|
A 14-year-old girl presented with a complaint of a painful left eye of one day’s duration. The doctor wrote “CL” in the history but nothing about the patient’s past activity the days preceding the pain, the degree of her pain or her contact lens hygiene. The patient’s mother filled out the history form and did not check off that she wore contact lenses. She did check off two boxes of the reason for visiting: “eyes itch” and “eyes water.” There was no box for “eye pain.” There was no mention of red eye. Other health history included an ear infection for which the patient was taking an antibiotic. There was no indication in the history of how long the patient had the ear infection, what antibiotic was prescribed and how long she was taking it.
 |
|
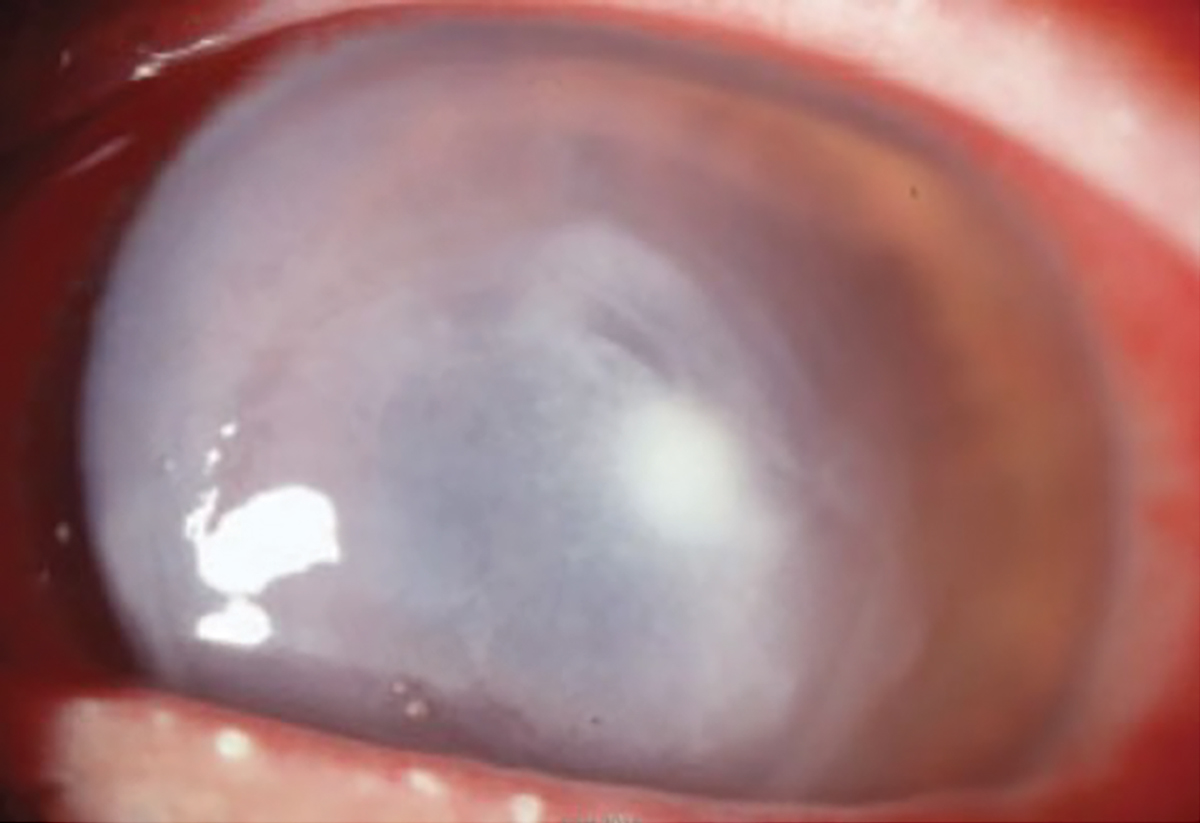
Fig. 1. Pseudomonal ulcer in another patient. Untreated infection causes a gray necrosis that can destroy a cornea in 24 hours. Photo: Scott Hauswirth, OD, and Richard Mangan, OD. Click image to enlarge. |
Clinical Findings
Entering unaided visual acuities were 20/200 OD and 20/400 OS. Pinhole visual acuities were not measured, nor was best-corrected visual acuity (BCVA) measured through a spectacle lens. Anterior segment examination was normal OD. Examination OS revealed grade 2+ conjunctival hyperemia, a central small corneal abrasion that exhibited “+ staining” with fluorescein dye, a deep and quiet anterior chamber and clear lens. The picture the practitioner drew in the record had the central corneal opacity be about 1mm to 2mm in size, but the practitioner did not measure it.
Diagnosis and Follow-Up
The patient was diagnosed with a corneal abrasion and was prescribed erythromycin ointment BID OS. She was also told to “patch as needed” and to discontinue contact lens wear. The patient was told to return the next day.
Her pain worsened, and she went to an emergency room in the middle of the night. She was seen by an emergency room physician. The diagnosis and antibiotic remained unchanged, and the patient was prescribed Voltaren (diclofenac, GlaxoSmithKline) for the eye pain. That next morning, she returned to the doctor’s office and was seen by a second doctor. At this visit, the patient complained of increasing pain, photophobia and tearing. The cornea was now noted for a large 6mm central corneal infiltrate with surrounding haze and 3+ conjunctival injection. The patient was immediately referred to be seen by a cornea specialist the same day.
The cornea specialist obtained a history of “red eye left eye for three days—went to ER, given diclofenac one drop Q6h and erythromycin ung once a day, patient wears contact lenses daily, occasionally sleeps in them” and a history of the ear infection treated with neomycin ear drops, two drops a day, left ear and amoxicillin 875mg PO.” Pinhole visual acuities were 20/40 OD and 20/400 OS. Cornea examination was noted for a 7mm x 6mm large ring ulcer surrounding the pupil with 2+ cells and flare in the anterior chamber (Figure 1).
The cornea specialist performed a corneal scraping for a diagnostic smear. The patient was started on homatropine 5% BID OS, chlorhexidine 0.02% QID OS, polyhexamethylene biguanide (PHMB), an anti-Acanthamoeba medication, 0.02% QID OS, vancomycin 50mg/cc every hour while awake and tobramycin ointment at bedtime. The patient returned the next day feeling much better, reporting no pain and only slight sensitivity to light. The patient’s father forgot to bring in her drops and didn’t know when they were last administered. Examination revealed a 30% enlargement of the infiltrate with 2+ cells/flare and now a 0.5mm hypopyon. Due to the imminent threat of corneal perforation, the patient was referred to an eye hospital for an emergency corneal transplant. Multiple drops of Besivance (besifloxacin, Basuch + Lomb) and gentamicin eye drops were instilled every five minutes in-office, and the patient was told to continue this regimen until she got to the eye hospital.
The patient’s family sought a second opinion from a children’s hospital the same day. On that visit, the history revealed the fact that she had been swimming in the ocean while wearing her contacts. It also included notes about her lens hygiene and wearing schedule. She said that she never slept in her lenses (which differed from what she told the cornea specialist) and that she cleaned them daily with Optifree solution. She also claimed that she changed her lenses at the appropriate times. At this visit, the patient was diagnosed with a contact lens associated corneal ulcer, which was cultured at bedside. The patient was admitted to the hospital due to the intensive treatment regimen. For the first hour, she was treated with fortified vancomycin and PHMB one drop each five minutes apart for the first hour and then chlorhexidine and tobramycin one drop every five minutes for the second hour, then each drop q1h and homatropine BID. A corneal transplant was not recommended. Four days later, the culture came back positive for Pseudomonas aeruginosa. Over the next several weeks, the medications were tapered. Two months later, the patient was left with a central corneal scar in the left eye and corrected to 20/70 VA.
Malpractice Allegation
The first and second eyecare practitioners and the cornea specialist who initially examined the patient were sued for failure to properly diagnose and treat the corneal ulcer that led to vision loss in her left eye. The emergency room doctor and hospital were not named in the suit because there was no eyecare specialist in the ER that night and the patient was seen by a general physician who treated her for pain.
You Be the Judge
In light of the facts presented thus far, consider the following questions:
- Did the first practitioner get enough information in the history and examination to differentiate an abrasion from a central corneal infiltrate/ulcer?
- Was the first practitioner correct in diagnosing a corneal abrasion since the opacity was so small?
- Did the first practitioner consider the grade 2+ conjunctival hyperemia when he diagnosed an abrasion?
- Did the first practitioner deviate from the standard of care in the history, examination and treatment of the patient?
- Did the second practitioner deviate from the standard of care by referring the patient to a cornea specialist?
- Did the cornea specialist deviate from the standard of care by not adequately treating the patient and then recommending a corneal transplant?
 |
|
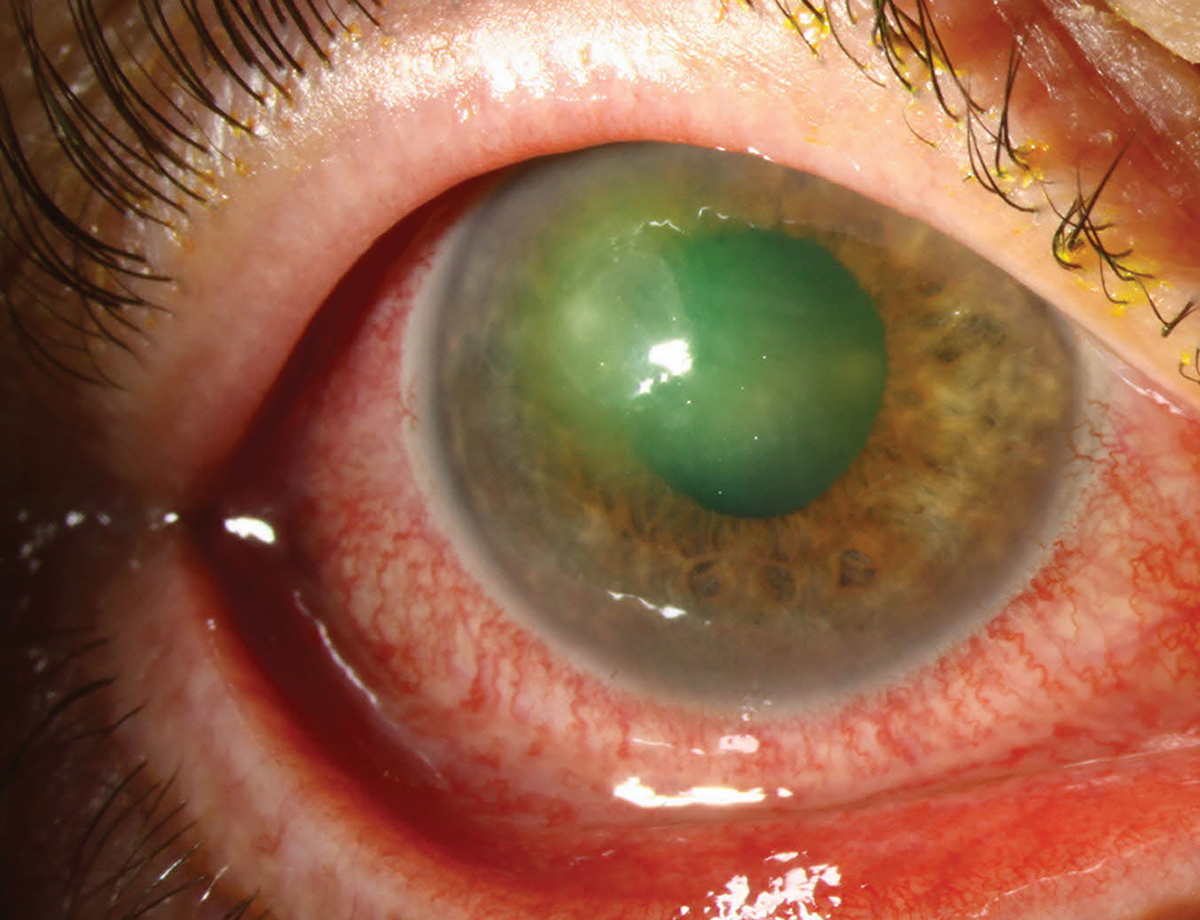
Fig. 2. Early pseudomonal ulcer in another patient. Note the extensive hyperemia and near central location. Photo: University of Iowa. Click image to enlarge. |
Our Opinion
One of us (SB) opines that, based on the history, that this patient rubbed her eyes after swimming in the ocean, and perhaps sand may have embedded under her contact lens and caused an epithelial break. Although Pseudomonas aeruginosa is most common in freshwater and soil, it has been demonstrated to be found in marine habitats.1 Patients who present as such, especially contact lens wearers, must be treated with a strong antibiotic before the organism has a chance to invade a cornea that has an epithelial break.
The first practitioner who examined this patient noted a small abrasion but did not obtain (or record) a history of what the patient was doing that day or the day before. In addition, the BCVA was never determined. A large decrease in the affected eye might have been a red flag for an ulcer, not an abrasion.
The patient should have been asked about the level of pain in her left eye. A more painful eye makes a corneal ulcer more suspect. The first eyecare practitioner did not specify any details about the staining of the lesion. In early ulcers, the dye will seep into the stroma as opposed to remaining on the corneal surface. In suspicious cases like this, the practitioner should have waited a few minutes to see if the dye infiltrated into the stroma. In addition, corneal ulcers are associated with significant conjunctival hyperemia, present in this patient. The patient should have been instructed about what to do if the pain increased over the next few hours instead of being told to just return the next day.
Since the pain increased enough to drive the patient into an emergency room in the middle of the night, the ulcer and the pain obviously increased significantly. It was likely the size of the ulcer in Figure 2 in another patient. Pseudomonas ulcers can be devastating and can destroy a cornea in less than 24 hours.2
The eyecare practitioner also told the patient to “patch as needed.” Patching an abraded cornea in a contact lens patient is contraindicated since bacterial ulcers are more common in contact lens patients, and bacteria can more easily invade an abraded epithelium when patched. Additionally, the antibiotic prescribed (erythromycin ointment) was not strong enough to kill the invading Pseudomonas—erythromycin is bacteriostatic, not bactericidal. A bacteriostatic drug controls bacterial growth but does not kill off all the bacteria. If an ulcer is suspected, the patient should have been treated with a bactericidal antibiotic, like a fluoroquinolone—and aggressively. The patching (if the patient did patch) would have only made matters worse. The patient also reported an ear infection one day after swimming. Pseudomonas is a known cause of “swimmer’s ear.”3
The second eyecare practitioner, who referred the patient immediately to a cornea specialist, was sued but was not culpable since there was a timely referral. The cornea specialist who treated the patient appropriately was sued because the patient got worse under their care. But the patient and her parents were apparently noncompliant with the drops and were unsure if all the drops were being used. Bad patient behavior unfortunately may or may not support a malpractice defense, based on the specific circumstances.
Takeaways
This case highlights the importance of obtaining a thorough history, especially if the patient is a contact lens wearer. It also demonstrates the reason why contact lens patients must be warned not to wear their contact lenses while swimming or in the shower. This can easily be accomplished by providing a handout specifying how to care for and when not to wear contact lenses. This patient was fit for contact lenses in the practice where she first presented. There is no evidence in the records that the patient was ever provided with such a handout or that the patient was verbally told not to wear contact lenses while swimming and showering.
Corneal ulcers are not as common as corneal abrasions. However, there are specific criteria that should alert the practitioner to differentiate a corneal ulcer from a corneal abrasion. Pain, BCVA and conjunctival hyperemia are certainly significant, but a good history can make a huge difference to avoid a huge mistake.
The case was settled for an undisclosed amount
| NOTE: This article is one of a series based on actual lawsuits in which the author served as an expert witness or rendered an expert opinion. These cases are factual, but some details have been altered to preserve confidentiality. The article represents the authors’ opinion of acceptable standards of care and do not give legal or medical advice. Laws, standards and the outcome of cases can vary from place to place. Others’ opinions may differ; we welcome yours. |
Dr. Sherman is a Distinguished Teaching Professor at the SUNY State College of Optometry and editor-in-chief of Retina Revealed at www.retinarevealed.com. During his 52 years at SUNY, Dr. Sherman has published about 750 various manuscripts. He has also served as an expert witness in 400 malpractice cases, approximately equally split between plaintiff and defendant. Dr. Sherman has received support for Retina Revealed from Carl Zeiss Meditec, MacuHealth and Konan.
Dr. Bass is a Distinguished Teaching Professor at the SUNY College of Optometry and is an attending in the Retina Clinic of the University Eye Center. She has served as an expert witness in a significant number of malpractice cases, the majority in support of the defendant. She serves as a consultant for ProQR Therapeutics.
1. Khan NH, Ishii Y, Kimata-Kino N, et al. Isolation of Pseudomonas aeruginosa from open ocean and comparison with freshwater, clinical and animal isolates. Microb Ecol. 2007;3(2)173-8. 2. McElvanny AM. Doxyclycline in the management of Pseudomonas corneal melting: two case reports and a review of the literature. Eye Contact Lens. 2003;29(4)258-61. 3. Maclean K, Njamo FOJP, Serepa-Dlamini MH, et al. Antimicrobial susceptibility profiles among Pseudomonas aeruginosa isolated from professional scuba divers with otitis externa, swimming pools and the ocean at a diving operation in South Africa. Pathogens. 2022;11(1):91. |