The historical norm for treating myopic patients has been to alleviate their visual symptoms with spectacles, contact lenses (CLs) or refractive surgery.1,2 While these modalities are highly effective at correcting visual blur, they have little to no impact on reducing the likelihood of developing vision-threatening conditions such as retinal detachments, glaucoma or cataracts, which may develop secondary to myopia later in life.3 Myopic eyes specifically undergo abnormal axial elongation, which results in thinning of the posterior segment.4 This thinning likely increases susceptibility to these ocular pathologies. Reducing a patient’s final refractive error by just 1.00D decreases one’s likelihood of developing maculopathies by about 40%.5 Myopia management, which is the art of reducing myopic progression with pharmacological or optical means, easily has the potential to reduce a treated patient’s refractive error by this amount.6,7 However, it is still too new to fully evaluate this prediction.
Myopia management is quickly becoming recognized as the standard of care across the world, and the need for such treatments is ever more urgent as we approach three billion myopes worldwide.8,9 With myopia being a hot topic in the clinic and laboratory over the past decade, there has been an ever-increasing amount of literature on this topic, which can make clinicians feel overwhelmed and may deter them from breaking into this space, especially if they have not recently completed their clinical training. While admittedly there are a number of nuances to consider, one can easily begin treating this patient demographic after learning a few basic concepts. You can also start to gradually work myopia management into your practice and expand upon your offerings after you have gained some confidence, while simultaneously developing a new source of income.
 |
|
Helping children with contact lens insertion and removal helps ease their anxieties about beginning a myopia intervention. Click image to enlarge. |
Myopia Management Options
One of the most important skills to gain as a new myopia management practitioner is to simply understand your patient’s treatment options. This section will highlight the options currently available in the United States as well as one option only in other markets, which should be available in the US soon. Armed with this knowledge, you can better treat and educate your patients.
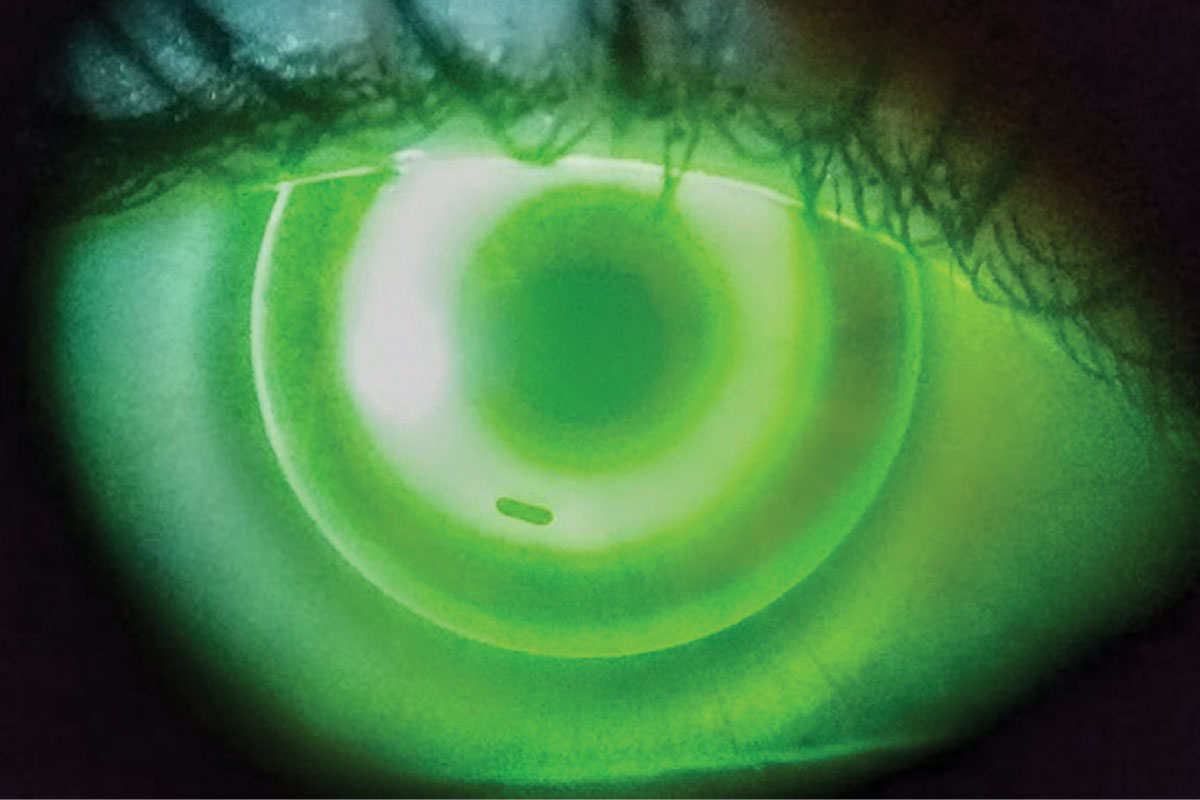
• Low-dose atropine. While the community has long been aware that 1.0% atropine can substantially reduce myopic progression, 1.0% atropine typically results in untenable photophobia and accommodative paralysis, which has hampered its use in the US. Nevertheless, the Atropine for the Treatment of Myopia (ATOM) study has determined that while 1.0% atropine is able to better slow myopic progression than 0.01% concentrations over the first two years of treatment, both can significantly reduce myopic progression.10,11 The ATOM study furthermore determined that 0.01% atropine has a minimal rebound effect after stopping treatment, which was not the case with 1.0% atropine. These data overall suggest that 0.01% atropine is more effective than 1.0% long-term while 0.1% atropine also had minimal side effects.
The Low-concentration Atropine for Myopia Progression (LAMP) study has since determined that 0.025% and 0.05% atropine are more effective at slowing myopic progression than 0.01% atropine. Because of this, many practitioners are now prescribing these higher concentrations.12,13 While we have substantial research supporting the use of low-dose atropine for myopia management, its mechanism is still unclear.
Low-dose atropine may be the easiest treatment modality to incorporate into your practice because it requires minimal additional chair time and equipment. There is no FDA-approved low-dose atropine option in the US market but several are on the horizon, including NVK-002 (Vyluma), which is expecting FDA action imminently for its 0.01% atropine option.
Myopia management practitioners would historically need to use a compounding pharmacy to prescribe low-dose atropine.14 Research suggests that atropine concentrations can vary widely from one compounding pharmacy to another; thus, it is worth asking the pharmacist what the most prescribed concentrations are in your area.14 It may also be worth asking other practitioners in your area about their concentration preferences and why they use the concentration they do. While not scientific, this anecdotal evidence may be useful for determining factors such as if the 0.05% atropine produced by your compounding pharmacy frequently results in side effects or if 0.01% atropine can meaningfully control myopic progression. Concentration variability should be less of an issue with the release of an FDA-approved product.
The community will likewise have data from the Childhood Atropine for Myopia Progression (CHAMP) study, supported by Vyluma, to directly reference.15 This study furthermore suggests that low-dose atropine can be use in patients who are three years and older, showing that it has wonderful versatility in everyday practice.
 |
|
In this well-centered ortho-K lens at initial visit, note the small bubble under the return zone inferiorly. These can be ignored and will generally dissipate as the reshaping occurs in the first 24-hour period. You could also instruct the patient to overfill the lens with a viscous artificial tear prior to insertion. Click image to enlarge. |
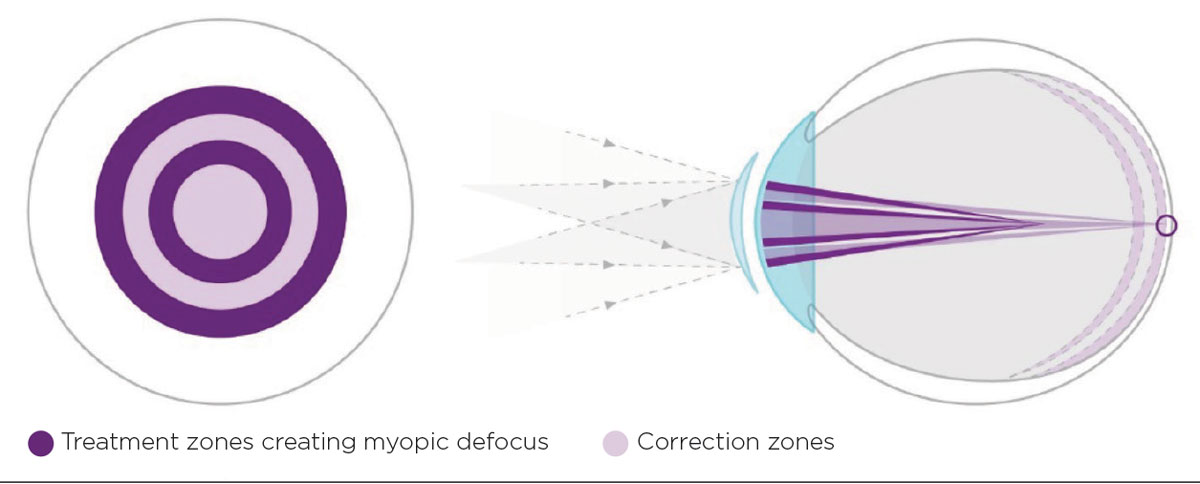
• Multifocal CLs. This option has long been a mainstay of myopia management. Multifocal CLs are theorized to slow myopic progression by reducing peripheral hyperopic defocus.16 Studies from investigators such as Smith et al. have determined specifically that the fovea is not essential for regulating myopic growth.17,18 Related research suggests that providing plus power to the peripheral retina can act as an inhibitor to axial growth, likely by reducing peripheral hyperopic defocus/increasing peripheral myopic defocus.19 The opposite effect can be observed by providing minus power to the peripheral retina. This theory has been supported by the success of center-distance multifocal CLs, which can simultaneously correct foveal refractive error while also reducing peripheral hyperopic defocus.16,20
Although there has been a plethora of multifocal CL studies displaying their effectiveness, the MiSight (daily disposable CLs) and Bifocal Lenses in Nearsighted Kids (BLINK) (monthly CLs) trials may be the best controlled and most important studies in the field.6, 21 Each trial has demonstrated a clinically meaningful reduction in myopic progression. Together, these studies suggest that a +2.00D or +2.50D add is effective at slowing myopic progression, while contact lenses with an add power less than +2.00D may not produce clinically meaningful results.
Multifocal lenses can also be easily incorporated into a typical clinical practice. Some effective ones are already a part of everyday practice for treating presbyopic patients (e.g., VTI NaturalVue Multifocal 1 Day, CooperVision Biofinity D monthly) and myopia management–specific lenses, such as the MiSight, are also now relatively easy to obtain.21 Myopia management soft CLs are fitted and managed just like any other soft lens; therefore, you only need to rely upon your past training to start fitting these.
Nevertheless, one potential nuance with soft CLs is that not all practitioners are comfortable with fitting children in CLs. While this could be new territory for some ODs, an important point to keep in mind is that a practitioner’s judgement can typically be used to accurately determine if young patients will be good CL candidates (e.g., patient is able to easily follow directions and complete a manifest refraction with a phoropter).22 Clinical trials further suggest that patients eight years of age and older are good candidates and that, while kids may require more chair time to fit than adults CL wearers, much of this time is related to application and removal training, which can be delegated.20,22
Other helpful points to remember is that there are no clinically meaningful benefits to ramping up CL wear times over the first week compared to starting CL wear full-time; therefore, children should be given the choice. While fitting them into CLs may feel odd at first, kids who wear soft CLs are statistically less likely to develop an eye infection than young adults.23,24
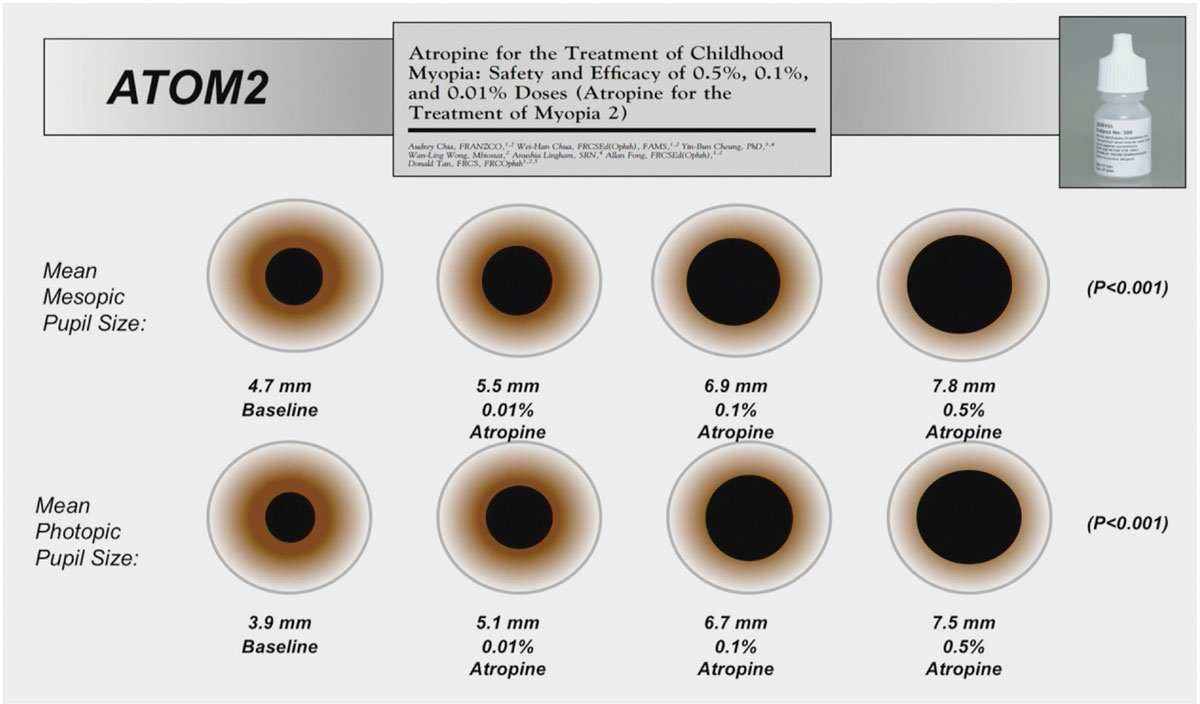 |
• Orthokeratology (ortho-K) lenses. This mainstay of myopia management is theorized to reduce myopic progression by reducing peripheral hyperopic defocus much like multifocal CLs.25 Ortho-K likewise has been clinically shown to reduce myopic progression by a clinically meaningful amount.26,27 Although there have been numerous studies on this topic, two of the most important are from Cho et al., who first demonstrated efficacy with ortho-K compared to spectacles, and later from Walline et al., who corroborated Cho et al.’s results by comparing ortho-K to soft lenses.26,27 Research suggests that ortho-K can successfully be used in patients six years and older, yet practitioner judgement should again be used for patient selection.
Ortho-K may be the most challenging option to incorporate into a typical clinic because it requires a topographer to monitor lens fit, which would be a capital investment into the practice. Practitioners also need to be to highly proficient with advanced rigid lens fitting. Other challenges associated with fitting ortho-K are that it requires substantially more chair time (e.g., several follow-up visits, longer sessions) compared with soft CLs and that overnight wear of any contact lens comes with an increased risk of developing microbial keratitis.28,29 While this increased risk is not dramatically worse than daily wear CLs, it should always be discussed with patients.28,29
With these considerations in mind, it may be best to wait to incorporate ortho-K until after the practice is proficient with prescribing other myopia management treatments unless you are already versed on fitting this modality. Nevertheless, if ortho-K does interest you and you need help getting started, you might want to consider contacting a lab who can assist you. The lab may even be willing to send a representative to your practice to help you see your first few patients.
• Spectacles. Gaining favor outside the US but not yet available here, new spectacle lens designs are also theorized to reduce myopic progression via the reduction of peripheral hyperopic defocus (e.g., Hoya MiyoSmart, Essilor Stellest).30 Nevertheless, there is also a lens design that is aimed at slowing myopic progression by altering contrast sensitivity (SightGlass Vision from CooperVision).31
Research suggests that spectacles are easily accepted by patients and that they are highly effective at reducing myopic progression.30,31 Some of the seminal work on myopia management spectacles comes from Lam et al., with their trial indicating about a 60% reduction in both refractive error and axial length over the first two years of treatment (Hoya, MiyoSmart).30 When spectacles become available in the US, they will likely revolutionize pediatric clinical care. These lenses will specifically not require any additional chair time besides patient education and they will not carry any added risks such as the increased risk of microbial keratitis associated with CLs or the increased risk of photophobia or paralysis of accommodation associated with atropine use.10,29
• Combination treatments. There is a plethora of research evaluating the combination of atropine with orthokeratology, multifocal CLs and/or spectacles.32-37 While studies comparing combined atropine with ortho-K to atropine alone are numerous, data overall may suggest that most of the benefit of combination treatment occurs during the first six months of treatment.32,38,39 It is unclear if there are benefits of combining atropine with other treatment modalities, and because of this, more research is needed on evaluating these combinations, especially with atropine concentrations greater than 0.01%.34
Although some patients may inquire about combination treatments, the current data and additional costs associated with using two myopia management interventions should be fully discussed with patients, and one should be well-versed in this literature before making the decision to advocate for this treatment option. With these points in mind, it may be best to avoid offering combination treatments as a first-line option.
 |
Tracking Myopia Progression
Many practices use advanced technologies to track myopic progression. The simplest and most accurate method is to use a phoropter to complete a manifest refraction. This is likely the best approach for someone new to prescribing myopia management. It could even be applied to managing ortho-K patients who have had their refractive error negated by the treatment. With these patients, one would specifically complete a patient’s ortho-K fit and determine their final refraction in the morning just after adaptation and lens removal. Practitioners can then compare refractive error at subsequent visits at a similar time of day to determine if there has been progression. This approach not only spares additional cost to the practitioner, but it will provide the OD with enough information to determine if there is a clinically meaningful change.
Cycloplegic autorefraction can yield an unbiased measure of refractive error and is more repeatable than a manifest refraction, especially when there is more than one practitioner managing a patient. Since most practices have an autorefractor, this information could be easily collected by a new myopia management practitioner and be used as additional data to inform upon if there has been myopic progression.
After practitioners have had some time to incorporate myopia management, they might want to consider adding an optical biometer to monitor axial length progression. Excessive axial length is the primary factor increasing the likelihood of developing ocular comorbidities. Evaluating axial length is attractive because it can help understand the potential risk of developing these ocular comorbidities (>26mm is considered high myopia).40 This measure could also be helpful because axial length may increase even with a stable refractive error as part of normal emmetropization.41 In fact, young emmetropes typically have an axial length increase of about 0.1mm/year.41 Even further, if axial length has stopped changing, this could be an indicator that a patient’s eye has stopped growing, which could suggest a potential time to taper or stop myopia management treatment.
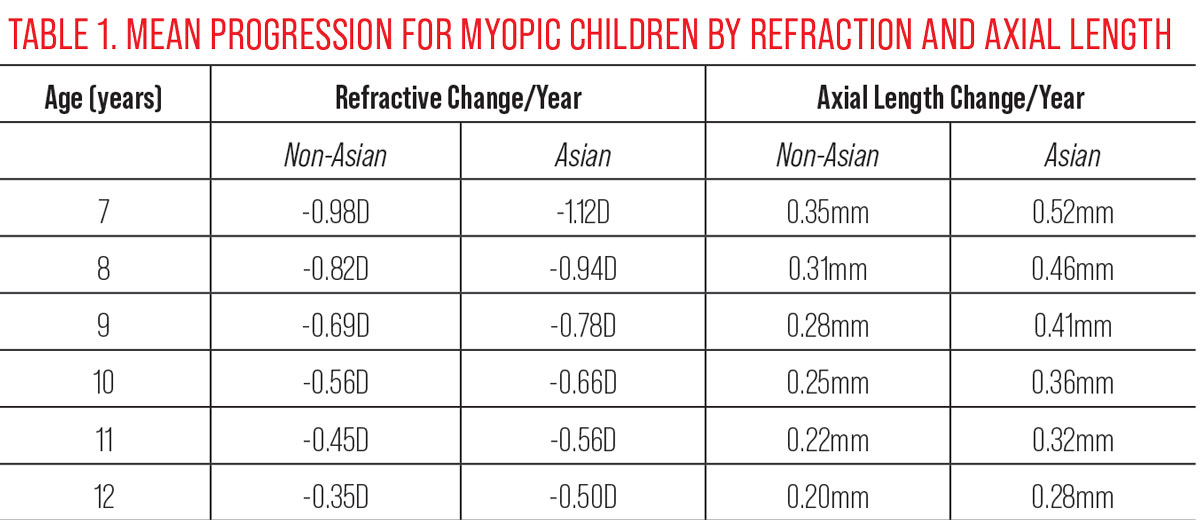
While an optical biometer is nice to have, it is not at all required because change in myopic refractive error and axial length are highly correlated.42 Said another way, one can use refractive error as a surrogate for axial length if an optical biometer is not available. With this in mind, one can determine if a treatment is successfully working by either evaluating refractive error or axial length. The OD could specifically note the patient’s age and compare their refractive error to norms (Table 1) and determine if the treatment is successful (e.g., biometric changes are less than the norms for a given age).43
A final point related to progression comes from the Correction of Myopia Evaluation Trial study, which suggests that virtually all patients who are 10 years old or younger are progressing; thus, there is little need to wait to determine if there is progression to treat in this group if they are already myopic.44
Attracting Patients
While there is scant research on myopia management patient recruitment in an everyday clinic, anecdotally it is common practice to begin by recruiting existing patients from one’s own practice. This approach will not require one to make dramatic practice pattern changes or to spend extra money on recruitment campaigns. Once you are more comfortable with myopia management, you may then want to incorporate this offering on your website along with some patient education on this topic, given that the public may not be fully aware of all the options or benefits.
It is the prescribing clinician’s duty to educate patients and their families about all their treatment options; however, the time burden associated with this can be easily shared with trained staff members. Although it may not be realistic to have all staff within a practice well-versed, one could start by educating yourself and subsequently one additional staff member who has an interest in the topic, so they can help recruit patients and educate them on starting a program.
 |
|
The MiSight 1 Day lens uses what the manufacturer calls “ActivControl technology,” consisting of two discrete rings with a +2.00D add (dark purple) to create myopic defocus on the retina. Click image to enlarge. |
Patient Burden
There is an unfortunate cost and time burden for the patient and their families. While generally not covered by insurance, there are some aspects that may be. For example, a few rare states cover low-dose atropine under Medicaid. Contact lens materials can likely be partially covered with many plans. One additional consideration is that it may be best to break up myopia management fees (e.g., materials, contact lens fitting fee) to allow for lens material benefits to be applied while also avoiding an insurance company from discounting the full management fee down to a contact lens fit fee.
Although there is currently limited insurance coverage for myopia management modalities, this will likely change as more data emerges and more treatments are approved by the FDA. Until that changes, clinicians might want to consider developing an internal patient assistant program to provide an economical myopia management program for those who are unable to afford the full costs of care.
Takeaways
Myopia management has come of age, and it is time for it to be part and parcel with primary care optometry. It does not require you to be a key option leader in the field, have access to every journal article or have extensive capital equipment—it can simply start by taking an interest, making a plan and acting upon it. This simple plan can then grow more elaborate with your skill level and practice while providing your patients with much needed care to improve their visual and ocular health outcomes.
Dr. Pucker is the senior director of clinical and medical sciences at Lexitas Pharma Services. He earned his OD, MS and PhD degrees from The Ohio State University. His independent research and clinical career have focused on dry eye disease, contact lenses and myopia development. Dr. Pucker is a Fellow and Diplomate of the American Academy of Optometry, Fellow of the Scleral Lens Education Society and Fellow of the British Contact Lens Association.
1. Remington LA. Clinical anatomy of the visual system. 2nd ed. Boston: Butterworth-Heinemann; 2005. 2. Javitt JC, Chiang YP. The socioeconomic aspects of laser refractive surgery. Arch Ophthalmol. 1994;112(12):1526-30. 3. Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31(6):622-60. 4. Funata M, Tokoro T. Scleral change in experimentally myopic monkeys. Graefes Arch Clin Exp Ophthalmol. 1990;228(2):174-9. 5. Bullimore MA, Brennan NA. Myopia control: Why each diopter matters. Optom Vis Sci. 2019;96(6):463-5. 6. Chamberlain P, Peixoto-de-Matos SC, Logan NS, et al. A three-year randomized clinical trial of MiSight lenses for myopia control. Optom Vis Sci. 2019;96(8):556-67. 7. Chamberlain P, Bradley A, Arumugam B, et al. Long-term effect of dual-focus contact lenses on myopia progression in children: a six-year multicenter clinical trial. Optom Vis Sci. 2022;99(3):204-12. 8. World Council of Optometry. Resolution: the standard of care for myopia management by optometrists. www.worldcouncilofoptometry.info/resolution-the-standard-of-care-for-myopia-management-by-optometrists. Accessed January 2, 2024. 9. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-42. 10. Chia A, Chua WH, Cheung YB, et al. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1% and 0.01% doses (Atropine for the treatment of Myopia 2). Ophthalmology. 2012;119(2):347-54. 11. Chia A, Chua WH, Wen L, et al. Atropine for the treatment of childhood myopia: changes after stopping atropine 0.01%, 0.1% and 0.5%. Am J Ophthalmol. 2014;157(2):451-7.e1. 12. Yam JC, Jiang Y, Tang SM, et al. Low-concentration atropine for myopia progression (LAMP) study: a randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025% and 0.01% atropine eye drops in myopia control. Ophthalmology. 2019;126(1):113-24. 13. Yam JC, Li FF, Zhang X, et al. Two-year clinical trial of the low-concentration atropine for myopia progression (LAMP) study: phase 2 report. Ophthalmology. 2020;127(7):910-9. 14. Richdale K, Tomiyama ES, Novack GD, Bullimore MA. Compounding of low-concentration atropine for myopia control. Eye Contact Lens. 2022;48(12):489-92. 15. Zadnik K, Schulman E, Flitcroft I, et al. Efficacy and safety of 0.01% and 0.02% atropine for the treatment of pediatric myopia progression over three years: a randomized clinical trial. JAMA Ophthalmol. 2023;141(10):990-9. 16. Berntsen DA, Kramer CE. Peripheral defocus with spherical and multifocal soft contact lenses. Optom Vis Sci. 2013;90(11):1215-24. 17. Smith EL 3rd, Hung LF, Huang J. Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vision Res. 2009;49(19):2386-92. 18. Smith EL 3rd, Ramamirtham R, Qiao-Grider Y, et al. Effects of foveal ablation on emmetropization and form-deprivation myopia. Invest Ophthalmol Vis Sci. 2007;48(9):3914-22. 19. Schaeffel F, Glasser A, Howland HC. Accommodation, refractive error and eye growth in chickens. Vision Res. 1988;28(5):639-57. 20. Walline JJ, Lindsley KB, Vedula SS, et al. Interventions to slow progression of myopia in children. Cochrane Database Syst Rev. 2020;1(1):CD004916. 21. Walline JJ, Walker MK, Mutti DO. Effect of high add power, medium add power or single-vision contact lenses on myopia progression in children: the BLINK randomized clinical trial. JAMA. 2020;324(6):571-80. 22. Walline JJ, Jones LA, Rah MJ, et al. Contact lenses in pediatrics (CLIP) study: chair time and ocular health. Optom Vis Sci. 2007;84(9):896-902. 23. Pucker AD, Steele S, Rueff E, et al. Contact lens adaption in neophytes. Optom Vis Sci. 2021;98(3):266-71. 24. Wagner H, Richdale K, Mitchell GL, et al. Age, behavior, environment and health factors in the soft contact lens risk survey. Optom Vis Sci. 2014;91(3):252-61. 25. Nti AN, Berntsen DA. Optical changes and visual performance with orthokeratology. Clin Exp Optom. 2020;103(1):44-54. 26. Walline JJ, Jones LA, Sinnott LT. Corneal reshaping and myopia progression. Br J Ophthalmol. 2009;93(9):1181-5. 27. Cho P, Cheung SW, Edwards M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res. 2005;30(1):71-80. 28. Bullimore MA, Sinnott LT, Jones-Jordan LA. The risk of microbial keratitis with overnight corneal reshaping lenses. Optom Vis Sci. 2013;90(9):937-44. 29. Stapleton F, Keay L, Edwards K, Holden B. The epidemiology of microbial keratitis with silicone hydrogel contact lenses. Eye Contact Lens. 2013;39(1):79-85. 30. Lam CS, Tang WC, Lee PH, et al. Myopia control effect of defocus incorporated multiple segments (DIMS) spectacle lens in Chinese children: results of a three-year follow-up study. Br J Ophthalmol. 2022;106(8):1110-4. 31. Rappon J, Chung C, Young G, et al. Control of myopia using diffusion optics spectacle lenses: 12-month results of a randomised controlled, efficacy and safety study (CYPRESS). Br J Ophthalmol. 2023;107(11):1709-15. 32. Kinoshita N, Konno Y, Hamada N, et al. Efficacy of combined orthokeratology and 0.01% atropine solution for slowing axial elongation in children with myopia: a two-year randomized trial. Sci Rep. 2020;10(1):12750. 33. Zhao Q, Hao Q. Clinical efficacy of 0.01% atropine in retarding the progression of myopia in children. Int Ophthalmol. 2021;41(3):1011-7. 34. Jones JH, Mutti DO, Jones-Jordan LA, Walline JJ. Effect of combining 0.01% atropine with soft multifocal contact lenses on myopia progression in children. Optom Vis Sci. 2022;99(5):434-42. 35. Erdinest N, London N, Lavy I, et al. Low-concentration atropine monotherapy vs. combined with MiSight 1 Day contact lenses for myopia management. Vision (Basel) 2022;6(4):73. 36. Nucci P, Lembo A, Schiavetti I, et al. A comparison of myopia control in European children and adolescents with defocus incorporated multiple segments (DIMS) spectacles, atropine, and combined DIMS/atropine. PLoS One. 2023;18(2):e0281816. 37. Huang Z, Chen XF, He T, et al. Synergistic effects of defocus-incorporated multiple segments and atropine in slowing the progression of myopia. Sci Rep. 2022;12(1):22311. 38. Yu S, Du L, Ji N, et al. Combination of orthokeratology lens with 0.01% atropine in slowing axial elongation in children with myopia: a randomized double-blinded clinical trial. BMC Ophthalmol. 2022;22(1):438. 39. Tan Q, Ng AL, Cheng GP, et al. Combined 0.01% atropine with orthokeratology in childhood myopia control (AOK) study: a two-year randomized clinical trial. Cont Lens Anterior Eye. 2023;46(1):101723. 40. Ohno-Matsui K, Wu PC, Yamashiro K, et al. IMI pathologic myopia. Invest Ophthalmol Vis Sci. 2021;62(5):5. 41. Chamberlain P, Lazon de la Jara P, Arumugam B, Bullimore MA. Axial length targets for myopia control. Ophthalmic Physiol Opt. 2021;41(3):523-31. 42. Mutti DO, Hayes JR, Mitchell GL, et al. Refractive error, axial length and relative peripheral refractive error before and after the onset of myopia. Invest Ophthalmol Vis Sci. 2007;48:2510-9. 43. Nixon A, Brennan N. Managing Myopia: A Clinical Response to the Growing Epidemic. Johnson & Johnson Vision 2020. April 13, 2021. Accessed January 2, 2024. www.jnjvisionpro.com/education-center/resource-library/managing-myopia-clinical-response-growing-epidemic. 44. Group C. Myopia stabilization and associated factors among participants in the Correction of Myopia Evaluation Trial (COMET). Invest Ophthalmol Vis Sci. 2013;54(13):7871-84. |