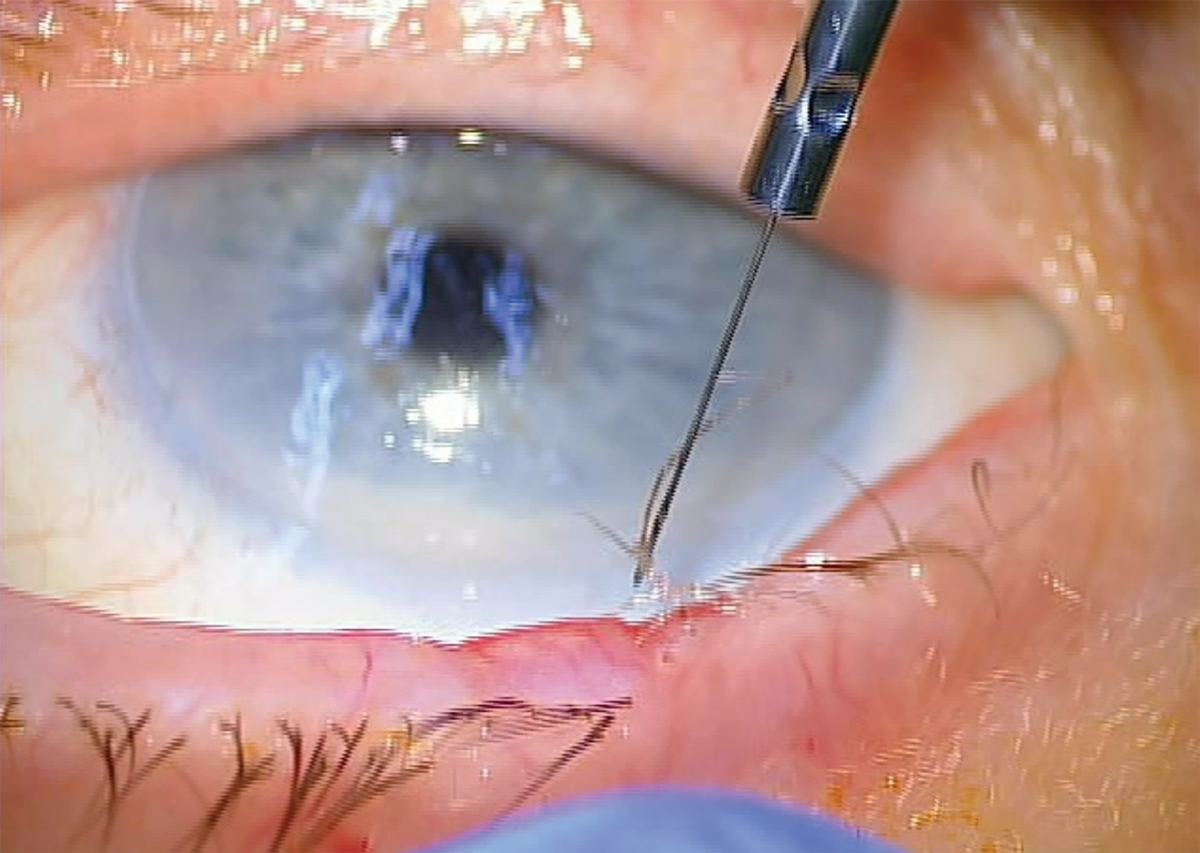
Micro-insulated electrode shown in this photo. The electrode should be inserted adjacent to the eyelash to the base of the follicle. Click image to enlarge. |
Procedural Technique
Let’s review how to perform trichiasis ablation with radiofrequency.
1. Place the patient in supine position, with the grounding plate/passive electrode of the radiofrequency unit underneath the patient’s back or shoulder area.
2. Set up the surgical microscope or loupes.
3. Instill topical anesthetic (proparacaine, tetracaine) into both eyes to minimize reflex lacrimation, the blink reflex and keep the patient comfortable during the procedure.
4. Use an alcohol prep pad to clean around the skin and eyelashes where anesthetic will be injected.
 |
|
Perfect orientation of the radiofrequency electrode down the shaft of the lash. Click image to enlarge. |
5. Use a 30-gauge needle, bevel up, to inject anesthesia (0.5%, 1% or 2% lidocaine with epinephrine 1:100,000 or 1:200,000) subcutaneously at a 10° to 15° angle adjacent to the eyelid margin where eyelashes will be treated. Avoid injecting toward the globe or directly into the eyelid margin. Continue to inject as the needle is withdrawn to form a small bolus of anesthetic either directly below the offending lashes (if on the lower eyelid) or directly above the offending lashes (if on the upper eyelid).
6. A gauze pad or cotton-tipped applicator can be used to massage the anesthesia into the area.
7. Use a 10% povidone-iodine (betadine) swabstick to clean the ocular adnexal area and eyelashes to maintain asepsis. Povidone-iodine should remain on the skin for three minutes. This step is optional, depending on treating clinician preference.
8. Use a piece of gauze to remove any excess povidone-iodine if needed.
9. Use forceps to test the area for proper anesthesia. Ask the patient if they feel any pain or pinching. Pressure sensation is expected.
10. If inadequate anesthesia is present on the eyelid margin, which commonly occurs, apply a few Weck-Cel sponges soaked in 4% topical lidocaine directly onto the offending eyelashes and eyelid margin. Hold each sponge on the eyelid for approximately 30 to 60 seconds. Always ensure the patient is fully anesthetized before performing the procedure.
11. Turn on the smoke evacuator that comes with the radiofrequency unit and place it as close to the operative site as possible; no further than 2cm.
12. Partially evert the eyelid to visualize the offending eyelashes and to keep the eyelid margin away from the globe.
 |
|
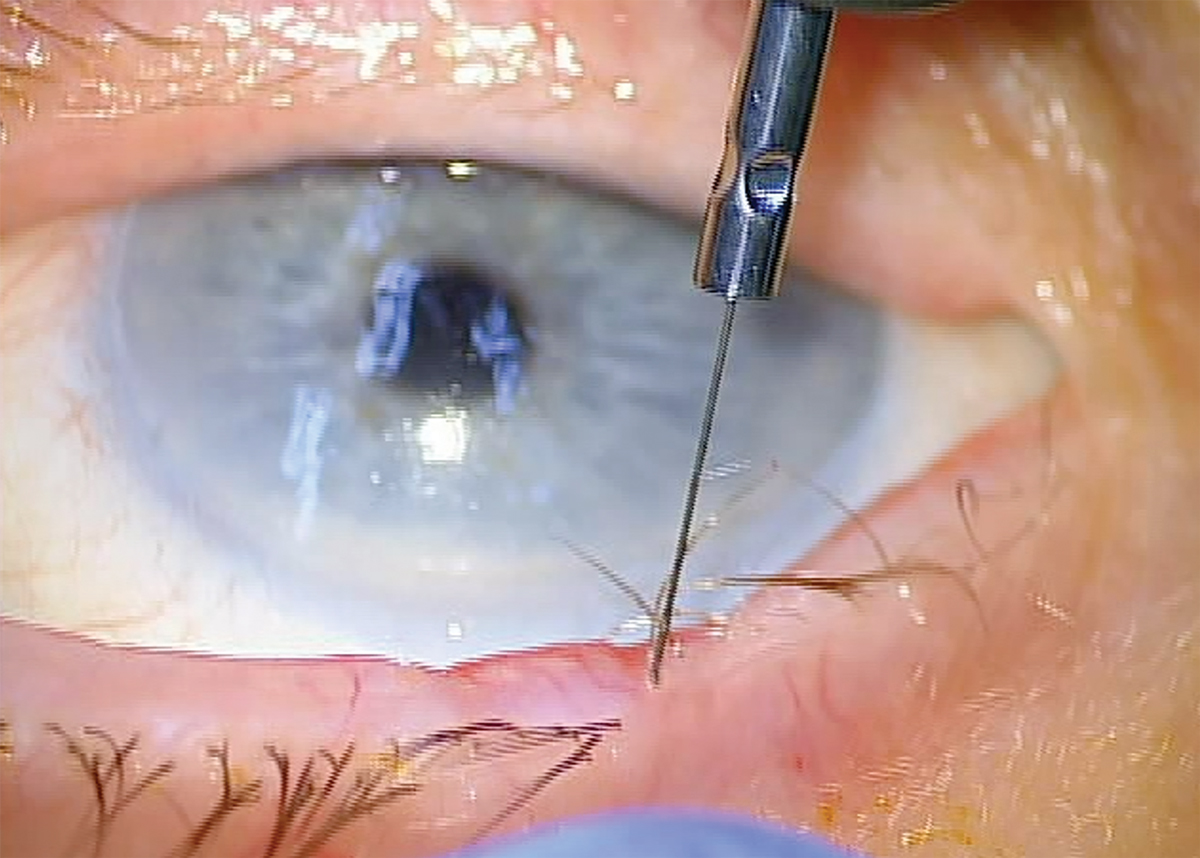
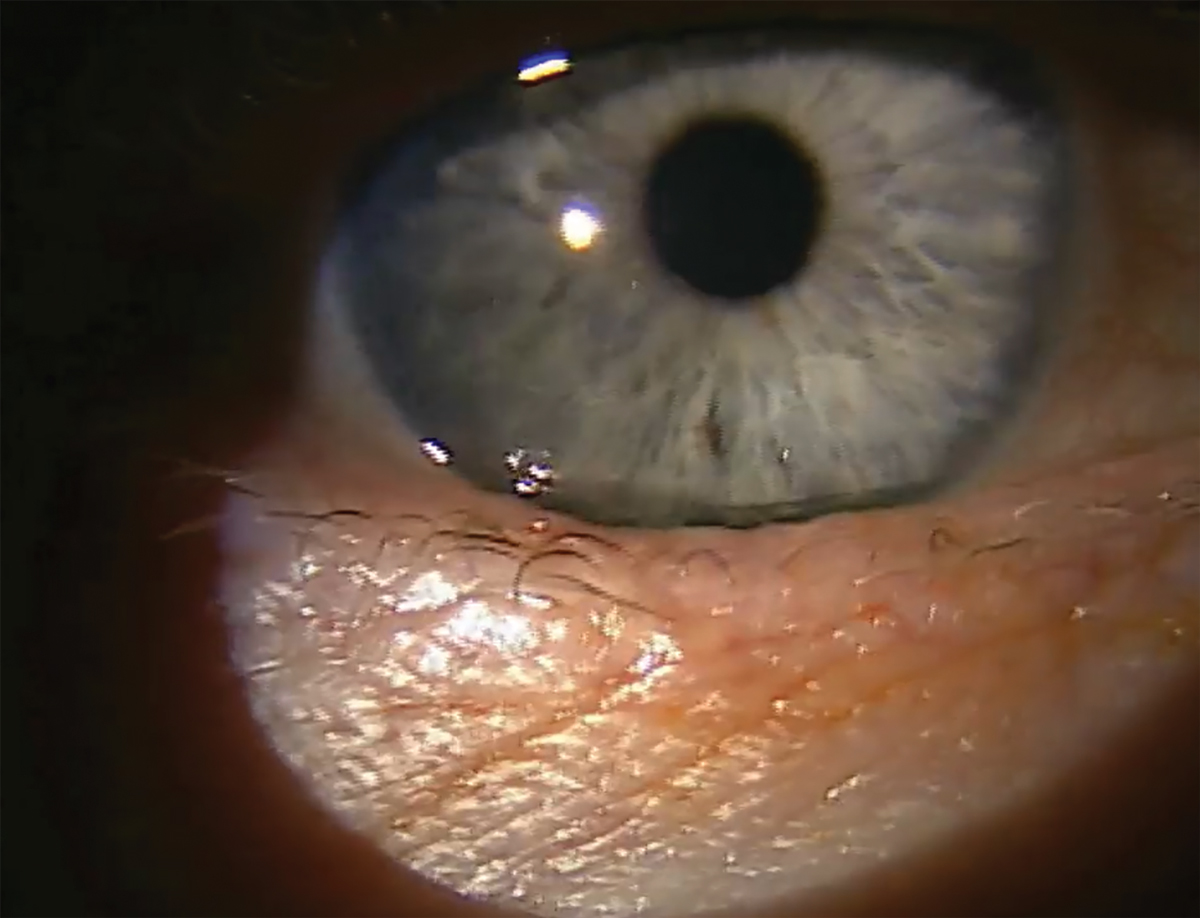
The ideal endpoint of radiofrequency ablation of lashes is the lash being coagulated and sticking to the electrode. Click image to enlarge. |
13. Align the micro-insulated needle electrode or fine wire electrode down the shaft of the offending eyelash. The electrode should be inserted adjacent to the eyelash to the base of the follicle. This is approximately 2.4mm for the upper eyelid and 1.4mm for the lower eyelid. It is important to match the orientation of the electrode with the orientation of the offending eyelash.
14. Once in the hair follicle, the foot pedal is pressed for one to two seconds on setting 3 (coagulate/hemostasis) at a starting power of 3. A successful removal is when the eyelash comes out on the electrode. Multiple attempts are often required to successfully get the eyelash to stick to the electrode. If multiple attempts are required, it is encouraged to go around the lash when treating. For example, if the electrode is on the right side of the eyelash and multiple attempts fail to coagulate the follicle and remove the lash, subsequent attempts should position the electrode to the left side of the lash, on the top or on the bottom of it.
Radiofrequency settings. Setting 3: coagulate/hemostasis (10% cutting, 90% coagulation)— power 3 to 6.
15. If the eyelash is not sticking to the electrode after several attempts (five to 10), use forceps to gently pull on the eyelash to see if it removes with ease. If a tugging sensation is felt, coagulate again. No resistance should be felt upon removing the eyelash, indicating a successful ablation.
16. Repeat this process until all offending eyelashes have been removed.
17. Apply erythromycin 0.5% ophthalmic ointment to the eyelid margin.
18. No bandages or patches are needed at the conclusion of the procedure.
19. Measure blood pressure and pulse.
Follow-up
An operative report should be completed after every procedure that describes the steps taken to perform the procedure. Blood pressure and pulse are measured after the procedure due to the injection of epinephrine. An antibiotic ointment is used three times a day for seven days to prevent infection and aid healing. A one- to two-month follow-up appointment is typically booked to assess treatment success and to determine whether re-treatment is needed. The patient is advised to return sooner if signs and symptoms of infection arise.
Redness and bruising are temporary during the postoperative phase and will self-resolve once completely healed. Bruising may occur from injection of anesthesia and typically resolves within a week. Infection is rare and prevented with the antibiotic ointment that is prescribed postoperatively. If infection were to occur, use topical or oral antibiotics.
Eyelid complications including notching and scarring are more common with electrocautery than radiofrequency, but can occur if the depth of the electrode is excessive or if the radiofrequency power setting is too high.2 Due to the proximity of the eyelid margin to the globe, accidental injury to the eye may occur.5 One study found a complication rate of 14% after radiofrequency ablation.6 These complications included eyelid notching, madarosis, progressive entropion and hyperpigmentation. Another study, using a smaller group size, found faint hypopigmentation in 8.3% of patients and eyelid notching in 16.6% of patients.7
 |
|
The ideal endpoint of radiofrequency ablation of lashes is the lash being coagulated and sticking to the electrode. Click image to enlarge. |
Takeaways
Trichiasis ablation with radiofrequency is a more long-lasting treatment option to offer patients over eyelash epilation. Recurrence of eyelash growth is possible with radiofrequency ablation; however, the procedure can be repeated two to three months after initial treatment with success. This simple and effective in-office, surgical procedure can yield tremendous improvement in patient symptoms.
Dr. Patel is an assistant professor at the Oklahoma College of Optometry (NSUOCO). She completed a primary care residency at NSUOCO specializing in ocular disease and advanced procedures. Dr. Patel is a diplomate of the American Board of Optometry and a fellow of the American Academy of Optometry. She has no financial disclosures.
Dr. Lighthizer is the associate dean, director of continuing education and chief of specialty care clinics at the NSU Oklahoma College of Optometry. He is a founding member and immediate past president of the Intrepid Eye Society. Dr. Lighthizer’s full disclosure list can be found here.
1. Dutton JJ and Waldrop TG. Atlas of Oculoplastic and Orbital Surgery. 2nd ed. Wolters Kluwer; 2019. 2. Fowler G. Pfenninger and Fowler’s Procedures for Primary Care. Elsevier; 2020. 3. Bowling B and Kanski JJ. Kanski’s Clinical Ophthalmology: A Systematic Approach. 8th ed. Elsevier; 2016: 135-6. 4. Onofrey BE, Skorin L, Jr. and Holdeman NR. Ocular Therapeutics Handbook: A Clinical Manual. 3rd ed. Lippincott Williams & Wilkins; 2012. 5. Hainer BL. Electrosurgery for the skin. Am Fam Physician. 2002;66(7):1259-66. 6. Al-Fakey YH. Treatment of trichiasis with high-frequency radiowave electrosurgery. Saudi J Ophthalmol. 2006;20(2):119-23. 7. Sakarya Y, Sakarya R and Yildirim A. Electrolysis treatment of trichiasis by using ultra-fine needle. Eur J Ophthalmol. 2010;20(4):664-8. |