2024 Pharma IssueIn the March issue of Review of Optometry, experts provide exciting updates on incoming treatments and prescribing protocols. Check out the other article featured in this issue:
|
As scope of practice continues to expand in optometry, oral pharmaceuticals prescription has become a mainstay in many practices in the treatment and management of a variety of ocular and periocular conditions. Optometrists don’t hesitate when prescribing topical medications, but when it comes to oral pharmaceuticals we often hesitate or at least think twice about what we are going to prescribe. Let’s review the “dos and don’ts” of the most prescribed oral pharmaceuticals that optometrists use in the management of ocular and periocular conditions.
Case History
Patients present to our offices with urgent or emergent eye care concerns, and the first step of the management plan is a thorough case history. Review the patient’s chief concern and the various signs and symptoms, and then think about possible etiologies and treatment options for the patient. A thorough medical history will include important considerations such as allergies to medications, age, sex, pregnancy, current health conditions and medication use.
Be aware of possible cross-sensitivity with other medications (e.g., someone with a penicillin allergy may also be sensitive to certain cephalosporins).1 It is important to ask the patient whether they had experienced any reactions with any medications. Patients often misinterpret experiencing a side effect of a medication as being allergic to it. For example, nausea and diarrhea after taking amoxicillin is not an allergic response but a well-known side effect of that medication. The CDC reported in 2017 that 10% of the population reports being allergic to penicillins, but less than 1% are truly allergic upon testing.2 Side effects often take several days to develop, while a person who is allergic will often develop symptoms shortly after administration of the medication.
 |
|
Fig. 1. Mild cases of dacryocystitis in children often self-resolve, while more severe forms should be managed with antibiotic therapy, dose-adjusting based upon weight. Photo: Joseph W. Sowka, OD. Click image to enlarge. |
Signs and symptoms of an allergic response to a medication include the development of skin rashes/hives, blistering of mucous membranes and/or breathing issues.3 Educate all patients whenever prescribed an oral medication (especially sulfa-based antibiotics) that, if they develop any rashes/hives, blisters or breathing issues, they should stop the medication immediately and contact the clinic. Also, teach them about potential side effects of the medication like nausea, diarrhea, paresthesia, sedation, etc.
Any medical conditions the patient may be experiencing that affect the kidneys and liver should be carefully explored (e.g., diabetes and chronic kidney disease or alcoholism and liver function). Dosing may have to be altered or the medication entirely avoided, depending on the patient’s liver and kidney functioning.4
In addition, the medications the patient takes to manage their medical conditions have the potential to either cross-react or alter the patient’s “normal” physiology, making the patient have an adverse reaction even in typical or normal dosing. For example, the monoamine oxidase inhibitors (MAOI) were one of the very first antidepressant medications, but they have largely been replaced by newer drugs due to several dietary restrictions, side effects and safety concerns. Prescribing tramadol for a patient’s corneal abrasion would be contraindicated in a patient taking an MAOI because it could lead to serotonin syndrome, which can develop within minutes to hours in a patient leading to possible hallucinations, tachycardia, abnormal eye movements, loss of coordination and other effects.5
Allergies vs. Side EffectsAllergic responses typically occur within an hour of taking a medication. Symptoms include red and unusually warm skin, blotchy rash, hives (nettle rash), Itching, swollen mucous membranes, fluid retention in the body’s tissues (edema). Severe allergic responses can also include anaphylaxis and lead to breathing difficulties, confusion and drowsiness or even cardiac arrest.1 Side effects of medications can happen at any time and typically include upset stomach, diarrhea (loose stools), dry mouth, drowsiness, flushing/sweating and changes in mood or behavior.2
|
Systemic Antibiotics
Infections involving the periocular soft tissues (e.g., preseptal cellulitis, dacryocystitis and internal hordeola) require the systemic antibiotics (Figure 1). When prescribing these, consider that the overuse or the inappropriate prescribing of antibiotics can lead to the development of resistance. When deciding which antimicrobial agent to prescribe, the clinician should consider the spectrum of action, the route of administration and the suspected site of infection. In addition, patient factors such as allergy status, age, renal and liver function and weight must be considered.6
The antibiotic is often chosen based on the knowledge of what is the most common pathogen found in that tissue or site. For example, the most common bacteria associated with periocular tissue infections is Staphylococcus aureus, a gram-positive bacterium. Additional consideration must be given to patients who may have an increased risk of their infection being secondary to methicillin-resistant Staphylococcus aureus (MRSA) (Figure 2). The clinician will need to consider covering for a MRSA infection if the patient reports prolonged hospitalization, intensive care admission, recent hospitalization, recent antibiotic use, previous MRSA infection, invasive procedures, HIV infection, admission to nursing homes, open wounds and hemodialysis.8
The cell wall synthesis inhibitor group of antibiotics is one of the most prescribed for soft tissue infections, as they have good soft tissue penetration and good activity against gram-positive bacteria. The cell wall synthesis inhibitor antibiotics include the ß-lactam antibiotics, vancomycin and bacitracin.9 The ß-lactam group of antibiotics includes penicillins (e.g., amoxicillin) and cephalosporins (e.g., cephalexin).10 There are penicillinase-resistant antibiotics that have a natural resistance to penicillinase such as dicloxacillin, oxacillin and nafcillin.11
Penicillin. Note that penicillin allergies, or hypersensitivity, are one of the more common drug allergies that patients report. Approximately 10% of the population reports an allergy to penicillins; however, in reality only about 1% of the population has a true penicillin allergy. Even if an individual had a penicillin allergy as a child, approximately 80% of patients often lose their sensitivity after 10 years.2
The CDC and other organizations that monitor antibiotic use and resistance strongly recommend all healthcare professionals take a proactive role to delabel penicillin allergy in patients who report a penicillin allergy. To do so, initiate skin testing and review the patients’ medical history in relation to what reaction the patient had to the penicillin. Skin testing is recommended for those individuals who report an anaphylactic response to a penicillin. For most other patients with histories of penicillin allergy that are vague or benign, prescribing without preceding skin testing is the preferred approach.
Another side effect of the penicillin group of antibiotics is antibiotic associated-diarrhea (AAD). Amoxicillin is most associated with AAD. The administration of systemic antibiotics can kill not only pathogens also disrupt the natural symbiotic flora of the gut resulting in gastrointestinal upset (GI), nausea and diarrhea. AAD occurs in patients from the start of the treatment and can last up to two months after the end of the treatment. Taking antibiotics with food and recommending taking probiotics approximately two hours after the antibiotic can mitigate the symptoms of AAD by helping normalize an unbalanced flora.12
Cephalosporins. These are one of the most prescribed antibiotics due to their wide clinical utility and good tolerability with a low chance for allergic response. As the cephalosporins are part of the ß-lactam group like penicillin, patients with supposed penicillin allergies are treated similarly because of concern of cross-reactivity and an allergic response. The cross-reactivity of cephalosporins with penicillin allergy was originally thought to be approximately 10%, but more recent research indicates that it is likely closer to about 1% to 4%.10 Cross-reactivity allergic response also depends on the generation of cephalosporin prescribed with the most likely chance of response occurring with the first-generation cephalosporins like Keflex (cephalexin, Advancis Pharmaceutical). There are five generations of cephalosporins, with an increase in gram-negative coverage as you go up in generation.1 Third-generation cephalosporins are the mainstay treatment for patients with gonorrhea.
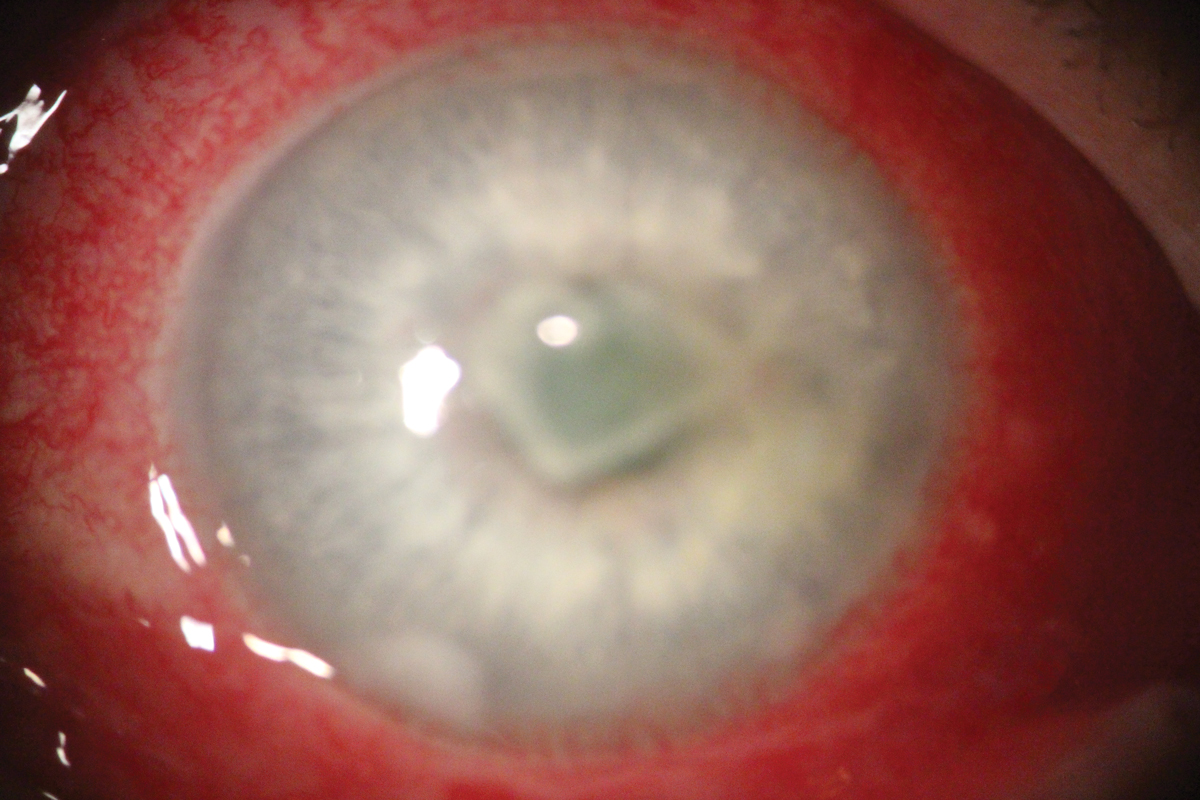 |
| Fig. 2. Non-MRSA Staph. aureus corneal ulcer. Click image to enlarge. |
Macrolides. If patients have a penicillin allergy and you are hesitant in prescribing a cephalosporin, the macrolide group of antibiotics are a good alternative. Azithromycin, clarithromycin and erythromycin are prescribed to treat a variety of conditions including pneumonia, sinusitis, pharyngitis, tonsillitis and uncomplicated skin infections. Like any other antibiotic, macrolides carry a certain level of risk from typical adverse effects like nausea, vomiting, abdominal pain and diarrhea.13
As of 2021, azithromycin is no longer considered the mainstay treatment for chlamydia and gonorrhea. It is used in patients who are either allergic to or unable to take doxycycline (100 mg BID for seven days) or a ceftriaxone injection (500mg or 1g if there is ocular involvement).14
Traditional management of meibomian gland dysfunction (MGD) has included the use of oral doxycycline. Two recent studies have demonstrated that azithromycin is equally if not more effective than doxycycline without the side effects of doxycycline (GI upset, photosensitivity). The first study compared a 30-day treatment with doxycycline vs. a five-day course of azithromycin, and both were found to improve signs and symptoms of MGD.15 The second study demonstrated that a three-week course of weekly oral azithromycin was equivalent to a six-week course of oral doxycycline in treating moderate to severe MGD (Figure 3).16 Azithromycin should be used with caution in patients who have a history of or taking medications for arrythmias (specifically, QT interval prolongation).17
Tetracyclines. These have traditionally been used in the treatment of rickettsial infections, Lyme disease, acne and chlamydial infections.18 Several conditions have an indication for doxycycline treatment, including ocular/acne rosacea, MGD, recurrent corneal erosion (RCE) and chronic corneal wounds. These medications have been shown to inhibit the production of pro-inflammatory mediators, thus reducing the production of inflammatory compounds, such as cytokines and chemokines, and matrix-metalloproteineases (MMP). Doxycycline and minocycline are the most frequently prescribed members of the tetracycline group and are the most used tetracyclines in eye care.19
Tetracyclines can commonly cause GI distress, including abdominal discomfort, epigastric pain, nausea, vomiting and anorexia. Some patients experience photosensitivity, which can manifest as a red rash or skin blistering.18 The tetracyclines, in particular minocycline, have been linked to an increased chance of patient’s developing idiopathic intracranial hypertension (IIH).20 Despite traditional wisdom, recent studies have demonstrated that there is a very low chance of teeth discoloration in children taking doxycycline. Recommendations have changed stating that doxycycline, but not other tetracyclines, can be used for short courses (<21 days) regardless of age. Clinicians should be aware of this because doxycycline use may extend to disease states apart from tick-borne illnesses in pediatric patients.21 Remember the common dos and don’ts for taking doxycycline: avoid calcium and antacids, do not take before lying down, recommend sun protection and take with food.18
Trimethoprim/sulfamethoxazole (TMP-SMX) is available as a generic and branded (Bactrim, Roche or Septra, Pfizer). It is an antimicrobial used to treat and prevent many bacterial infections. It is probably most familiar to clinicians for being prescribed for patients with MRSA skin infection or suspects. The treatment of Staphylococcus aureus infections, including MRSA, is a non–FDA approved use of this medication. It comes in two dosages: standard strength, at 400mg of sulfamethoxazole and 80mg of trimethoprim dosed two pills every 12 hours, and double strength, which is 800mg/160mg dosed one pill every 12 hours and is more commonly used. Other treatments for MRSA include doxycycline (100mg BID for seven days), minocycline (200mg orally once, then 100mg orally twice daily) or clindamycin (450mg orally three times daily).22
TMP-SMX has many potential adverse side effects and interactions with other drugs to be aware of. The most common/serious possible adverse reactions are the development of Clostridium difficile colitis, hyperkalemia (possible development of kidney stones), hypoglycemia, photosensitivity and—probably one of the most severe adverse events—bone marrow suppression, if combined with other folate-inhibiting medications such as methotrexate (first-line treatment for many rheumatological conditions). It is a sulfa-based drug, so the patient cannot have a sulfa allergy. Also, recommend drinking lots of fluids (to help kidney function) as well as sun protection and ensure the patient is not taking any other folate-inhibiting medications.23
 |
|
Fig. 3. A three-week course of weekly oral azithromycin was deemed equivalent to a six-week course of oral doxycycline in treating moderate to severe MGD in a recent study. Click image to enlarge. |
Antiviral Therapy
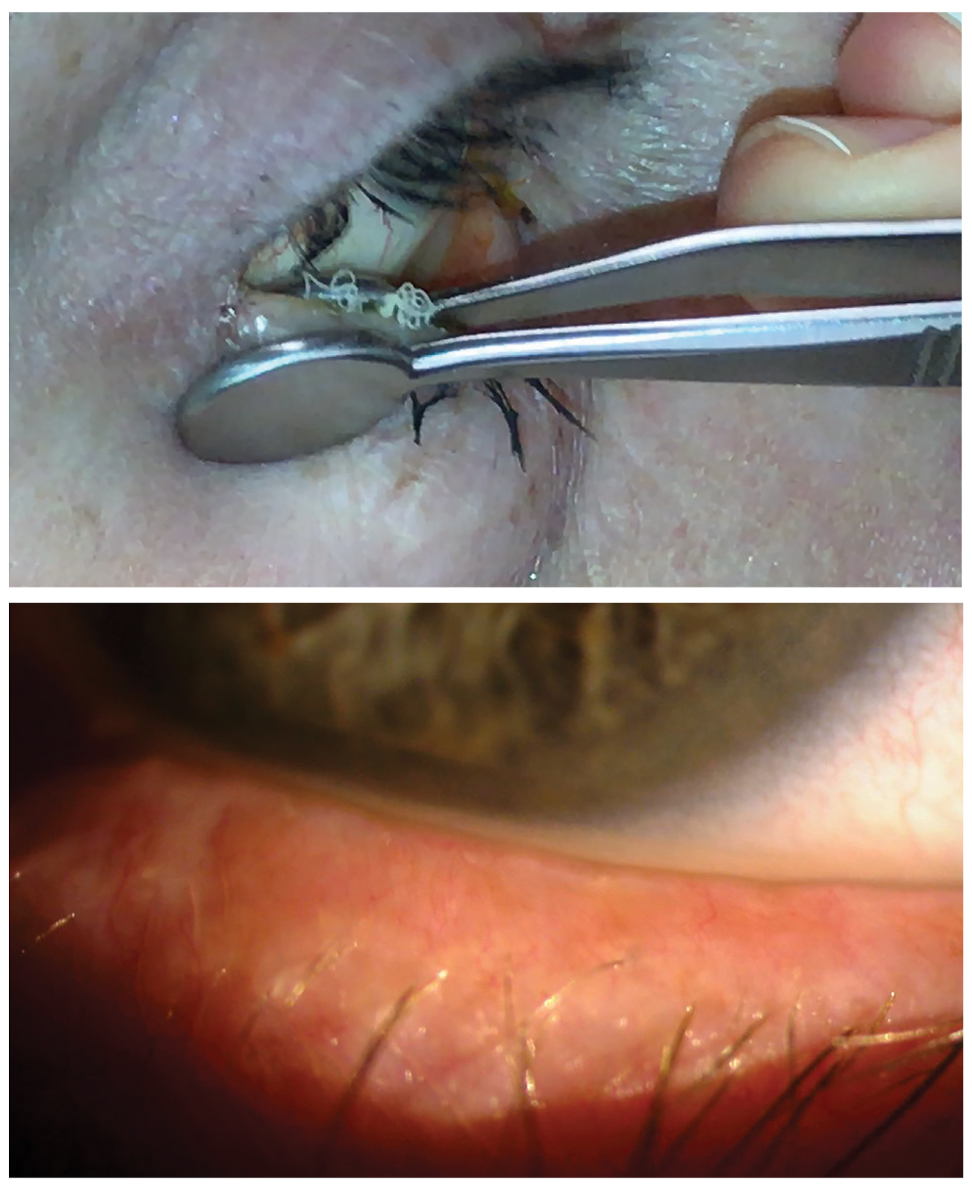
Herpes simplex virus (HSV) keratitis and herpes zoster ophthalmicus (HZO) are two of the more painful and potentially sight-threatening infections that an optometrist can encounter in practice (Figure 4).
HZO occurs due to the reactivation of the latent varicella-zoster virus (VZV). VZV primary infection most commonly occurs in childhood and is spread by airborne, droplet or direct transmission. HZO is secondary to the reactivation of the VZV typically decades after the initial infection. Ocular manifestations can include conjunctivitis, uveitis, episcleritis, keratitis and retinitis and is considered an ophthalmic emergency because of the potential of severe vision loss.
Antiviral therapy is required for treating these two. There are three oral antivirals available for treatment. For HSV keratitis, oral acyclovir (400mg five times daily) or valacyclovir (500mg three times daily) are both effective. Valacyclovir has the advantage of less frequent dosing and higher bioavailability but may be more expensive than acyclovir. Famciclovir (250mg to 500mg three times daily) may be used for allergic patients or resistant disease.24 For HZO, acyclovir 800mg five times daily, valacyclovir 1000mg three times daily or famciclovir 500mg three times daily is recommended, and treatment is preferable within 72 hours of the outbreak.25
Acyclovir is remarkably well tolerated in most patients, though there are a couple of important considerations. Acute renal failure, produced by the precipitation of relatively insoluble acyclovir crystals in the renal tubules, is an occasional complication of intravenous therapy. Neurologic toxicity is a rare, reported condition that has included agitation, tremors, delirium, hallucinations and myoclonus typically occurring in patients with underlying renal failure.26 Valacyclovir and famciclovir have similar side effects.
Vaccination with Shingrix (GlaxoSmithKline) is indicated to reduce the risk of developing herpes zoster and postherpetic neuralgia in those at increased risk for disease (immunocompetent individuals ≥50 years of age, immunocompromised patients ≥19 years of age at increased risk of herpes zoster). Shingrix requires two doses administered intramuscularly for protection with the second dose being administered two to six months after the first.27
Oral Steroids
With the ever-expanding scope of practice for optometrists, the ability to prescribe oral steroids is now available in 44 states. Their potential for serious patient side effects cannot be overstated. Oral steroids work to control the body’s immune response and help prevent damaging consequences such as scarring and neovascularization. Steroids are best suited for controlling acute inflammation whereas chronic inflammation is likely better managed with immunomodulators.28
Oral steroids (glucocorticoids) are used to treat a variety of anterior and posterior ocular conditions including non-infectious uveitis, periocular dermatitis, Bell’s palsy, scleritis, thyroid eye disease, arteritic anterior ischemic optic neuropathy (giant cell) and optic neuritis.29 The most common steroids prescribed by optometry are prednisone and methylprednisone.30
Dosing for oral corticosteroids is dependent on the patient’s clinical presentation and course, but prednisone is commonly used at a dose of 0.5mg/kg to 1.5mg/kg daily. Typically, an initial dose of 20mg to 40mg of prednisone per day may be reasonable for mild inflammation; 40mg to 60mg per day might be considered for severe inflammation; and doses as high as 80mg to 100mg daily (or more) may be necessary for resistant inflammation 48 hours after the initial dose.31
A convenient way to prescribe an oral steroid for a patient is by using a Medrol Dosepak (Pfizer), as it delivers a higher dose of steroids on day one with a built-in tapering schedule that is easy to follow. Several retrospective reviews have shown long-term glucocorticoid use, even in low doses, is a significant independent predictor of numerous adverse effects and that the risk is both dose- and duration-dependent. The daily dose of glucocorticoid is a key factor in toxicity, with higher doses carrying a higher risk of adverse effects. Longer duration of glucocorticoid therapy, and therefore higher cumulative doses, are associated with adverse effects.
 |
|
Fig. 4. HSV with classic dendritic epithelial involvement. Click image to enlarge. |
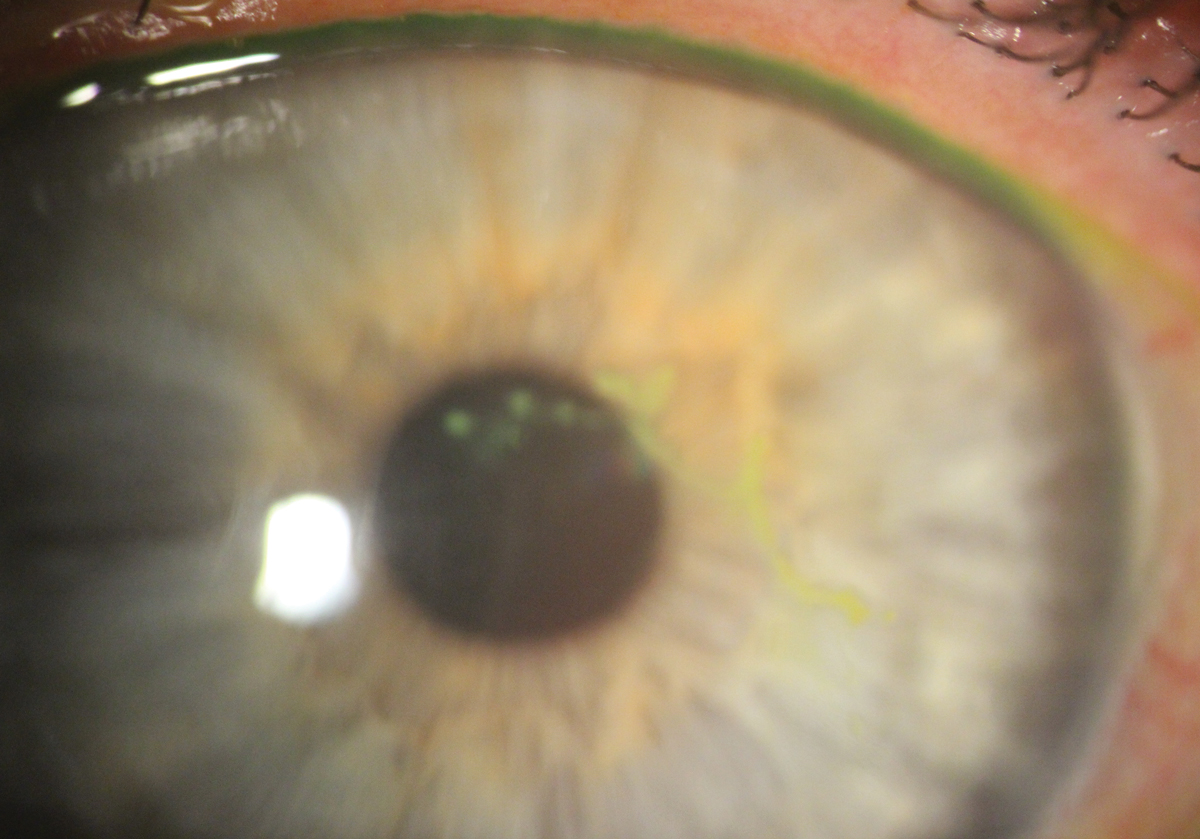
However, even shorter-term glucocorticoid use may also be associated with serious adverse effects, particularly with higher doses.33 There are many potential adverse side effects of glucocorticoid treatment and with removal from treatment. Some hyperglycemia (patients with diabetes will have elevated blood glucose levels), weight gain, thinning of the skin, fluid retention, hypertension, arrythmias, GI complications, osteoporosis, sleep disorders, psychoses, mood disorders and well-known ophthalmic complications including cataracts, increased IOP, central serous chorioretinopathy and exophthalmos (Figure 5).32
Pain Management
A common reason for patients to present to their eyecare professional is secondary eye pain. Nociceptive pain is often adequately managed with topical agents, whereas neuropathic pain is better managed with oral pain relievers and other adjunctive therapies.33
When considering oral pain management, the clinician has the choice of recommending either non-narcotic (e.g., acetaminophen, nonsteroidal anti-inflammatory drugs; NSAIDs, gabapentin) and narcotic agents (e.g., codeine, hydrocodone, oxycodone). In 1986 the World Health Organization proposed an analgesic ladder for pain management. The “original” analgesic ladder included:
• First step. Mild pain: non-opioid analgesics such as NSAIDs or acetaminophen with or without adjuvants.
• Second step. Moderate pain: weak opioids (hydrocodone, codeine, tramadol) with or without non-opioid analgesics and with or without adjuvants.
• Third step. Severe and persistent pain: potent opioids (morphine, methadone, fentanyl, oxycodone, buprenorphine, tapentadol, hydromorphone, oxymorphone) with or without non-opioid analgesics and with or without adjuvants.34
The latest update to the analgesic ladder keeps the basic tenets of the original, with some additions:
- Oral dosing of drugs whenever possible (as opposed to intravenous, rectal, etc.).
- Around-the-clock rather than on-demand administration. The prescription must follow the pharmacokinetic characteristics of the drugs.
- Analgesics must be prescribed according to pain intensity as evaluated by a pain severity scale. For this purpose, a clinical examination must combine with an adequate pain assessment.
- Individualized therapy (including dosing) addresses the concerns of the patient. This method presupposes that there is no standardized dosage in pain treatment. This is probably the biggest challenge in pain medicine, as the dosology must be continuously adapted to the patient, balancing desired effects and possible side effects.
- Proper medication adherence, as any dosing alterations can lead to pain recurrence.35
When considering pain management, make sure you know the underlying cause for the pain. Over-the-counter (OTC) non-narcotics are recommended unless they will not adequately manage the patient’s pain over a 24-hour time period. These are indicated for patients with mild to moderate pain, while narcotic medications should only be considered for severe pain that is not able to be managed by other means and for the minimal time possible.35
Acetaminophen is one of the most widely used non-opioid analgesics and antipyretic agents used to treat pain and fever. Often, they are lumped into the same group as NSAIDs, but they lack the anti-inflammatory effects of the latter.36
- Regular strength: 325mg and is dosed at two tablets every four to six hours and not to exceed 10 pills in 24 hours (max 3250mg/day).
- Extra strength: 500mg and dosed two caplets every six hours, not to exceed six caplets in 24 hours (max 3000mg/day).
- Eight-hour relief: 650mg in each bi-layer and dosed at two bi-layer tablets every eight hours, not to exceed six bi-layer tablets in 24 hours (3900mg/day).
Patients can experience a variety of adverse side effects with the most serious being hepatotoxicity. Due to patients potentially taking multiple products that contain acetaminophen, the FDA limited the amount of acetaminophen that can be found in a prescription product to 325mg (regular strength tablet). Other reactions that patients can have are skin rashes secondary to hypersensitivity and hematological/metabolic issues, though these are uncommon.36,37
NSAIDs are FDA-approved for use as antipyretic, anti-inflammatory and analgesic agents. The main mechanism of action of NSAIDs is the inhibition of the enzyme cyclooxygenase (COX). Non-selective NSAIDs have more potential to affect the GI mucosa and result in GI upset and even development of gastric ulcers, whereas the COX-2 selective NSAIDs that are more selective for inflammatory processes have less potential for GI disorders while still providing pain-reducing and anti-inflammatory properties.38
The most recommended OTC NSAIDs and their dosing are:
- Ibuprofen: 200mg tablets, one to two tablets every four to six hours while symptoms persist. The daily limit for ibuprofen is 1200mg.
- Aspirin regular strength: 325mg tablets, one to two tablets every four hours or three tablets every six hours. The daily limit for aspirin is 4000mg.
- Naproxen sodium: 220mg tablets, one to two tablets every eight to 12 hours. The daily limit for naproxen sodium is 660mg.38
For patients who have mild to moderate pain, a good option for controlling their pain is the alternation of acetaminophen and ibuprofen. The most common “algorithm” is alternating two pills of 325mg acetaminophen followed two hours later be two pills of 200mg ibuprofen and continuing until the pain has subsided. By alternating these medications every two hours, the patient will not exceed the typical dosing regimen of each of the mediations individually which is every four hours. The analgesic action of acetaminophen and ibuprofen is limited by a ceiling effect when an increase in dose produces only a minor increment in effect and increases the chance of toxicity.39
With the current opioid epidemic, clinicians are looking for ways to treat acute pain reliably without having to always default to an opioid. Several studies have demonstrated that a patient taking 1000mg of acetaminophen and 400mg of ibuprofen at the same time is equivalent to prescribing an opioid.40,41
Prescriptions NSAIDs most used in optometric practice include:
- Indomethacin: available in 25mg, 50mg and 75mg capsules. Indicated for treatment of inflammatory conditions like scleritis; however, it is not commonly used as a pain medication, as patients do not like the side effects of the medication.
- Ketoprofen: available in 50mg and 75mg immediate release and 200mg extended release. Dosing can be 50mg orally four times a day or 75mg orally three times a day with maximum dose: 300mg/day. For extended release: 200mg orally once a day with maximum dose: 200mg/day.
- Celebrex (celecoxib, Pfizer) is available in 50mg, 100mg, 200mg and 400mg. Dosing is typically 200mg per day unless for acute pain, where it can be up to 400mg/day.42
NSAIDs have well-known adverse effects affecting the gastric mucosa, renal system, cardiovascular system, hepatic system and hematologic system. Gastric issues include GI upset, nausea and diarrhea with the most serious complication is the development of peptic ulcers. In order to prevent these problems, the patient should either be put on a proton pump inhibitor (e.g., omeprazole) or switched to a COX-2 selective NSAID. NSAIDs interfere with normal prostaglandin production which is crucial for kidney hemodynamics.
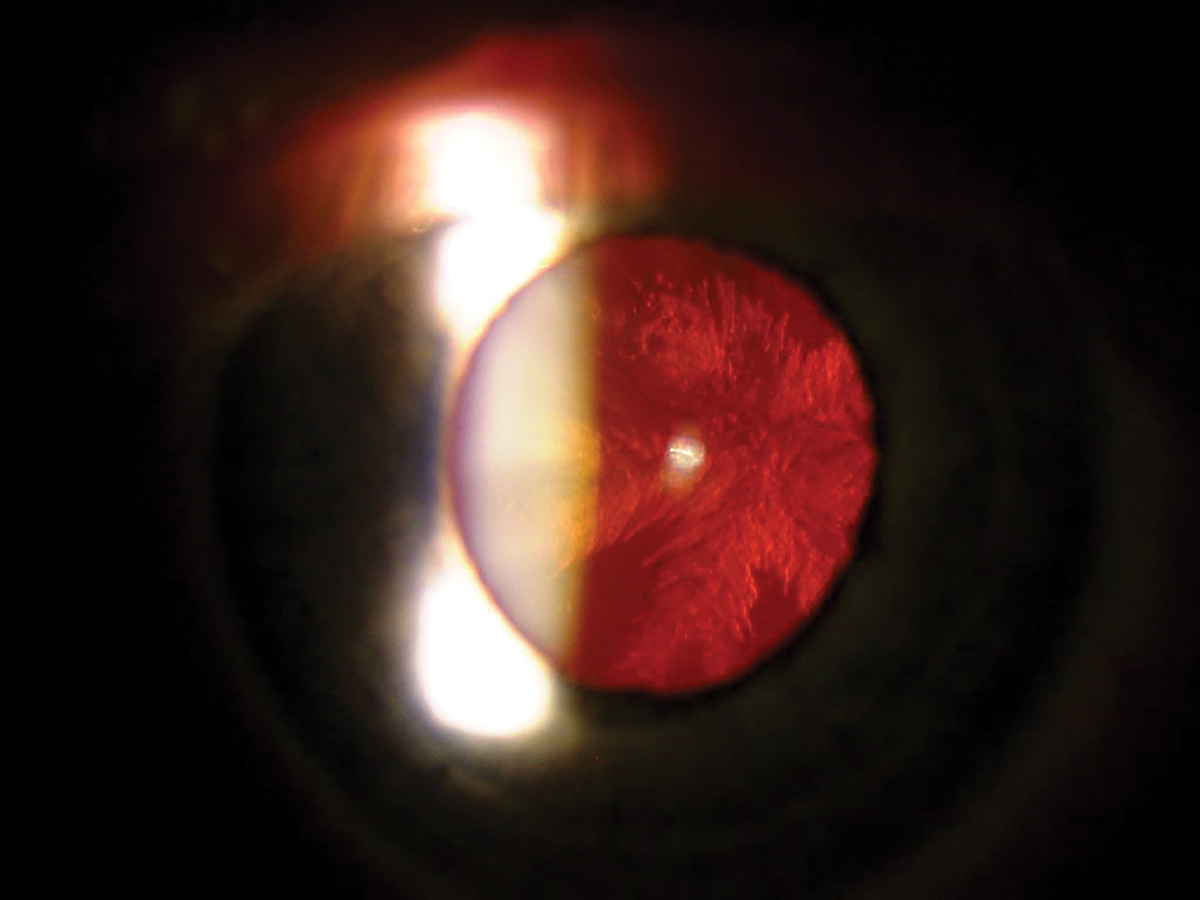 |
Fig. 5. Posterior subcapsular cataract on retroillumination. Click image to enlarge. |
NSAIDs can also interfere with patients’ blood pressure medications—especially diuretics. Patients who are on the maximum daily dose of NSAIDs for more than a couple of weeks can have decreased activity of their blood pressure medications. NSAIDs have been linked to increased chance of cardiovascular complications including myocardial infarction, thromboembolic events and atrial fibrillation. Diclofenac has been reported to be the one most linked to these complications. Hematological adverse effects are also possible especially with the non-specific NSAIDs, which can inhibit platelet aggregation but generally only affect those patients with pre-existing peptic ulcers or bleeding disorders.38
Gabapentin (Neurontin, Pfizer) is an anticonvulsive drug with FDA approval for post-herpetic neuralgia, adjunctive therapy for partial seizure and restless leg syndrome. It is used off-label for neuropathic pain, fibromyalgia, bipolar disorder, diabetic neuropathy pain, PTSD and a variety of other conditions. Herpes zoster pain and post-herpetic neuralgia (PHN) is the most likely condition where an optometrist would consider prescribing gabapentin.
Gabapentin at the federal level is not listed as a controlled drug, is considered a non-addictive medication and is considered by the CDC a substitute for opiates for chronic pain. However, there are growing concerns about its potential for misuse. Several states have moved gabapentin to a schedule V drug. A benefit of gabapentin use is its relatively mild side-effect profile. The most common side effects are fatigue, dizziness and headache but can increase to euphoria when combined with an opioid.
Initial treatment with gabapentin is usually started with one dose of 300mg/day in the evening and later increases the frequency to three times a day and dosage up to 1800mg/day. The effects are apparent in the first week of treatment but sometimes take about a month for significant improvement. Taper the dose over more than seven days to discontinue the medication.43 Both gabapentinoids (i.e., gabapentin and pregabalin) and tricyclic antidepressants (TCAs) have been found to be effective and generally well tolerated for PHN.43 Pregabalin (Lyrica, Pfizer) can also be used for patients with PHN.
Takeaways
There are many cases in which using oral medications strengthens patient care. To ensure care is maintained along the process, check in with your patient and discuss any anticipated effects and what the patient should do if those occur. Education regarding drug choice and treatment initiation, being up-to-date on legislative changes to controlled substances and monitoring an individual patient’s use will be the best way to meet a patient’s needs.
Dr. Lonsberry is a professor of optometry at Pacific University College of Optometry. His financial disclosures include roles at Dompe, Sun Pharmaceuticals and Thea Pharmaceuticals.
Dr. Ibach works at Vance Thompson Vision in Sioux Falls, SD. There, he is the residency co-coordinator. His financial disclosures include roles at Alcon, Allergan, Avellino, Bausch + Lomb, Dompe, Equinox, Glaukos, Heru, Kala, New World Medical, Ocular Therapeutix, Ocuphire, Sight Sciences, Sun Pharmaceuticals, Thea Pharmaceuticals, Viatris and Zeiss.
1. Chaudhry SB, Veve MP, Wagner JL. Cephalosporins: a focus on side chains and β-lactam cross-reactivity. Pharmacy (Basel). 2019;7(3):103. 2. National Center for Emerging and Zoonotic Infectious Diseases. Is it really a penicillin allergy? Division of Healthcare Quality Promotion. stacks.cdc.gov/view/cdc/82752. October 31, 2017. Accessed January 15, 2024. 3. Khan DA, Banerji A, Blumenthal KG, et al. Drug allergy: a 2022 practice parameter update. J Allergy Clin Immunol. 2022;150(6):1333-93. 4. Garza AZ, Park SB, Kocz R. Drug elimination. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. www.ncbi.nlm.nih.gov/books/NBK547662/. Last updated July 4, 2023. Accessed January 15, 2024. 5. Sub Laban T, Saadabadi A. Monoamine Oxidase Inhibitors (MAOI) In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. www.ncbi.nlm.nih.gov/books/NBK539848/. July 17, 2023. Accessed January 15, 2024. 6. Edwards F, MacGowan A, Macnaughton E. Antimicrobial therapy: principles of use. Medicine (Abingdon). 2021;49(10):624-31. 7. Mohammed AA, Ali MM, Zenebe MH. Bacterial etiology of ocular and periocular infections, antimicrobial susceptibility profile and associated factors among patients attending eye unit of Shashemene comprehensive specialized hospital, Shashemene, Ethiopia. BMC Ophthalmol. 2020;20(1):124. 8. Siddiqui AH, Koirala J. Methicillin-Resistant Staphylococcus aureus. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. www.ncbi.nlm.nih.gov/books/NBK482221/. Last updated April 2, 2023. Accessed January 15, 2024. 9. Sarkar P, Yarlagadda V, Ghosh C, Haldar J. A review on cell wall synthesis inhibitors with an emphasis on glycopeptide antibiotics. Medchemcomm. 2017;8(3):516-33. 10. Pandey N, Cascella M. Beta-Lactam Antibiotics. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. www.ncbi.nlm.nih.gov/books/NBK545311/. Last updated June 4, 2023. Accessed January 15, 2024. 11. Penicllins (2nd generation) In: LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases. www.ncbi.nlm.nih.gov/books/NBK548033/. Last updated October 20, 2020. Accessed January 15, 2024. 12. Kopacz K, Phadtare S. Probiotics for the prevention of antibiotic-associated diarrhea. Healthcare (Basel). 2022;10(8):1450. 13. Patel PH, Hashmi MF. Macrolides. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. www.ncbi.nlm.nih.gov/books/NBK551495/. Last updated May 16, 2024. Accessed January 15, 2024. 14. Workowski KA, Bachmann LH, Chan PA, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021;70(4):1-187. 15. Kashkouli MB, Fazel AJ, Kiavash V, et al. Oral azithromycin vs. doxycycline in meibomian gland dysfunction: a randomised double-masked open-label clinical trial. Br J Ophthalmol. 2015;99(2):199-204. 16. Upaphong P, Tangmonkongvoragul C, Phinyo P. Pulsed oral azithromycin vs. six-week oral doxycycline for moderate to severe meibomian gland dysfunction: a randomized clinical trial. JAMA Ophthalmol. 2023;141(5):423-9. 17. Graziani, Amy. Azithromycin and clarithromycin. UpToDate. Hooper, David (Ed). Wolters Kluwer. Last updated July 12, 2022. Accessed February 11, 2024. 18. Shutter MC, Akhondi H. Tetracycline. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. www.ncbi.nlm.nih.gov/books/NBK549905/. Last updated June 5, 2023. Accessed January 15, 2024. 19. Brunton LB, Lazo JS, Parker KL (eds.). Goodman & Gilman’s The Pharmacological Basis of Therapeutics, 11th ed. Section VII. Chemotherapy of Microbial Diseases, Chapter 55. Protein Synthesis Inhibitors and Miscellaneous Antibacterial Agents. New York: McGraw-Hill; 2005. 20. Passi SF, Butcher R, Orme DR, et al. Increased incidence of pseudotumor cerebri syndrome among users of tetracycline antibiotics. J Neuroophthalmol. 2022;42(3):323-7. 21. Stultz JS, Eiland LS. Doxycycline and tooth discoloration in children: changing of recommendations based on evidence of safety. Ann Pharmacother. 2019;53(11):1162-6. 22. Lowy F. Methicillin-resistant Staphylococcus aureus (MRSA) in adults: Treatment of skin and soft tissue infections. In: UpToDate, Spelman, Denis (Ed), Wolters Kluwer. Last updated November 29, 2023. Accessed February 11, 2024. 23. Trimethoprim-sulfamethoxazole (co-trimoxazole): Drug information. In: UptoDate, Wolters Kluwer. Accessed December 28, 2023. 24. Sugar A. Herpes simplex keratitis. In: UpToDate, Jacobs, Deborah and Hirsch, Martin (Ed), Wolters Kluwer. Accessed December 28, 2023. 25. Albrecht MA. Herpes zoster treatment. In: UpToDate, Hirsch, Martin and Schmader, Kenneth (Ed), Wolters Kluwer. Accessed December 28, 2023. 26. Zachary KC. Acyclovir: an overview. In: UpToDate, Hirsch, Martin (Ed), Wolters Kluwer. Accessed on December 28, 2023. 27. Albrecht MA, Levin MJ. Vaccination for prevention of shingles (herpes zoster) In: UpToDate, Hirsch, Martin (Ed), Wolters Kluwer. AccessedDecember 28, 2023. 28. Bartlett JD, Jaanus KE. Clinical Ocular Pharmacology. Butterworth-Heinemann. 2008. 29. Fung AT, Tran T, Lim LL, et al. Local delivery of corticosteroids in clinical ophthalmology: a review. Clin Exp Ophthalmol. 2020;48(3):366-401. 30. Burress J, Turner M. Know the ins and outs of oral steroids. Rev Optom. 2023;160(3):50-4. 31. Dinh R and Do BK. Steroids options for treatment of uveitis. Retinal Physician. 2023;20:32-6. 32. Saag K, Furst D. Major adverse effects of systemic glucocorticoids. In: UpToDate, Hirsch, Martin (Ed), Wolters Kluwer. Accessed on December 28, 2023. 33. Rusciano D, Bagnoli P, Gallar J, Galor A. Editorial: eye pain: etiology and therapeutic approaches. Front Pharmacol. 2022;13:914809. 34.Ventafridda V, Saita L, Ripamonti C, De Conno F. WHO guidelines for the use of analgesics in cancer pain. Int J Tissue React. 1985;7(1):93-6. 35. Anekar AA, Hendrix JM, Cascella M. WHO analgesic ladder. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. www.ncbi.nlm.nih.gov/books/NBK554435/. Last updated April 23, 2023. Accessed February 11, 2024. 36. Gerriets V, Anderson J, Nappe TM. Acetaminophen. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. www.ncbi.nlm.nih.gov/books/NBK482369/. Last updated June 20, 2023. Accessed February 11, 2024. 37. Agrawal S, Khazaeni B. Acetaminophen toxicity. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. www.ncbi.nlm.nih.gov/books/NBK441917/. Last updated June 9, 2023. Accessed February 11, 2024. 38. Ghlichloo I, Gerriets V. Nonsteroidal anti-inflammatory drugs (NSAIDs). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. www.ncbi.nlm.nih.gov/books/NBK547742/. Last updated May 1, 2023. Accessed February 11, 2024. 39. Botting RM. Mechanism of action of acetaminophen: is there a cyclooxygenase 3? Clin Infect Dis. 2000;31 Suppl 5:S202-10. 40. Lyngstad G, Skjelbred P, Swanson DM, Skoglund LA. Analgesic effect of oral paracetamol 1000mg/ibuprofen 400mg, paracetamol 1000mg/codeine 60mg, paracetamol 1000mg/ibuprofen 400mg/codeine 60mg or placebo on acute postoperative pain: a single-dose, randomized and double-blind study. Eur J Clin Pharmacol. 2023;79(8):1131-41. 41. Slawson D. Ibuprofen plus acetaminophen equals opioid plus acetaminophen for acute severe extremity pain. Am Fam Physician. 2018;97(5):348. 42. Schwenk, Eric. Nonopioid pharmacotherapy for acute pain in adults In: UpToDate, Maniker, Robert (Ed), Wolters Kluwer. Accessed December 29, 2023. 43. Yasaei R, Katta S, Saadabadi A. Gabapentin. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. www.ncbi.nlm.nih.gov/books/NBK493228/. Last updated December 19, 2022. Accessed February 11, 2024. |